Aortic valve sclerosis is a degenerative disease defined as the thickening and calcification of the aortic valve (a trileaflet valve) without obstructing the ventricular outflow. This disease needs prompt medical attention, particularly in the presence of aortic systolic murmur that confirms the possibility of aortic valve sclerosis. However, early diagnosis and treatment are required to avoid progression into aortic valve stenosis. The frequency of the aortic valve sclerosis increases with advancing age. It most commonly affects people aged more than 65 years. 1Prasad Y, Bhalodkar NC. Aortic sclerosis–a marker of coronary atherosclerosis. Clin Cardiol. 2004 Dec;27(12):671-3. doi: 10.1002/clc.4960271202. PMID: 15628107; PMCID: PMC6654225.
Anatomy of an Aortic Valve
There are about four parts of the aorta (ascending aorta, aortic arch, descending aorta (thoracic), and abdominal aorta. The ascending aorta is connected to the left ventricle. Your heart comprises four valves that regulate the outflow of blood, and the aortic valve is one of them.
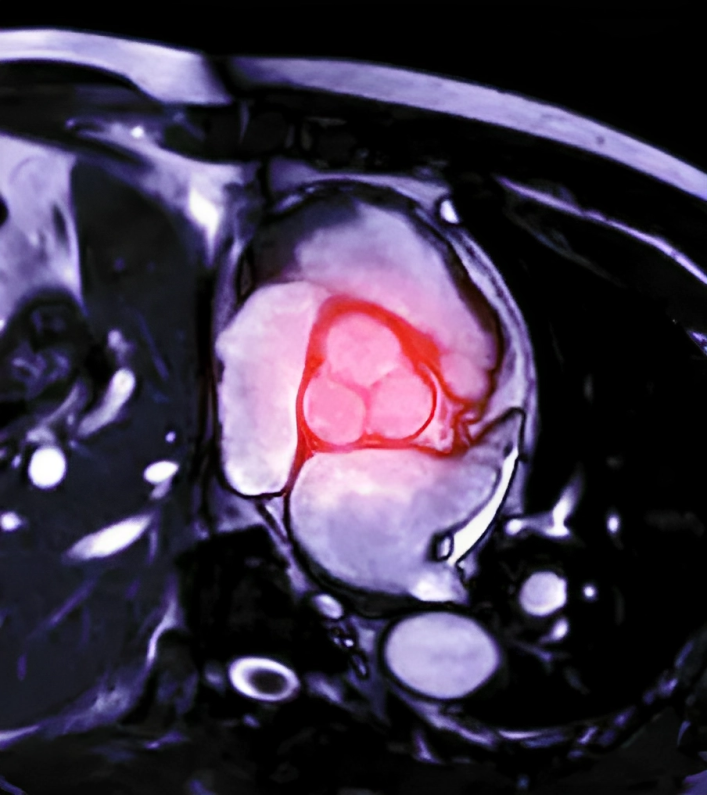
The aortic valve is an opening that allows the outflow of blood towards your body and separates the left ventricle (the main supply of your heart) from the ascending aorta. Additionally, It comprises three leaflets (the right, left, and posterior).
Function of the Aortic Valve
When your heart contracts during systole, the aortic valve opens 3-5 square centimeters, and blood moves into the aorta and circulates to the different parts of the body. During the diastolic or relaxation phase, ventricles are filled with the blood. The aortic valve prevents the backflow of blood from ascending the aorta to the left ventricle during this phase.
Epidemiology
The incidence of aortic valve sclerosis is directly proportional to your age (as age progresses, its frequency increases). According to a cardiovascular health study, aortic sclerosis was 26% in people 65 years of age, 37 % in people aged 75 years, and 48% in people above 85 years of age. The risk of aortic valve sclerosis also increases in patients with other comorbidities like CKD, end-stage renal disease, and other cardiovascular disorders.2Lindroos M, Kupari M, Heikkila J, Tilvis R. Prevalence of aortic valve abnormalities in the elderly: an echocardiographic study of a random population sample. J Am Coll Cardiol 1993; 21: 1220-5
According to a research study, the prevalence of patients with end-stage renal disease was about 55-69 percent. 3Prasad Y, Bhalodkar NC. Aortic sclerosis–a marker of coronary atherosclerosis. Clin Cardiol. 2004 Dec;27(12):671-3. doi: 10.1002/clc.4960271202. PMID: 15628107; PMCID: PMC6654225.4Straumann E, Meyer B, Misteli M, Blumberg A, Jenzer HR. Aortic and mitral valve disease in patients with end-stage renal failure on long-term hemodialysis. Br Heart J 1992; 67: 236-9
Pathophysiology of Aortic Valve Sclerosis
Aortic valve sclerosis is the earliest stage of thickening of the aortic valve in the absence of hemodynamic instability or outflow obstruction. Previously, aortic stenosis and aortic sclerosis were considered progressive degenerative diseases. However, now there is some evidence that shows aortic sclerosis is not a progressive degenerative process; it is a complex and actively regulated process.
The aortic valve comprises a dense layer of collagen fibers with few fibroblast cells (fibrosa). At the same time, the valve of the ventricular side is composed of elastic tissue (ventricularis). Between these two layers (fibrosa and ventricularis), a layer of loose connective tissue (called spongiosa) is present predominantly in the basal 1/3 or the aortic valve. With advancing age, the number of adipose tissue increases in spongiosa, resulting in the thickening of the aortic valve.
Inflammation:
Inflammation plays a key role in the development of aortic sclerosis and aortic stenosis. Inflammatory cytokines are actively involved in the pathogenesis of aortic sclerosis. However, some cells are actively involved in this process. These include the following:
- Macrophages
- T lymphocytes
- Human leukocyte antigen (HLA-DR)
- Interleukin 2
- Mast cells
- Tumor necrosis factors (TNF)
These inflammatory cells induce sclerotic changes inside the valve in the presence of a lesion, resulting in the thickening of the valve.
Lipid Deposition:
Lipid deposition is a prominent feature of calcified aortic valve disease. The accumulation of lipids predominantly occurs in the aortic layer called fibrosa. Damage to endothelial cells allows the deposition of lipids, specifically low-density lipoproteins (LDL) and Lp(a), at the lesion site. Therefore, oxidation of these lipoproteins results in atherosclerotic lesions formation.

Nitric Oxide :
Nitric oxide has multiple functions that are linked with the aortic valve structure and function. It has two important properties: anti-inflammatory and vasodilator. It restricts the calcification process in the aortic valve sclerosis. Comparatively, the dysfunctioning of nitric oxide results in increased calcification, leading to aortic stenosis and aortic sclerosis.
Calcification & Bone Formation:
The calcified aortic valve contains multiple extracellular proteins. These proteins include the following:
- Osteonectin
- Osteopontin
- Bone morphogenetic proteins
- Matrix g-carboxylated glutamine protein
Osteopontin is an extracellular protein that is involved in both the normal calcification process and dystrophic calcification. In aortic valve sclerosis, there is an increase in the level of receptor activator of nuclear factor kappa-B ligand (RANKL), resulting in increased expression of the osteoblasts (bone-forming cells). However, in later stages, evidence of bone formation inside the aortic valve is found.5Nightingale AK, Horowitz JD. Aortic sclerosis: not an innocent murmur but a marker of increased cardiovascular risk. Heart. 2005 Nov;91(11):1389-93. doi: 10.1136/hrt.2004.057117. Epub 2005 Mar 29. PMID: 15797932; PMCID: PMC1769170.
Symptoms of Aortic Valve Sclerosis
Most of the time, aortic sclerosis remains asymptomatic. The characteristic feature of this disease is the presence of an aortic systolic murmur. Doctors can confirm on examination. If it progresses into aortic stenosis, it becomes symptomatic. The following are the symptoms of disease progression:
- Shortness of breath
- Fainting
- Heartbeats become irregular
- Exercise intolerance
- Chest pain, even at rest
What is Aortic Valve Sclerosis Murmur?
Ejection systolic murmur is a characteristic feature of aortic valve sclerosis that can be diagnosed by auscultating the aortic area with a stethoscope. Echocardiography can also detect it. 6Nightingale AK, Horowitz JD. Aortic sclerosis: not an innocent murmur but a marker of increased cardiovascular risk. Heart. 2005 Nov;91(11):1389-93. doi: 10.1136/hrt.2004.057117. Epub 2005 Mar 29. PMID: 15797932; PMCID: PMC1769170.
Causes of Aortic Valve Sclerosis
As we have discussed, lesions in the heart cause atherosclerotic changes at that site. So, there are multiple causes of aortic valve sclerosis. The most common causes include:
- Rheumatic heart disease
- Marfan syndrome
- Rheumatoid arthritis
- Systemic Lupus erythematosus (SLE)
- High blood pressure
- Endocarditis
Risk Factors of Aortic Valve Sclerosis
Some risk factors predispose to aortic valve sclerosis. The incidence of aortic valve sclerosis increases due to the following factors:
- Aging is the most common cause and risk factor
- High blood pressure
- Previous history of heart disease
- Chronic diabetes Mellitus
- Male gender
- Smoking
- High lipoprotein LPa
- High low-density lipoproteins
- End-stage renal disease
Difference Between Aortic Valve Sclerosis and Stenosis
As we have discussed above, aortic valve sclerosis is a clinical condition in which there is a focal thickening of the three leaflets of the aortic valve without complete obstruction of the blood flow. Moreover, the incidence of aortic valve sclerosis increases with age.
Aortic stenosis is a progressive disease in which there is a narrowing of the aortic valve followed by outflow obstruction, and the velocity of flow of blood is less than 2.5 m/s. Moreover, the incidence of aortic stenosis is not directly proportional to the age of the patient. Its prevalence is about 2.9 percent in people with 75 years of age.7Lindroos M, Kupari M, Heikkila J, Tilvis R. Prevalence of aortic valve abnormalities in the elderly: an echocardiographic study of a random population sample. J Am Coll Cardiol 1993; 21: 1220-5
When to see your doctor?
Immediately book your appointment with your cardio physician when you have symptoms like persistent chest pain, loud murmur, and fainting.
Diagnosis Aortic Valve Sclerosis?
Your doctor diagnoses aortic valve sclerosis on the basis of history, physical examination, laboratory investigations/baseline, and radiological investigations.
History:
History is the first step to making a diagnosis. This comprehensive inquiry encompasses various aspects of the patient’s life and health. It begins with the basics, such as biodata and weight, providing essential demographic information. Subsequently, the focus shifts to specific symptoms, including chest pain, palpitations, fainting episodes, headaches, and breathing difficulties. These inquiries aim to pinpoint potential indicators of aortic sclerosis.
Further delving into the patient’s medical background unveils any previous illnesses or chronic conditions, shedding light on their medical history. In addition, details about past drug usage are essential to assess any medications that may have contributed to the current condition. A patient’s personal history, including lifestyle factors like smoking and alcohol consumption, is examined, as these habits can significantly impact overall health. Occupational and family histories provide insights into potential environmental and hereditary factors influencing the patient’s health. By methodically addressing each of these historical elements, healthcare providers can establish a solid foundation for diagnosis and treatment planning.
Physical Examination:
After a detailed history, the next step is the complete physical examination that also helps to reach the diagnosis. In physical examination, your doctor will take the following steps:
Inspection
In this step, your doctor will only inspect while he will check for :
- Chest movement
- Any scar marks
- Any visible swelling
- Any visible pulsation
- Any deformity
- Clubbing
- Anemia
- Encouragement of neck veins
Palpation
During the palpation phase of the examination, your doctor will systematically assess your chest for various indicators, which include checking for temperature and tenderness, identifying any swelling or lumps, and examining the apex beat. Additionally, he will also search for signs of edema and perform abdominal palpation to assess for splenomegaly and hepatomegaly, as well as any potential abdominal masses.
Auscultation
In this step, your doctor will auscultate your chest to check :
- Apex beat in normal position or not
- Check for murmur or regurgitation
- Chest auscultation
- Aortic bruit
Laboratory Investigations:
When a suspicious finding arises during history and examination, laboratory investigations become necessary. These investigations encompass:
- Complete blood count (CBC) to check for anemia
- Erythrocyte sedimentation rate (ESR) to check for chronic inflammation of infection
- C reactive protein (CRP) to check for acute infection
- White blood cell count to check for bacterial or viral infections
- Lipid profile
- Serum creatinine
- Renal parameters (RPM)
- LFTs (liver function tests)
- Viral markers
- Cardiac markers (troponin level)
- Lactate dehydrogenase level
Exercise Tolerance Test
It is a type of test in which you are asked to walk on the treadmill or to walk, followed by heart rate monitoring. This test helps to determine whether the symptoms of this disease occur during some physical activity or not.
Electrocardiography (ECG)
This is a first-line investigation for patients who present with chest pain or dyspnea. Your ECG will show the contractility of your heart. It also used to check:
- ST-segment elevation or depression
- T wave reversal
- The presence of pathological q waves
- Ventricular enlargement
Radiological Investigations:
Radiological investigations are required to confirm the diagnosis and to rule out other diseases. These investigations are:
Chest X-ray
Chest X-ray is the first baseline investigation that shows the lungs, the shape and size of the heart, and the position of the trachea.
Echocardiogram
It is a radiological intervention in which your doctor sees the internal structure of your heart. It shows the flow of blood through your heart valves and the shape and size of the valve. Additionally, sometimes, a special type of echocardiogram known as a transesophageal echocardiogram may be used to provide a zoomed structure of the aortic valve. However, in a transesophageal echocardiogram, a flexible ultrasound-guided probe is moved down from the throat to the esophagus and placed near the heart.

Aortic Valve Assessment
Through echocardiography, the aortic valve is assessed on the basis of grades. There are four grades of aortic valve sclerosis. 8Tolstrup K, Crawford MH, Roldan CA (2002) Morphologic characteristics of aortic valve sclerosis by transesophageal echocardiography: importance for the prediction of coronary artery disease. Cardiology 98(3): 154-158. These are
- Grade 0: no thickening of the aortic leaflet is present
- Grade 1: Thickness is less than or equal to 2mm
- Grade 2: thickens between 2-4mm
- Grade 3: thickness is greater than 4mm and less than 6mm
- Grade 4: thickness is greater than 6mm
According to Tolstrup et al., There are about four morphological types of aortic valve sclerosis. These are:
- The sclerosis is localized and non-nodular
- Sclerosis is localized and nodular
- Sclerosis is defuse
- Mixed sclerosis
CT Scan of Heart
In cardiac CT scans, several combined X-rays provide a detailed structure of the heart. This test helps to determine the size of the aorta.
MRI of the Heart
This test uses radio waves and a magnetic field to provide a detailed 3-dimensional image of the heart. It helps to determine the size of the aorta and the severity of the disease.
Other Investigations:
When other diagnostic methods prove inconclusive, doctors may recommend cardiac catheterization, a surgical procedure. During this procedure, a slender and flexible catheter is carefully inserted into the blood vessels, typically in either the wrist or the groin, and it is then guided to the heart. Then, a special dye is injected through the catheter to enhance the visibility of the arteries. Moreover, the pressure inside the heart can also be measured.
How to Treat Aortic Valve Sclerosis?
The treatment approach to this disease is considered to prevent the following:
- Progression of aortic valve sclerosis into aortic valve stenosis
- Adverse outcomes associated with the aortic valve sclerosis
There are some medical and surgical interventions that are used to treat aortic sclerosis.
Medical interventions:
Your cardiologist may advise medications to slow down the progression of the disease. Medical management includes:
- Statins (HMG Co-A inhibitors): Several studies suggest that statins slow down the progression of disease and calcification in the aortic valve.
- Angiotensin-convertase enzyme inhibitors (ACE inhibitors): ACE inhibitors are considered the potential agents that are used to treat aortic sclerosis. However, strict vital monitoring is advised to avoid hypotension9Siddiq, M. Z. (2023, May 23). What is aortic valve sclerosis. https://www.icliniq.com/articles/heart-circulatory-health/aortic-valve-sclerosis
Surgical Approach:
Your doctor may advise surgical treatment if you fail to respond to the medical treatment. Surgical interventions for aortic sclerosis are:
- Balloon valvuloplasty (A procedure in which your cardiologist inserts a catheter to insert a balloon into the aortic valve)
- Aortic valve replacement10NHS. (n.d.). Aortic valve replacement. NHS. https://www.nhs.uk/conditions/aortic-valve-replacement/
- Aortic valve repair
Lifestyle Modifications
In addition to the medical treatment, you can adopt some lifestyle modifications to overcome the disease and its severity. These modifications include:
- Avoid fatty foods
- Get a healthy diet plan from your nutritionist
- Take exercise regularly
- Have good control of your blood pressure
- Limit sugar intake to prevent obesity
- Stop smoking
- Stop drinking alcohol
Conclusion
To conclude, aortic sclerosis is a degenerative disease that occurs due to the thickening and calcification of the aortic valve with advancing age. It can progress to aortic stenosis. It usually remains asymptomatic until you develop aortic stenosis. Ejection systolic murmur is the characteristic feature of aortic stenosis. However, medications like statins, ACE inhibitors, and lifestyle modifications can treat it. In severe cases, the doctor may advise surgical intervention.
Refrences
- 1Prasad Y, Bhalodkar NC. Aortic sclerosis–a marker of coronary atherosclerosis. Clin Cardiol. 2004 Dec;27(12):671-3. doi: 10.1002/clc.4960271202. PMID: 15628107; PMCID: PMC6654225.
- 2Lindroos M, Kupari M, Heikkila J, Tilvis R. Prevalence of aortic valve abnormalities in the elderly: an echocardiographic study of a random population sample. J Am Coll Cardiol 1993; 21: 1220-5
- 3Prasad Y, Bhalodkar NC. Aortic sclerosis–a marker of coronary atherosclerosis. Clin Cardiol. 2004 Dec;27(12):671-3. doi: 10.1002/clc.4960271202. PMID: 15628107; PMCID: PMC6654225.
- 4Straumann E, Meyer B, Misteli M, Blumberg A, Jenzer HR. Aortic and mitral valve disease in patients with end-stage renal failure on long-term hemodialysis. Br Heart J 1992; 67: 236-9
- 5Nightingale AK, Horowitz JD. Aortic sclerosis: not an innocent murmur but a marker of increased cardiovascular risk. Heart. 2005 Nov;91(11):1389-93. doi: 10.1136/hrt.2004.057117. Epub 2005 Mar 29. PMID: 15797932; PMCID: PMC1769170.
- 6Nightingale AK, Horowitz JD. Aortic sclerosis: not an innocent murmur but a marker of increased cardiovascular risk. Heart. 2005 Nov;91(11):1389-93. doi: 10.1136/hrt.2004.057117. Epub 2005 Mar 29. PMID: 15797932; PMCID: PMC1769170.
- 7Lindroos M, Kupari M, Heikkila J, Tilvis R. Prevalence of aortic valve abnormalities in the elderly: an echocardiographic study of a random population sample. J Am Coll Cardiol 1993; 21: 1220-5
- 8Tolstrup K, Crawford MH, Roldan CA (2002) Morphologic characteristics of aortic valve sclerosis by transesophageal echocardiography: importance for the prediction of coronary artery disease. Cardiology 98(3): 154-158.
- 9Siddiq, M. Z. (2023, May 23). What is aortic valve sclerosis. https://www.icliniq.com/articles/heart-circulatory-health/aortic-valve-sclerosis
- 10NHS. (n.d.). Aortic valve replacement. NHS. https://www.nhs.uk/conditions/aortic-valve-replacement/

