Brucellosis is a zoonotic infection that was historically known as Mediterranean fever. Over time, it has been associated with various regional names, including Maltese fever, Gibraltar fever, Crimean fever, Bang disease, goat fever, gastric remittent fever, and Undulant Fever. It affects animals and humans and is one of the most widespread diseases that develop due to the genus ‘Brucella’.1Qureshi, K. A., Parvez, A., Fahmy, N. A., Abdel Hady, B. H., Kumar, S., Ganguly, A., Atiya, A., Elhassan, G. O., Alfadly, S. O., Parkkila, S., & Aspatwar, A. (2023). Brucellosis: epidemiology, pathogenesis, diagnosis, and treatment-a comprehensive review. Annals of Medicine, 55(2), 2295398. https://doi.org/10.1080/07853890.2023.2295398
What is Brucellosis?
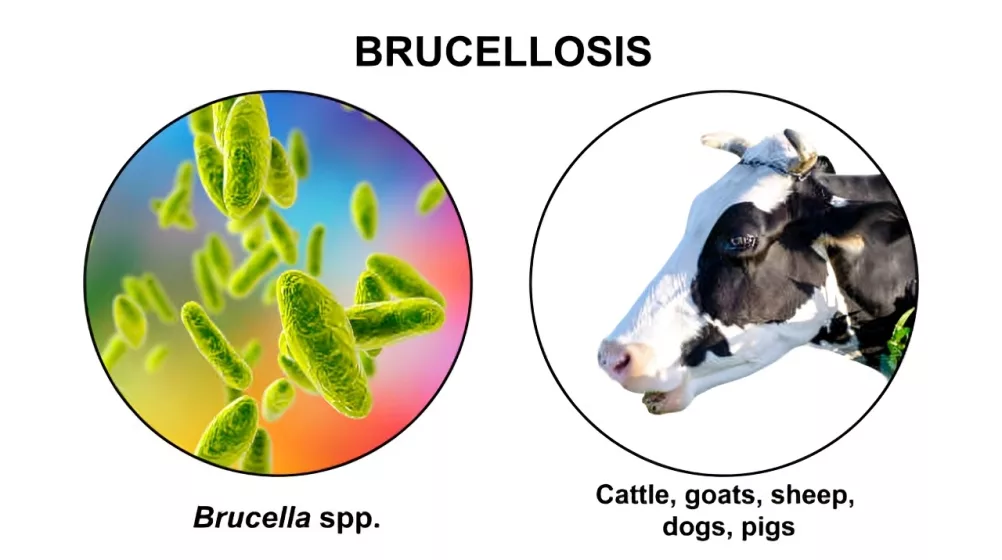
Brucellosis is a zoonotic bacterial infection caused by the Brucella genus, affecting both humans and animals. The disease is characterized by undulant fever, fatigue, joint pain, and other systemic symptoms. It is primarily transmitted to humans through direct contact with infected animals, consumption of contaminated animal products, or inhalation of infectious aerosols. While it is found worldwide, its prevalence is higher in regions with inadequate veterinary control and poor food safety practices. If untreated, brucellosis can lead to severe complications, including arthritis, endocarditis, and neurological disorders.
Common Brucella Species in Humans
The disease was first described in 1751 by George Cleghorn, a British army surgeon, based on his observations in the Mediterranean region. However, the causative organism was not identified until 1887, when David Bruce isolated Brucella melitensis from patients and livestock in Malta. Brucellosis has many different species, but four of its most common forms that are present in humans include:
- Brucella melitensis: The most pathogenic species, transmitted from sheep and goats, and responsible for severe disease cases.
- Brucella suis: Linked to pigs and associated with chronic, often complicated infections.
- Brucella abortus: Primarily found in cattle, causing milder infections in humans.
- Brucella canis: Found in dogs, less common but increasingly recognized as a potential source of human infection.

How common is Brucellosis?
Brucellosis is a globally prevalent zoonotic disease that continues to pose a significant threat to public health due to its complex nature and widespread distribution. Among the various Brucella species, Brucella abortus and Brucella melitensis are the most common pathogens affecting humans. B. melitensis is particularly severe and often leads to debilitating illness, while B. abortus tends to cause milder disease. The Middle East, North Africa, and South Asia are regions with the highest prevalence of brucellosis, raising serious public health concerns.
According to the World Health Organization (WHO), 500,0000 cases of Brucellosis infection are reported yearly.2Centers for Disease Control and Prevention (CDC). (2024). Brucellosis. In CDC Yellow Book: Health Information for International Travel. Retrieved from https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/brucellosis
In developing countries, children are frequently affected, whereas in developed regions, the disease is more prevalent among young adults aged 25-45 who work in livestock farming, veterinary medicine, or food processing. Men are more commonly affected than women, likely due to occupational exposure.
Almost 86 different countries reported cases of brucellosis. It impacts economic conditions and is an alarming sign for human health globally. The top countries affected by Brucella disease include North Africa and Eastern countries. The disease is common in various Asian countries, including Pakistan, Sri Lanka, China, and India, affecting both animals and humans.
How does Brucellosis disease spread?
Brucellosis primarily spreads from infected animals to humans through the consumption of unpasteurized dairy products (e.g., milk, cheese) or undercooked meat, as well as direct contact with infected animals or their secretions, such as urine, milk, and placental fluids. Inhalation of aerosolized bacteria is another route of transmission, particularly in occupational settings. While wild animals can carry Brucella bacteria, they pose a lower transmission risk to humans due to limited direct contact.
Rare cases of person-to-person transmission have been reported, such as through congenital infection or tissue transplantation. Statistics indicate that from 2004 to 2021, China reported 684,293 cases of human brucellosis, averaging approximately 38,016 cases annually. The disease has significant economic impacts, including decreased milk production, spontaneous abortions, and reduced fertility in livestock. This underscores the need for effective control measures to mitigate the public health and economic burdens of brucellosis.3de Figueiredo, P., Ficht, T. A., Rice-Ficht, A., Rossetti, C. A., & Adams, L. G. (2015). Pathogenesis and immunobiology of brucellosis: review of Brucella-host interactions. The American journal of pathology, 185(6), 1505–1517. https://doi.org/10.1016/j.ajpath.2015.03.003
Symptoms of Brucellosis
Brucellosis often presents as a severe flu-like illness, with symptoms including sweating, undulating fever, headaches, muscle pain, chills, fatigue, and joint pain. In some cases, it can affect other organs, such as the liver, heart, and spleen. The hallmark feature of brucellosis is undulating fever, characterized by periodic rises and falls in body temperature. Less common symptoms include vomiting, diarrhea, abdominal pain, and, in severe cases, complications like miscarriage during pregnancy.4Edathodu, J., Alamri, M., Alshangiti, K. A., Alfagyh, N. S., Alnaghmush, A. S., Albaiz, F., Alothman, B., Khalil, H., Edathodu, Z., & Alrajhi, A. A. (2021). Clinical manifestations and treatment outcomes of human brucellosis at a tertiary care center in Saudi Arabia. Annals of Saudi Medicine, 41(2), 109–114. https://doi.org/10.5144/0256-4947.2021.109
Other common symptoms of brucellosis include:
- Cyclical fever and headache
- Migratory arthralgia (joint pain that moves from one joint to another)
- Asthenia (weakness)
- Anorexia (loss of appetite)
- Fatigue and general malaise
- Vomiting
- Diarrhea
How to diagnose Brucellosis?
Several serological and microbial laboratories use PCR to diagnose Brucella disease, as it is one of the most essential and effective methods to diagnose this disease. Furthermore, a simple and frequently used method is blood culture. Still, in the last few years, due to a lack of funding, facilities, and other medical limitations in developing countries, the commonly used technique is PCR.5Navarro, E., Casao, M. A., & Solera, J. (2004). Diagnosis of human brucellosis using PCR. Expert review of molecular diagnostics, 4(1), 115–123. https://doi.org/10.1586/14737159.4.1.115
The following tests help to diagnose this disease:
- Complete Blood Count (CBC): Helps detect anemia or leukopenia, which may occur in brucellosis.
- Inflammatory Markers: Elevated levels of markers like C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) indicate inflammation.
- Blood Culture: A standard method to isolate Brucella bacteria in acute cases.
- Serology: Tests like the Rose Bengal test and ELISA detect antibodies against Brucella.
- Liver Enzymes: Elevated levels may indicate liver involvement.
- Polymerase Chain Reaction (PCR): A highly sensitive and specific method for Brucella detection.
- Radiography: Used to assess complications, such as joint or bone involvement.
- Biopsy: Rarely used but may confirm the diagnosis in localized infections.6Freire, M. L., Machado de Assis, T. S., Silva, S. N., & Cota, G. (2024). Diagnosis of human brucellosis: Systematic review and meta-analysis. PLoS Neglected Tropical Diseases, 18(3), e0012030. https://doi.org/10.1371/journal.pntd.0012030
Treatment of Brucellosis:
Treatment for brucellosis typically involves antibiotics tailored to the severity and circumstances of the infection. Commonly prescribed medications include doxycycline, rifampin, streptomycin, gentamicin, and trimethoprim-sulfamethoxazole (TMP-SMX), used alone or in combination. Whether the patient needs to use this medicine for several weeks or months depends on each individual’s severity of the infection.
The World Health Organization (WHO) and other clinical guidelines recommend the following antibiotic regimens:
Adults
- Doxycycline 100 mg twice daily plus rifampin 600–900 mg daily for six weeks.
- Alternatively, doxycycline 100 mg twice daily for six weeks combined with streptomycin 1 g daily intramuscularly for 2–3 weeks.7World Health Organization. (1986). Joint FAO/WHO Expert Committee on Brucellosis Sixth Report. https://apps.who.int/iris/handle/10665/40175
Children under 8 years
- Cotrimoxazole (trimethoprim-sulfamethoxazole) plus rifampin for six weeks.8 Huang, S., Xu, J., Wang, H., et al. (2024). Updated therapeutic options for human brucellosis: A systematic review and network meta-analysis of randomized controlled trials. PLoS Neglected Tropical Diseases, 18(8), e0012405. https://doi.org/10.1371/journal.pntd.0012405
Pregnancy
- Rifampin (600–900 mg daily) combined with TMP-SMX for 6–8 weeks.
- Gentamicin 3–5 mg/kg/day intramuscularly for 1 week, combined with TMP-SMX for 6 weeks, may be used if rifampin is unavailable.9 Arenas-Gamboa, A. M., Rossetti, C. A., et al. (2016). Human Brucellosis and Adverse Pregnancy Outcomes. Current Tropical Medicine Reports, 3(4), 164–172. https://doi.org/10.1007/s40475-016-0092-010Huang, S., Xu, J., Wang, H., Li, Z., Song, R., Zhang, Y., Lu, M., Han, X., Ma, T., Wang, Y., Hao, J., Song, S., Zhen, Q., & Shui, T. (2024). Updated therapeutic options for human brucellosis: A systematic review and network meta-analysis of randomized controlled trials. PLoS Neglected Tropical Diseases, 18(8), e0012405. https://doi.org/10.1371/journal.pntd.0012405
Prevention of Brucellosis
Prevention of Brucella disease is done by regularly vaccinating animals and maintaining good hygiene and sanitation practices. Ensuring dairy products are pasteurized and cooking meat thoroughly can significantly reduce the risk of transmission. Awareness campaigns targeting farmers, consumers of raw dairy products, and health workers are critical for effective control of the disease. Animal health management systems also need to develop strategies to control this disease to reduce potential risk factors and the causes of widespread brucellosis.
National and local animal health services play a vital role in managing brucellosis by implementing disease control strategies, such as monitoring livestock and vaccinating animals. According to a report in Spain, 12% of laboratory workers get Brucella during fieldwork. For this reason, the government needs to provide proper safety tools to health workers to reduce this disease.11E. Bouza, C. Sánchez-Carrillo, S. Hernangómez, M. José González, The Spanish Co-operative Group for the Study of Laboratory-acquired Brucellosis, Laboratory-acquired brucellosis: a Spanish national survey, Journal of Hospital Infection, Volume 61, Issue 1, 2005, Pages 80-83, ISSN 0195-6701, https://doi.org/10.1016/j.jhin.2005.02.018. (https://www.sciencedirect.com/science/article/pii/S0195670105001465)
How does Brucellosis affect pregnancy?
Brucellosis disease is dangerous for pregnant women because of its adverse outcomes. It can create complications for the mothers during pregnancy. In specific regions, including South Africa and Central America, human brucellosis is a significant health problem. It is a serious health concern because it can affect multiple body parts. Brucellosis affects the pregnancy in the following ways:12Khan, M. Y., Mah, M. W., & Memish, Z. A. (2001). Brucellosis in pregnant women. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America, 32(8), 1172–1177. https://doi.org/10.1086/319758
- Spontaneous Abortion (SA)
- Intrauterine fetal death (IUFD)
- Congenital Brucellosis
Pregnant women are particularly vulnerable to complications due to the infection’s impact on multiple organ systems. One of the most common and concerning problems is abortion.13Arenas-Gamboa, A. M., Rossetti, C. A., Chaki, S. P., Garcia-Gonzalez, D. G., Adams, L. G., & Ficht, T. A. (2016). Human Brucellosis and Adverse Pregnancy Outcomes. Current Tropical Medicine Reports, 3(4), 164–172. https://doi.org/10.1007/s40475-016-0092-0
Historically, brucellosis-related pregnancy complications have been documented as early as 1905, when the first case of abortion due to Brucella infection was reported in France. By 1937, preterm delivery associated with the disease was observed, followed by a series of 59 cases in 1938. The incidence of brucellosis in pregnant women is estimated at 1.5–2.1% among adult cases, with most affected women aged 25–29 years.14Bosilkovski M, Arapović J, Keramat F. Human brucellosis in pregnancy – an overview. Bosn J Basic Med Sci. 2020 Nov 2;20(4):415-422. doi: 10.17305/bjbms.2019.4499. PMID: 31782698; PMCID: PMC7664790.
Symptoms of Brucellosis In Pregnant Women:
Symptoms of Brucellosis in pregnant women include weakness, fever, excessive night sweating, and lack of appetite. Pregnant women also suffer from mild illness when Brucella organisms start activating in their bodies. Timely diagnosis is critical. Even after taking medication to treat brucellosis, it is still challenging during pregnancy. Rifampicin, combined with TMP-SMX, is commonly used to treat brucellosis during pregnancy. For pregnant women, the period to take this medicine is mainly 6 to 8 weeks. Some doctors also recommend gentamicin for 1 week plus TMP-SMX for 6 weeks, with or without rifampicin.15Roushan MR, Baiani M, Asnafi N, Saedi F. Outcomes of 19 pregnant women with brucellosis in Babol, northern Iran. Trans R Soc Trop Med Hyg. 2011 Sep;105(9):540-2. doi: 10.1016/j.trstmh.2011.06.003. Epub 2011 Jul 13. PMID: 21742362
Difference between Brucellosis and Q fever
Brucellosis and Q fever are zoonotic infections affecting animals and humans. While brucellosis, caused by Brucella species, commonly manifests as fever, muscle pain, fatigue, headaches, cyclical fever, migratory arthralgia, and in severe cases, miscarriage, Q fever, caused by Coxiella burnetii, often presents with hepatitis or pneumonia.
Chronic Q fever can result in endocarditis and severe organ damage, making it a potentially more severe condition in certain cases. Brucellosis is primarily transmitted through direct contact with infected animals or consumption of contaminated animal products, while Q fever spreads via inhalation of aerosols containing C. burnetii. Both diseases require timely diagnosis and treatment to prevent complications.16Cadmus, S., Salam, S. P., Adesokan, H. K., Akporube, K., Ola-Daniel, F., & Awosanya, E. J. (2021). Seroprevalence of brucellosis and Q fever infections amongst pastoralists and their cattle herds in Sokoto State, Nigeria. PloS one, 16(7), e0254530. https://doi.org/10.1371/journal.pone.0254530
Conclusion:
Brucellosis is a zoonotic infection by Brucella species and is one of the most widespread diseases affecting animals and humans. It transfers from animals to humans by various factors, including inhalation of aerosols or direct contact with infected animals. The constant use of unpasteurized dairy products and raw meat can cause brucellosis.
This disease can risk human and animal lives and cause enormous economic and financial loss for farmers, stakeholders, and consumers. For this reason, vaccination of animals can help reduce the potential risk of brucellosis.
Refrences
- 1Qureshi, K. A., Parvez, A., Fahmy, N. A., Abdel Hady, B. H., Kumar, S., Ganguly, A., Atiya, A., Elhassan, G. O., Alfadly, S. O., Parkkila, S., & Aspatwar, A. (2023). Brucellosis: epidemiology, pathogenesis, diagnosis, and treatment-a comprehensive review. Annals of Medicine, 55(2), 2295398. https://doi.org/10.1080/07853890.2023.2295398
- 2Centers for Disease Control and Prevention (CDC). (2024). Brucellosis. In CDC Yellow Book: Health Information for International Travel. Retrieved from https://wwwnc.cdc.gov/travel/yellowbook/2024/infections-diseases/brucellosis
- 3de Figueiredo, P., Ficht, T. A., Rice-Ficht, A., Rossetti, C. A., & Adams, L. G. (2015). Pathogenesis and immunobiology of brucellosis: review of Brucella-host interactions. The American journal of pathology, 185(6), 1505–1517. https://doi.org/10.1016/j.ajpath.2015.03.003
- 4Edathodu, J., Alamri, M., Alshangiti, K. A., Alfagyh, N. S., Alnaghmush, A. S., Albaiz, F., Alothman, B., Khalil, H., Edathodu, Z., & Alrajhi, A. A. (2021). Clinical manifestations and treatment outcomes of human brucellosis at a tertiary care center in Saudi Arabia. Annals of Saudi Medicine, 41(2), 109–114. https://doi.org/10.5144/0256-4947.2021.109
- 5Navarro, E., Casao, M. A., & Solera, J. (2004). Diagnosis of human brucellosis using PCR. Expert review of molecular diagnostics, 4(1), 115–123. https://doi.org/10.1586/14737159.4.1.115
- 6Freire, M. L., Machado de Assis, T. S., Silva, S. N., & Cota, G. (2024). Diagnosis of human brucellosis: Systematic review and meta-analysis. PLoS Neglected Tropical Diseases, 18(3), e0012030. https://doi.org/10.1371/journal.pntd.0012030
- 7World Health Organization. (1986). Joint FAO/WHO Expert Committee on Brucellosis Sixth Report. https://apps.who.int/iris/handle/10665/40175
- 8Huang, S., Xu, J., Wang, H., et al. (2024). Updated therapeutic options for human brucellosis: A systematic review and network meta-analysis of randomized controlled trials. PLoS Neglected Tropical Diseases, 18(8), e0012405. https://doi.org/10.1371/journal.pntd.0012405
- 9Arenas-Gamboa, A. M., Rossetti, C. A., et al. (2016). Human Brucellosis and Adverse Pregnancy Outcomes. Current Tropical Medicine Reports, 3(4), 164–172. https://doi.org/10.1007/s40475-016-0092-0
- 10Huang, S., Xu, J., Wang, H., Li, Z., Song, R., Zhang, Y., Lu, M., Han, X., Ma, T., Wang, Y., Hao, J., Song, S., Zhen, Q., & Shui, T. (2024). Updated therapeutic options for human brucellosis: A systematic review and network meta-analysis of randomized controlled trials. PLoS Neglected Tropical Diseases, 18(8), e0012405. https://doi.org/10.1371/journal.pntd.0012405
- 11E. Bouza, C. Sánchez-Carrillo, S. Hernangómez, M. José González, The Spanish Co-operative Group for the Study of Laboratory-acquired Brucellosis, Laboratory-acquired brucellosis: a Spanish national survey, Journal of Hospital Infection, Volume 61, Issue 1, 2005, Pages 80-83, ISSN 0195-6701, https://doi.org/10.1016/j.jhin.2005.02.018. (https://www.sciencedirect.com/science/article/pii/S0195670105001465)
- 12Khan, M. Y., Mah, M. W., & Memish, Z. A. (2001). Brucellosis in pregnant women. Clinical infectious diseases: an official publication of the Infectious Diseases Society of America, 32(8), 1172–1177. https://doi.org/10.1086/319758
- 13Arenas-Gamboa, A. M., Rossetti, C. A., Chaki, S. P., Garcia-Gonzalez, D. G., Adams, L. G., & Ficht, T. A. (2016). Human Brucellosis and Adverse Pregnancy Outcomes. Current Tropical Medicine Reports, 3(4), 164–172. https://doi.org/10.1007/s40475-016-0092-0
- 14Bosilkovski M, Arapović J, Keramat F. Human brucellosis in pregnancy – an overview. Bosn J Basic Med Sci. 2020 Nov 2;20(4):415-422. doi: 10.17305/bjbms.2019.4499. PMID: 31782698; PMCID: PMC7664790.
- 15Roushan MR, Baiani M, Asnafi N, Saedi F. Outcomes of 19 pregnant women with brucellosis in Babol, northern Iran. Trans R Soc Trop Med Hyg. 2011 Sep;105(9):540-2. doi: 10.1016/j.trstmh.2011.06.003. Epub 2011 Jul 13. PMID: 21742362
- 16Cadmus, S., Salam, S. P., Adesokan, H. K., Akporube, K., Ola-Daniel, F., & Awosanya, E. J. (2021). Seroprevalence of brucellosis and Q fever infections amongst pastoralists and their cattle herds in Sokoto State, Nigeria. PloS one, 16(7), e0254530. https://doi.org/10.1371/journal.pone.0254530