Brugada syndrome is a rare condition that can lead to abnormal heartbeat. It can be very dangerous and is caused by faulty genes inherited from parents. The abnormal heartbeat begins in the lower chambers of the heart. Prevention is the best way to manage it. Preventative measures include avoiding medications that affect the heart and reducing fever.
What is Brugada Syndrome?
Brugada Syndrome is an uncommon yet potentially life-threatening inherited condition that makes individuals more susceptible to fatal cardiac arrhythmias. Cardiac arrhythmias involve irregular heartbeats that can lead to fainting and, in severe instances, even death. This syndrome typically manifests during periods of sleep or rest.
Its distinctive identification on an electrocardiogram (ECG) lies in the specific presence of a right bundle branch block and elevated ST segments, particularly observed in the right precordial leads (V1-V3).
Causes of Brugada Syndrome
Brugada syndrome occurs due to mutations in the genes. The most common gene is the SCN5A gene, but other genes can also be involved. SCN5A gene encodes for voltage-gated sodium channels, which are important in producing sodium current for the upstroke of the cardiac action potential. These channels are pivotal in regulating the heart’s electrical activity, influencing heartbeat and rhythm. When sodium channels are flawed, this disrupts the entire process, leading to an irregular heartbeat.
It is an autosomal dominant condition linked to mutations in the SCN5A gene. This suggests a high likelihood of inheritance if one parent carries the gene mutation, although it’s important to note that inheritance isn’t guaranteed in every case. Some people develop Brugada syndrome without inheriting it from their parents; instead, it results from spontaneous genetic mutations in SCN5A genes.
It is also a possibility that a person with a faulty gene does not develop any symptoms throughout his life, and the syndrome stays dormant. However, certain conditions can trigger abnormal electrical activity and heartbeat. The most important triggers include1Peters, C. H., Abdelsayed, M., & Ruben, P. C. (2016). Triggers for arrhythmogenesis in the Brugada and long QT 3 syndromes. Progress in biophysics and molecular biology, 120(1-3), 77–88. https://doi.org/10.1016/j.pbiomolbio.2015.12.009:
- Antipsychotic drugs
- Antidepressant drugs
- Illegal drugs
- Conditions that cause fever
- Heat exhaustion
- Lithium
- Sodium channel blockers
- Dehydration
- Too much alcohol
- Electrolyte imbalance

Risk Factors for Brugada Syndrome
Some risk factors are stated next:
Family History
If anyone in the family has Brugada syndrome, the related people also have a higher risk of developing it as compared to those who do not have these patients in their families.2Wu, W., Tian, L., Ke, J., Sun, Y., Wu, R., Zhu, J., & Ke, Q. (2016). Risk factors for cardiac events in patients with Brugada syndrome: A PRISMA-compliant meta-analysis and systematic review. Medicine, 95(30), e4214. https://doi.org/10.1097/MD.0000000000004214
Gender & Racial Factor
Researchers think that the male hormone Testosterone has a role in inducing the symptoms of Brugada syndrome. Hence, Men are more at risk of developing it than women.3Milman, A., Gourraud, J. B., Andorin, A., Postema, P. G., Sacher, F., Mabo, P., Conte, G., Giustetto, C., Sarquella-Brugada, G., Hochstadt, A., Kim, S. H., Juang, J. J. M., Maeda, S., Takahashi, Y., Kamakura, T., Aiba, T., Leshem, E., Michowitz, Y., Rahkovich, M., Mizusawa, Y., … Belhassen, B. (2018). Gender differences in patients with Brugada syndrome and arrhythmic events: Data from a survey on arrhythmic events in 678 patients. Heart rhythm, 15(10), 1457–1465. https://doi.org/10.1016/j.hrthm.2018.06.019Similarly, it is more common in Asian people than in other races.
Age
Symptoms often appear in people who are in their late 30s or 40s.4Milman, A., Andorin, A., Gourraud, J. B., Sacher, F., Mabo, P., Kim, S. H., Maeda, S., Takahashi, Y., Kamakura, T., Aiba, T., Conte, G., Juang, J. J. M., Leshem, E., Rahkovich, M., Hochstadt, A., Mizusawa, Y., Postema, P. G., Arbelo, E., Huang, Z., Denjoy, I., … Belhassen, B. (2017). Age of First Arrhythmic Event in Brugada Syndrome: Data From the SABRUS (Survey on Arrhythmic Events in Brugada Syndrome) in 678 Patients. Circulation. Arrhythmia and electrophysiology, 10(12), e005222. https://doi.org/10.1161/CIRCEP.117.005222
Fever
A fever is not the causative factor of Brudaga syndrome. However, it triggers the heart, leading to the appearance of symptoms like dizziness or fainting.5Roomi, S. S., Ullah, W., Abbas, H., Abdullah, H., Talib, U., & Figueredo, V. (2020). Brugada syndrome unmasked by fever: a comprehensive review of the literature. Journal of Community Hospital Internal Medicine Perspectives, 10(3), 224–228. https://doi.org/10.1080/20009666.2020.1767278
Drugs
Certain drugs, including tricyclic antidepressants, cocaine, marijuana, lithium, and sodium channel blockers, also increase the risk of triggering the symptoms.
Symptoms of Brugada Syndrome
Brudaga syndrome does not always cause symptoms. So, many people do not know if they have the syndrome or not.
In case the symptoms occur with Brugada syndrome, they can be:
- Dizziness
- Fainting
- Difficulty in breathing and gasping at night
- Abnormal heartbeat – maybe fast and chaotic
- Palpitations – awareness of one’s heartbeat
- Seizures or fits
- Cardiac arrest during sleep
- Blackouts
- Chest pain
- Sudden Cardiac Death6 Nakano, Y., & Shimizu, W. (2022). Brugada Syndrome as a Major Cause of Sudden Cardiac Death in Asians. JACC. Asia, 2(4), 412–421. https://doi.org/10.1016/j.jacasi.2022.03.011
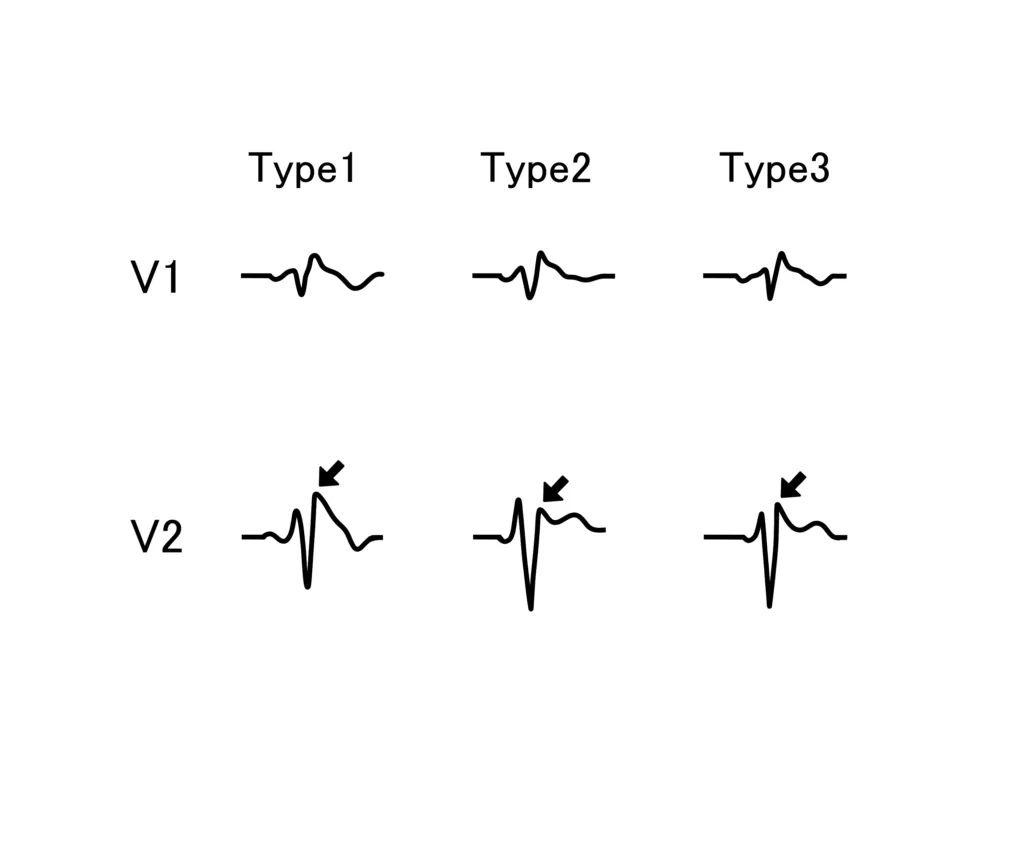
Types of Brugada Syndrome
In reality, Brugada Syndrome has only one type. Characteristic Brugada syndrome ECG shows ST segment elevation and T wave inversion. Different ECG patterns are seen depending upon variations in ST-segment elevation characteristics. Based on these ECG patterns, it is categorized into three types7Richter S. (2015). Das Brugada-EKG [Brugada ECG]. Herzschrittmachertherapie & Elektrophysiologie, 26(3), 247–259. https://doi.org/10.1007/s00399-015-0391-5. ECG is a type of investigation that measures electrical activity in different areas of the heart to check for different heart diseases.
Type 1 Brugada ECG Pattern
The graph obtained after doing an ECG has different parts. For Brugada syndrome, the ST segment and T wave are important. In type 1 Brugada morphology, there is a coved ST segment elevation greater than 2mm, and the T wave is inverted.
Type 2 Brugada ECG Pattern
In this morphology, the ST segment of ECG is “saddle shape,” and the T wave is biphasic. It is not a diagnostic feature of Brugada syndrome but raises suspicion, and further tests should be conducted.
Type 3 Brugada ECG Pattern
It consists of a coved or saddleback pattern of less than 2 mm ST-segment elevation in ECG. This feature was considered diagnostic of Brugada syndrome, but not anymore. It is important to understand that Brugada syndrome does not always show characteristic ECG.
Brugada ECG Pattern
Some people do not have the Brugada disease itself, i.e., they do not have abnormal heartbeat or rhythm, but their electrocardiogram (ECG) shows otherwise. This condition is called the Brugada ECG pattern. It is not harmful if the condition is temporary. But even for these individuals, it is necessary to undergo proper medical evaluation and monitoring to rule out any underlying cardiac conditions.
Diagnosis of Brugada Syndrome
A physician will suspect Brugada syndrome if any of the above symptoms develop in a person or if he has a positive family history. The physician will perform a full clinical examination and review medical and family history. The next step is to undergo proper medical diagnostic tests to establish a definitive diagnosis.8Vohra, J., Rajagopalan, S., & CSANZ Genetics Council Writing Group (2015). Update on the Diagnosis and Management of Brugada Syndrome. Heart, lung & circulation, 24(12), 1141–1148. https://doi.org/10.1016/j.hlc.2015.07.020
Tests for Brugada Syndrome
Electrocardiogram
ECG records the electrical activity of the heart and is helpful in the diagnosis of Brugada syndrome. However, the ECG might not give accurate results in the first attempt. So, it is repeated two to three times with repositioning of the chest leads to get appropriate results. The characteristic ECG findings of Brugada syndrome include incomplete right bundle branch block and greater than 2 mm ST segment elevation in anterior precordial leads (type 1).
Genetic Testing
Genetic testing of the SCN5A gene is done to check if the patient has the mutated gene responsible for this syndrome. The family members might also be tested. Genetic testing for SCN5A has a sensitivity of almost 20 percent.
ECG with medication
If the ECG does not give any result, the “drug challenge” is done. In this test, the patient is given a medicine that blocks the sodium channels. The most commonly used medicine is Ajmaline, which is an antiarrhythmic agent. Other antiarrhythmic agents like procainamide, flecainide, and propafenone are also used. An ECG is done after that, which shows a type 1 Brugada ECG pattern if the test is positive.
This test is done in hospital settings under professional guidance to uncover hidden Brugada syndrome.
Lab Investigations
Electrolyte imbalances like hyperkalemia and hypercalcemia can also cause ST segment elevation in the right precordial leads. So, to rule out electrolyte imbalance, a physician might recommend a complete electrolyte profile.
Treatment of Brugada Syndrome
Once the diagnosis has been established, the next step is to treat or manage the patient. Unfortunately, this condition has no cure because the problem is in the genes. The management aims to ensure the patient does not have ventricular fibrillation or abnormal rhythms. The treatment might include:
Medications
Isoproterenol, quinidine, and amiodarone might be prescribed by the doctor to prevent abnormal heartbeat.
Cardiac Ablation
In this procedure, the radiofrequency ablation of the anterior right ventricular outflow tract is done. When ventricular fibrillation episodes become too frequent, ablation is a good option. It is a new emerging treatment for Brugada syndrome, and it is showing promising results.
Implanted Cardioverter Defibrillator (ICD)
ICD implantation is the mainstay treatment in most cases of Brugada syndrome. It is a device that is implanted in a patient’s heart. When it detects the onset of ventricular fibrillation or any abnormal rhythm of the heartbeat, it either stops it or gives shock to the heart which resets the rhythm9Shinohara, T., Abe, I., Hirota, K., Kondo, H., Fukui, A., Akioka, H., Teshima, Y., Yufu, K., Nakagawa, M., & Takahashi, N. (2021). The usefulness of subcutaneous implantable cardioverter-defibrillator therapy in patients with Brugada syndrome. Heart and vessels, 36(2), 260–266. https://doi.org/10.1007/s00380-020-01683-0.
Complications of ICD:
ICD is not a perfect device. It can cause problems by giving a shock at the wrong time. It can also malfunction or cause an infection. The physician will guide the patient about various treatment options. It is important to take these preventative treatments even if the patient has never experienced a symptom. This is because the first symptom can be sudden cardiac death.
Lifestyle Modification for Brugada Syndrome:
It is important to avoid certain triggers to prevent stimulating cardiac events. Everyday activities like exercise, sex, pregnancy, and driving can be done easily by some people. However, some people have problems navigating these activities due to recurrent cardiac events. It is important to consult an electrophysiologist, genetic counselor, and primary care physician to develop a lifestyle that suits the symptoms best.
Doctors and physicians provide support, but living with a serious condition can have its own mental and emotional effects. Staying in touch with family, cultivating meaningful relationships and connections, and joining support groups is important.
Is Brugada Syndrome Dangerous?
It can be potentially life-threatening. Brugada syndrome can cause ventricular fibrillation. Ventricles are the chambers of the heart that pump blood to the lungs and the body. In the case of ventricular fibrillation, the heart does not pump enough blood to the body and the brain. It can lead to sudden fainting and cardiac arrest.
Life Expectancy
The risk of cardiac events is low in patients with asymptomatic Brugada syndrome. Type 1 ECG patterns and symptoms are associated with more cardiac events. There is no treatment for Brugada syndrome. However, people who modify their lifestyle accordingly and take appropriate preventative treatments have a better life expectancy.
Brugada Syndrome vs. ARVD
The most common abnormality associated with sudden cardiac death apart from Brugada syndrome is Arrhythmogenic Right Ventricular Dysplasia (ARVD). They can be differentiated from each other by considering the following differences.
- Brugada is associated with the SCN5A gene; ARVD is not.
- Brugada syndrome has no structural cardiac abnormality; ARVD shows fibrofatty infiltration.
- ARVD is precipitated by exercise or catecholamines; Brugada syndrome symptoms usually occur at rest or during sleep.
Some other conditions having similar presentations include the following:
- Acute myocardial infarction
- Cocaine intoxication
- Electrolyte imbalance
- Right or left bundle branch block
- Right ventricular outflow tract compression
- Left ventricular hypertrophy
A thorough history, clinical examination, and ECG findings help distinguish Brugada Syndrome.
To sum it up, Brugada syndrome is a serious genetic disorder that can cause sudden death due to heart arrest. It is important to take preventative measures to avoid triggering cardiac events. There is no cure for the disease, but people who optimize their lives accordingly have a pretty good quality of life.
Refrences
- 1Peters, C. H., Abdelsayed, M., & Ruben, P. C. (2016). Triggers for arrhythmogenesis in the Brugada and long QT 3 syndromes. Progress in biophysics and molecular biology, 120(1-3), 77–88. https://doi.org/10.1016/j.pbiomolbio.2015.12.009
- 2Wu, W., Tian, L., Ke, J., Sun, Y., Wu, R., Zhu, J., & Ke, Q. (2016). Risk factors for cardiac events in patients with Brugada syndrome: A PRISMA-compliant meta-analysis and systematic review. Medicine, 95(30), e4214. https://doi.org/10.1097/MD.0000000000004214
- 3Milman, A., Gourraud, J. B., Andorin, A., Postema, P. G., Sacher, F., Mabo, P., Conte, G., Giustetto, C., Sarquella-Brugada, G., Hochstadt, A., Kim, S. H., Juang, J. J. M., Maeda, S., Takahashi, Y., Kamakura, T., Aiba, T., Leshem, E., Michowitz, Y., Rahkovich, M., Mizusawa, Y., … Belhassen, B. (2018). Gender differences in patients with Brugada syndrome and arrhythmic events: Data from a survey on arrhythmic events in 678 patients. Heart rhythm, 15(10), 1457–1465. https://doi.org/10.1016/j.hrthm.2018.06.019
- 4Milman, A., Andorin, A., Gourraud, J. B., Sacher, F., Mabo, P., Kim, S. H., Maeda, S., Takahashi, Y., Kamakura, T., Aiba, T., Conte, G., Juang, J. J. M., Leshem, E., Rahkovich, M., Hochstadt, A., Mizusawa, Y., Postema, P. G., Arbelo, E., Huang, Z., Denjoy, I., … Belhassen, B. (2017). Age of First Arrhythmic Event in Brugada Syndrome: Data From the SABRUS (Survey on Arrhythmic Events in Brugada Syndrome) in 678 Patients. Circulation. Arrhythmia and electrophysiology, 10(12), e005222. https://doi.org/10.1161/CIRCEP.117.005222
- 5Roomi, S. S., Ullah, W., Abbas, H., Abdullah, H., Talib, U., & Figueredo, V. (2020). Brugada syndrome unmasked by fever: a comprehensive review of the literature. Journal of Community Hospital Internal Medicine Perspectives, 10(3), 224–228. https://doi.org/10.1080/20009666.2020.1767278
- 6Nakano, Y., & Shimizu, W. (2022). Brugada Syndrome as a Major Cause of Sudden Cardiac Death in Asians. JACC. Asia, 2(4), 412–421. https://doi.org/10.1016/j.jacasi.2022.03.011
- 7Richter S. (2015). Das Brugada-EKG [Brugada ECG]. Herzschrittmachertherapie & Elektrophysiologie, 26(3), 247–259. https://doi.org/10.1007/s00399-015-0391-5
- 8Vohra, J., Rajagopalan, S., & CSANZ Genetics Council Writing Group (2015). Update on the Diagnosis and Management of Brugada Syndrome. Heart, lung & circulation, 24(12), 1141–1148. https://doi.org/10.1016/j.hlc.2015.07.020
- 9Shinohara, T., Abe, I., Hirota, K., Kondo, H., Fukui, A., Akioka, H., Teshima, Y., Yufu, K., Nakagawa, M., & Takahashi, N. (2021). The usefulness of subcutaneous implantable cardioverter-defibrillator therapy in patients with Brugada syndrome. Heart and vessels, 36(2), 260–266. https://doi.org/10.1007/s00380-020-01683-0





