Benzodiazepines (BZDs) are some of the most prescribed drug classes worldwide. They are used for the treatment of anxiety, insomnia, seizures, muscle spasms, and alcohol withdrawal, which makes them a staple in emergency and outpatient care. What makes them so effective is their broad range and rapid action. But this accessibility is a problem at the same time.
Benzodiazepines are generally considered safe when used correctly; their mechanism of action, that is, central nervous system (CNS) depression, makes Benzodiazepine overdose a critical public health issue, though. It is a significant contributor to emergency department visits and drug-related mortality.
| General Name | Brand Name |
|---|---|
| Midazolam | Versed |
| Triazolam | Rilamir |
| Alprazolam | Xanax |
| Lorazepam | Ativan |
| Clonazepam | Klonopin |
| Diazepam | Valium |
| Flunitrazepam | Rohypnol |
| Chiordiazepoxide | Librium |
Mechanism of Action of Benzodiazepines
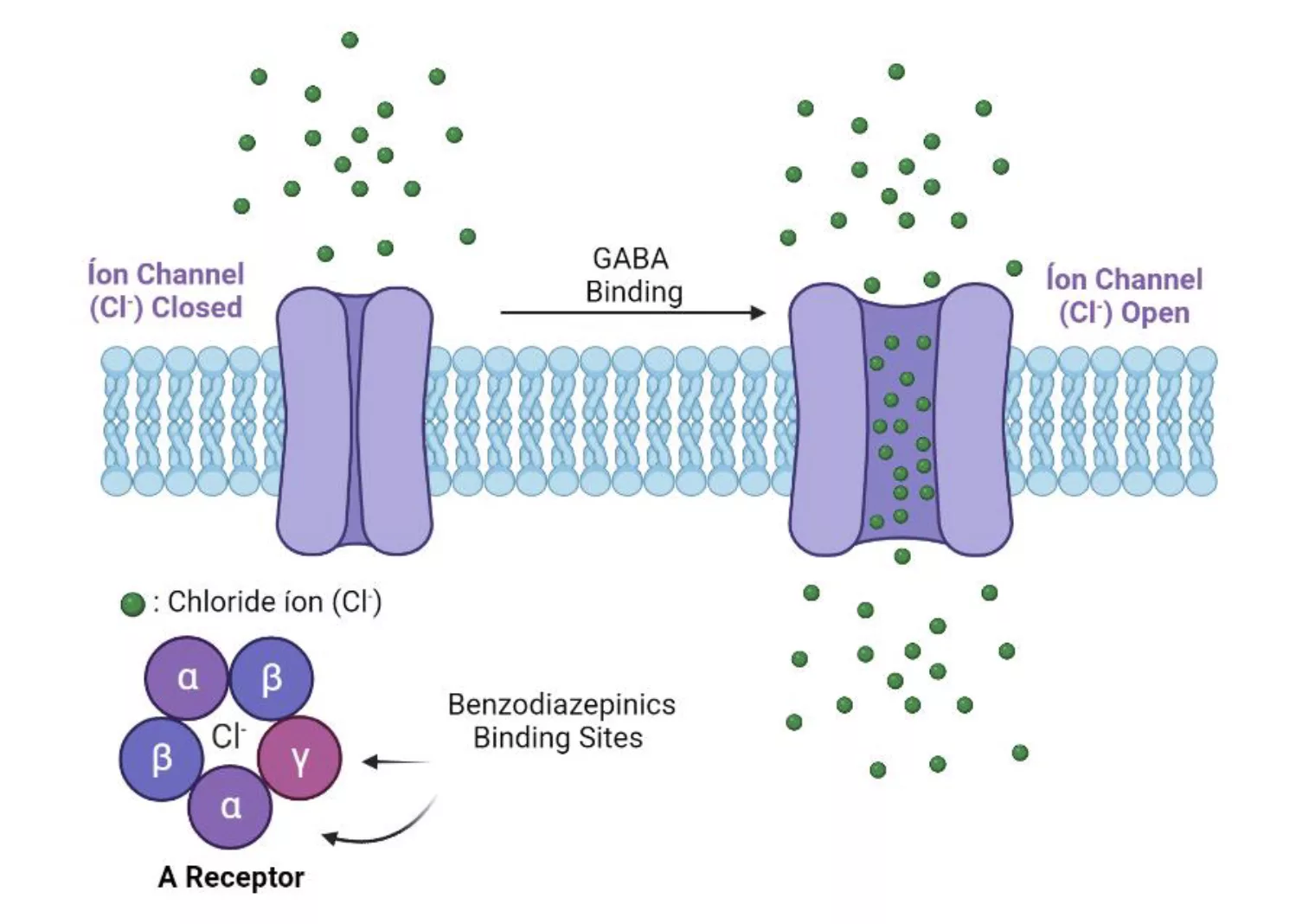
Benzodiazepines are CNS depressants that potentiate the effect of an inhibitory neurotransmitter: gamma-aminobutyric acid (GABA).
They act by binding the GABA-A receptor complex and increasing the affinity for GABA. When they are bound to the receptor, the opening of the chloride ion channel is facilitated. Chloride ions then flow into the neuron, causing it to become hyperpolarised. Hyperpolarisation reduces the excitability of the neuron throughout the entire central nervous system.1Araújo ÉJF, Rezende-Júnior LM, Lima LKF, Silva-Júnior MPD, Silva OA, Sousa Neto BP, Almeida AAC, Gutierrez SJC, Tomé ADR, Lopes LDS, Ferreira PMP, Lima FDCA. Pathophysiological investigations, anxiolytic effects and interaction of a semisynthetic riparin with benzodiazepine receptors. Biomed Pharmacother. 2018 Jul;103:973-981.
Therapeutic Effects of Benzodiazepines:
- Anxiety relief
- Sedation
- Muscle relaxation
- Anticonvulsant activity
Effects of Benzodiazepine Overdose:
Excessive enhancement of GABA inhibition leads to excessive CNS depression, especially when combined with other sedatives. Possible physiological consequences include:
| Symptom | Pathophysiology |
|---|---|
| Sedation | GABAergic activity suppresses cortical activity → drowsiness, lethargy |
| Ataxia | Cerebellar inhibition → poor coordination, slurred speech |
| Cognitive impairment | Frontal and hippocampal suppression → confusion, disorientation, anterograde amnesia |
| Hypotonia | Inhibition of spinal motor neurons → generalized muscle weakness |
| Respiratory depression | Suppression of brainstem respiratory centers → bradypnea, apnea, hypoxia |
| Hypotension | Sympathetic tone reduction + myocardial depression |
| Hypothermia | Impaired thermoregulation in prolonged overdose |
| Coma | Complete CNS suppression → unresponsiveness, especially in mixed overdoses |
Symptoms of Benzodiazepine Overdose
The clinical presentation of benzodiazepine overdose reflects the physiological effects; symptoms range from mild sedation to life-threatening respiratory depression.
Mild to Moderate Overdose:
- Drowsiness, lethargy
- Slurred speech
- Ataxia (stumbling gait, loss of coordination)
- Nystagmus (involuntary eye movements)
- Confusion
- Mild hypotension
- Normal or slightly depressed respiration
Severe Overdose (often with Co-Ingestants):
- Coma (no response to pain)
- Marked respiratory depression
- Systolic BP less than 90 mmHg
- Hypothermia (<35°C)
- Loss of protective airway reflexes (risk of aspiration)
- Cardiac arrest due to hypoxia
- Pupils are usually normal-sized and reactive, distinguishing BZD overdose from opioid toxicity.
Epidemiology of Benzodiazepine Overdose
A critical stat about benzodiazepine overdose is that it rarely happens in isolation. Most severe cases, over 70-80% in the US, involve co-ingestion of other CNS depressants, usually opioids.2Kleinman, R.A., Weiss, R.D. Benzodiazepine-Involved Overdose Deaths in the USA: 2000–2019. J GEN INTERN MED 37, 2103–2109 (2022).
In cases of overdose, benzodiazepines flood GABA-A receptors, leading to excessive CNS inhibition. However, due to their ceiling effect, a pharmacological safeguard, they rarely cause deep coma or death. But when mixed with opioids, alcohol, or barbiturates, they override this safeguard.
Opioid vs Benzodiazepine Overdose:
Though both drug classes depress the CNS, they target different respiratory centers, making their combination especially deadly.
- Opioids act on the pre-Bötzinger complex: the brainstem’s rhythm generator, slowing the initiation of breaths.
- Benzodiazepines suppress medullary and pontine centers, reducing the brain’s drive to breathe.
When they act together, the result is sedation, apnea, and death, often before emergency services can intervene. These aren’t just additive effects; they are synergistic, leading to outcomes neither drug would cause alone.
Other Dangerous Co-Ingestants:
| Co-Ingestant | Mechanism of Interaction | Clinical Consequences |
| Alcohol (ethanol) | Acts on GABA-A and NMDA receptors; worsens sedation, impairs airway protection | Exaggerated CNS depression, risk of aspiration, hypoxia, psychomotor impairment3Goroff D, Farinelli A. Benzodiazepine and Alcohol Co-Ingestion. J Coll Emerg Med Serv. 2018; 1(2): 19-23. |
| Barbiturates | Directly open GABA-A channels (even without GABA), unlike BZDs | Severe, prolonged coma, hypotension, refractory respiratory depression |
| Z-drugs (e.g. zolpidem, zopiclone) | Bind GABA-A receptor at BZD site; additive sedative and hypnotic effect | Increased risk of confusion, falls, and respiratory depression |
| Tricyclic Antidepressants (TCAs) | Anticholinergic, pro-arrhythmic, and pro-convulsant; TCAs do not sedate synergistically but worsen the condition overall | Muscle relaxants (e.g., carisoprodol, cyclobenzaprine) |
| Antipsychotics | Dopamine blockade + QT prolongation + anticholinergic effects | Worsened sedation, hypotension, arrhythmias, neuroleptic malignant-like symptoms |
| Gabapentinoids (gabapentin, pregabalin) | Modulate calcium channels; sedative when combined with other depressants | Heightened sedation, bradypnea, altered consciousness |
| Increased CNS depression, delirium, and respiratory risk | Sedative and anticholinergic properties; often misused with BZDs | Increased CNS depression, delirium, respiratory risk |
| Cannabinoids | May potentiate sedative effects and impair coordination when combined | Enhanced psychomotor slowing, confusion, possible hallucinations |
Differential Diagnosis
When a patient presents with reduced consciousness in the emergency department, benzodiazepine overdose is not the only possibility you should consider. Many conditions can mimic its presentation. A careful assessment of history, physical findings, and response to treatment helps differentiate among causes. Always assess for co-ingestants, especially opioids and alcohol.
| Condition | Key Features |
| Opioid overdose | Pinpoint pupils, severe respiratory depression, rapid reversal with naloxone |
| Barbiturate overdose | Similar CNS depression, longer duration, more profound hypotension |
| Alcohol intoxication | Ethanol odor, nystagmus, hypoglycemia, cerebellar signs |
| Hypoglycemia | Altered sensorium, diaphoresis, seizures, resolves with glucose |
| Head trauma | Focal neurological deficits, external signs of injury, vomiting |
| Hepatic encephalopathy | Asterixis, jaundice, elevated ammonia, chronic liver disease history |
| Stroke | Sudden onset, focal signs, unequal pupils, abnormal reflexes |
Diagnosis of Benzodiazepine Overdose
Diagnosis is primarily clinical, based on presentation and history of exposure. Toxicology screens can support the diagnosis, but aren’t definitive. This is usually true if synthetic or less commonly detected BZDs are involved. There is no pathognomonic sign, and differentials should always be considered.
History:
Information about ingestion (drug, amount, time), prescription history, substance use, psychiatric history, and potential co-ingestants.
In unconscious patients, collateral history from family, friends, or emergency services is vital.
Physical Examination:
Vitals (respiratory rate/pattern, oxygen saturation, BP, temperature), level of consciousness (Glasgow Coma Scale GCS), pupil size, neurologic exam (reflexes, tone), signs of trauma, and evidence of other toxins.
Toxicology Screening:
Urine Drug Screens (UDS)
- Can detect most common benzodiazepines with common metabolites.
- May miss agents like clonazepam, lorazepam, or designer benzo.
- Do not indicate dose, severity, or timing.
- Most useful for identifying co-ingestants (e.g., opioids, amphetamines).
Important to note that a positive UDS supports but does not confirm overdose; a negative result does not rule it out.
Serum Benzodiazepine Levels
- Rarely clinically useful in acute overdose management.
- Levels do not correlate with clinical severity due to tolerance, co-ingestants, and variable individual responses.
- It could be used in forensic or complex diagnostic scenarios, not routine management.
Specific Tests for Co-Ingestants
- Acetaminophen & salicylate levels: Check in all suspected intentional overdoses.
- Ethanol level: Helpful if alcohol co-ingestion is suspected.
- ECG: Mandatory to screen for cardiotoxic drugs (e.g., TCAs: look for widened QRS, QT prolongation).
Other Investigations:
Arterial Blood Gas (ABG)
Important to assess oxygenation (PaO2), ventilation (PaCO2), and acid-base status. Reveals hypoxemia, hypercapnia, and respiratory acidosis.
Basic Metabolic Panel (BMP)
Identify electrolyte disturbances, renal dysfunction, and hypoglycemia (can mimic coma).
Imaging
Chest X-ray if aspiration pneumonia is suspected. Head CT if head trauma or focal neurologic signs are present, or if diagnosis is uncertain.
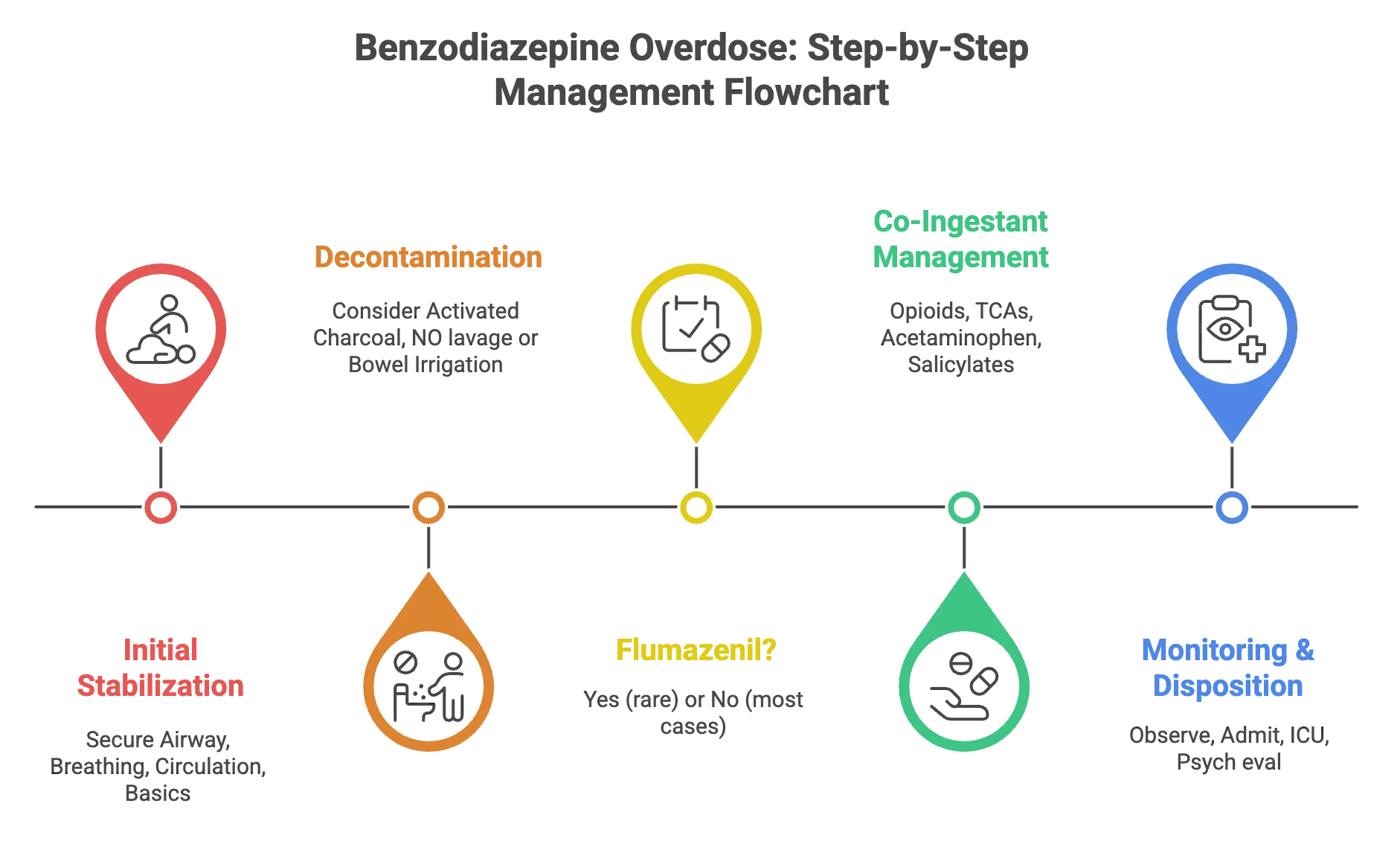
Management and Reversal of Benzodiazepine Overdose
The cornerstone of benzodiazepine overdose management is aggressive supportive care. There is no specific antidote universally recommended.4Druid H, Holmgren P, Ahlner J. Flunitrazepam: an evaluation of use, abuse and toxicity. Forensic Sci Int. 2001 Nov 01;122(2-3):136-41.
Step 1: Assess & Secure the ABCs:
Airway
- First priority is to secure the airways.
- If the airway is not protected (e.g., low GCS, absent gag reflex), intubate immediately.
- Prepare suction and airway equipment.
Breathing
- Check respiratory rate, depth, and SpO₂. Prepare high-flow supplemental oxygen.
- If significant respiratory depression occurs, begin with bag-valve-mask ventilation and intubate if no improvement.
- Aim for SpO₂ > 94%.
Circulation
- Establish IV access, monitor BP/HR.
- If hypotensive, give isotonic fluids (e.g., 0.9% saline boluses).
- Use vasopressors (e.g., norepinephrine) if persistent hypotension.
- Continuous cardiac monitoring is advised.
Step 2: Rapid Bedside Tests:
- Check blood glucose and treat hypoglycemia
- Warm hypothermic patients, but avoid rapid rewarming
- Check pupils & neurological exam for clues of co-ingestants
- Check for trauma or transdermal patches
Step 3: Consider Decontamination (Only in Select Cases):
Activated Charcoal (AC)5Zamani, N., Hassanian-Moghaddam, H., & Zamani, N. (2022). Strategies for the treatment of acute benzodiazepine toxicity in a clinical setting: the role of antidotes. Expert opinion on drug metabolism & toxicology, 18(6), 367–379. https://doi.org/10.1080/17425255.2022.2105692
- Not routinely used anymore, may be considered if the patient presents within 1-2 hours with a large overdose, and is awake or intubated.
- Contraindicated in unprotected airways due to aspiration risk.
- Never delay supportive care for activated charcoal administration.
Gastric Lavage & Whole Bowel Irrigation
- Not a recommended procedure because the risk of aspiration and esophageal injury outweighs the benefits.
Step 4: Administer Flumazenil if Indicated:
Flumazenil is a benzodiazepine receptor antagonist. It can reverse benzodiazepine-induced sedation, but its use is generally discouraged in emergency management of unknown or mixed overdoses.
Risks of Flumazenil
- In patients with chronic BZD use or dependence, flumazenil can trigger life-threatening withdrawal, including seizures.
- Can remove the protective anticonvulsant effect of BZDs in TCA, bupropion, or stimulant overdoses, leading to seizures or arrhythmias.
- Its half-life (40-80 mins) is shorter than most BZDs, meaning sedation and respiratory depression can recur, requiring repeated dosing or continuous infusion.6Maxa, J. L., Ogu, C. C., Adeeko, M. A., & Swaner, T. G. (2003). Continuous-infusion flumazenil in the management of chlordiazepoxide toxicity. Pharmacotherapy, 23(11), 1513–1516.
Indications for Flumazenil:
- Iatrogenic BZD overdose in a non-habituated patient (e.g., sedation error in a medical procedure).
- Known, isolated BZD overdose in a patient without a history of chronic use, dependence, or co-ingestants.
- Diagnostic tool in rare cases of unexplained coma (though EEG/monitoring may be safer).
If used, administer very slowly with seizure precautions in place. Start with 0.2 mg IV over 15 seconds. Repeat at 0.3–0.5 mg every minute, max of 3 mg.7An, H., & Godwin, J. (2016). Flumazenil in benzodiazepine overdose. CMAJ : Canadian Medical Association Journal, 188(17-18), E537. 8Sharbaf Shoar N, Bistas KG, Patel P, et al. Flumazenil. [Updated 2024 Feb 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470180/
Have airway support and benzodiazepines immediately available in case of paradoxical reactions.
Step 5: Management of Co-Ingestants:
Benzodiazepine overdose alone rarely causes death, but management of co-ingestions is often what actually determines the outcome. Assume they’re present until proven otherwise.
| Agent | Antidote / Treatment |
| Opioids | Naloxone (0.04–2 mg IV/IM/IN) |
| Tricyclic Antidepressants | Sodium bicarbonate (for QRS > 100 ms) |
| Acetaminophen | Start N-acetylcysteine (NAC) protocol |
| Salicylates | Alkalinize urine; consider dialysis |
| Ethanol | Supportive care |
Step 6: Monitoring:
- If asymptomatic after 6 hours, discharge can be considered with follow-up.
- If symptomatic (isolated BZD), admit for monitoring and supportive care. Recovery can be expected in 24–48 hrs.
- If co-ingestants or severe overdose, ICU admission is required for advanced support and management.
- If an intentional overdose, → Psychiatric evaluation is mandatory once stable
Prognosis of Benzodiazepine Overdose
Supportive care is usually really effective, and most patients with isolated benzodiazepine overdose recover fully. For example, with short-acting agents, recovery can be seen in as little as 6–12 hours.
Complications like aspiration pneumonia, hypoxic brain injury, or rhabdomyolysis occur primarily in polydrug overdoses. Mortality is low in cases of isolated overdoses. But the risk multiplies with co-ingestions, especially opioids.
Prevention & Public Health Considerations
Reducing the toll of benzodiazepine overdoses requires changes across the system.
- Prescribe benzodiazepines only when indicated, at the lowest effective dose for the shortest possible duration.
- Avoid long-term use for insomnia or anxiety where safer alternatives exist.
- Educate patients about the risks: dependence, tolerance, withdrawal, and the deadly combo with alcohol or opioids.
- Co-prescribe naloxone when patients are taking both opioids and benzodiazepines.
- Public health surveillance is important to track overdose trends, especially street benzos, fentanyl-laced pills, and synthetic sedatives.
Conclusion
Though it is a CNS depressant, benzodiazepine overdose does not kill by itself, but it isn’t very often the only drug involved. This is where it is dangerous, particularly when combined with other CNS depressants, particularly opioids, where the danger of respiratory arrest increases significantly. Management is generally supportive; the vast majority of isolated occurrences do well with airway support, monitoring, and stabilization.
Preventing these overdoses requires changes in prescribing habits, monitoring systems, and easier access to addiction care. The increased popularity of street BZDs only adds to the immediacy, particularly because these are increasingly used in conjunction with synthetic opioids.
Refrences
- 1Araújo ÉJF, Rezende-Júnior LM, Lima LKF, Silva-Júnior MPD, Silva OA, Sousa Neto BP, Almeida AAC, Gutierrez SJC, Tomé ADR, Lopes LDS, Ferreira PMP, Lima FDCA. Pathophysiological investigations, anxiolytic effects and interaction of a semisynthetic riparin with benzodiazepine receptors. Biomed Pharmacother. 2018 Jul;103:973-981.
- 2Kleinman, R.A., Weiss, R.D. Benzodiazepine-Involved Overdose Deaths in the USA: 2000–2019. J GEN INTERN MED 37, 2103–2109 (2022).
- 3Goroff D, Farinelli A. Benzodiazepine and Alcohol Co-Ingestion. J Coll Emerg Med Serv. 2018; 1(2): 19-23.
- 4Druid H, Holmgren P, Ahlner J. Flunitrazepam: an evaluation of use, abuse and toxicity. Forensic Sci Int. 2001 Nov 01;122(2-3):136-41.
- 5Zamani, N., Hassanian-Moghaddam, H., & Zamani, N. (2022). Strategies for the treatment of acute benzodiazepine toxicity in a clinical setting: the role of antidotes. Expert opinion on drug metabolism & toxicology, 18(6), 367–379. https://doi.org/10.1080/17425255.2022.2105692
- 6Maxa, J. L., Ogu, C. C., Adeeko, M. A., & Swaner, T. G. (2003). Continuous-infusion flumazenil in the management of chlordiazepoxide toxicity. Pharmacotherapy, 23(11), 1513–1516.
- 7An, H., & Godwin, J. (2016). Flumazenil in benzodiazepine overdose. CMAJ : Canadian Medical Association Journal, 188(17-18), E537.
- 8Sharbaf Shoar N, Bistas KG, Patel P, et al. Flumazenil. [Updated 2024 Feb 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470180/