Coccidioidomycosis,’ also known as ‘valley fever,’ ‘Desert Rheumatism,’ or ‘San Joaquin Valley Fever,’ is a common fungal illness caused by Coccidioides. This fungus is found in the soil and dust of the Southwestern United States, Northern Mexico, and certain regions of Central and South America.1Brown, J., Benedict, K., Park, B. J., & Thompson III, G. R. (2013). Coccidioidomycosis: epidemiology. Clinical epidemiology, 185-197 Although usually benign, it may lead to life-threatening situations in some individuals.
What is Coccidioidomycosis?
Coccidioidomycosis is a common fungal infection. You may contract it when you inhale spores of fungi Coccidioides immitis or Coccidioides posadasii, found in the soil of endemic regions. It affects almost twenty thousand people annually, with most cases reported from California and Arizona.2Valley fever. Cleveland Clinic. (n.d.). Retrieved April 19, 2023, from https://my.clevelandclinic.org/health/diseases/17754-valley-fever Most people inhaling spores don’t get infected or exhibit benign, flu-like symptoms. On the contrary, some get sick and even develop serious complications. These people may not recover.
How do we get Coccidioidomycosis?
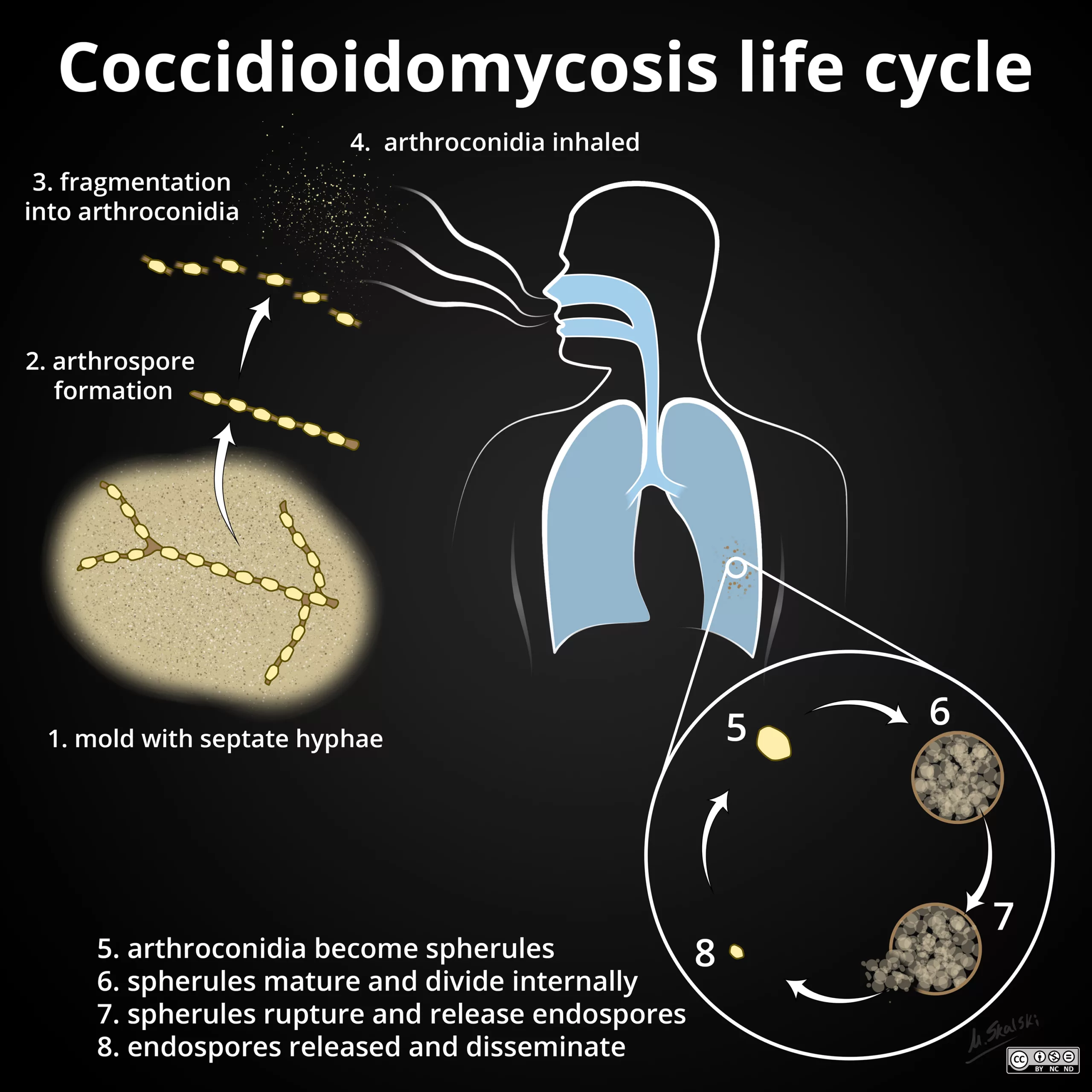
After winds, farming, or construction disturbs soil laden with this fungus, Coccidioides spores get dispersed in the environment. They are now present in the air we breathe. Once inhaled, these spores settle in our airways, transforming into spherules(round, double-walled structures containing hundreds to thousands of spores). These spherules enlarge with time, break down, and release endospores(offspring spores) that may lodge in your lungs and even be carried via the lymphatics to other parts of your body.3Bays DJ, Thompson GR III. Coccidioidomycosis. Infect Dis Clin North Am. 2021. 35(2):453-469
In some cases, spores may enter your body by direct penetration through a pre-existing skin breach, a cut, or a wound. In either case, the endospores challenge your immune system and trigger inflammatory responses by the body. Most of the time, our immune system dominates, and we are safe from serious forms of Coccidioidomycosis. In contrast, in some cases, especially in people from high-risk groups, our immunity can’t rid us of the infection: the benign illness progresses to a more dangerous ailment, requiring medical intervention and a longer course of treatment.
Who is at Risk for Coccidioidomycosis?
Though Coccidioidomycosis can affect anybody, some people are more vulnerable. These include:
- People who have a weak immune system, such as those on long-term steroid therapy, those undergoing organ transplantation, or people with defective immunity, e.g., HIV/AIDS
- People with diabetes
- People aged 60 years and above
- Pregnant women
- People having high occupational exposure to Coccidioides-laden soil
- Some races, e.g., the Blacks and the Filipinos
Coccidioidomycosis: What are the Symptoms?
The clinical picture of Coccidioidomycosis ranges from literally no symptoms at all to severe respiratory problems. Some of the most common coccidioidomycosis symptoms include:4Blair, J. E., Chang, Y. H. H., Cheng, M. R., Vaszar, L. T., Vikram, H. R., Orenstein, R., … & Parish, J. M. (2014). Characteristics of patients with mild to moderate primary pulmonary coccidioidomycosis. Emerging infectious diseases, 20(6), 983.
- Fever
- Shortness of breath
- Cough
- Rash on upper body and legs
- Fatigue
- Chest pain
- Headache
- Night sweats
- Muscle aches and joint pains
How Long do the Symptoms Last?
Coccidioidomycosis symptoms usually appear one to three weeks after exposure to the fungus and may take several weeks to months to subside.
Are there any Complications?
In a fraction of patients, approximately 5 to 10%, the illness progresses to grave lung problems, which take longer to recover. In an even smaller fraction, 0.6% of patients, the infection disseminates via lymphatics to other body organs and affects them.
Disseminated Coccidioidomycosis
In disseminated coccidioidomycosis, the infection disseminates and involves other body parts. It is seen more commonly in vulnerable groups. In this case, the primary infection spreads to other body organs a few months to a year after the initial infection. The primary disease may also reactivate in these patients. Furthermore, in case of more extensive involvement, you may also experience:
- Skin lesions like nodules and ulcers that are more troublesome than the usual coccidioidomycosis rash
- Lesions that cause pain in the spine, skull, or other bones
- Joint pain and swelling, particularly in the knees and ankles
- When the fungus permeates your nervous system, it may infect the membranes and fluid around the brain and spinal cord, causing meningitis. Note that this condition is deadly if not treated in time. So, if you experience neck stiffness, high-grade fever, or seizures, visit the nearby emergency center immediately.
Coccidioidomycosis: How to Get it Diagnosed?
Diagnosing coccidioidomycosis is not easy: your physician might have to rule out illnesses with a similar clinical picture before giving a final verdict. However, if this disease is common in your locality or if you have recently traveled to an endemic area, then your doctor will suspect it. He will take a thorough history and perform a relevant physical examination. After this, he might order the following tests to confirm his suspicion:
- Blood tests to detect Coccidioides’ antigens or antibodies: It is one of the most common lab tests to diagnose Coccidioidomycosis
- A CT scan or chest X-ray is performed to look for signs of lung infection. The scans may reveal characteristic findings, such as lung nodules or cavities, aiding in diagnosis.
- Culture of the fungus from a blood or tissue sample. It may be used to grow and identify Coccidioides fungi from clinical specimens.5Coba, A. J., Sallee, P. K., Dixon, D. O., Alkhateb, R., & Anstead, G. M. (2021). Pandora’s Box: Disseminated Coccidioidomycosis Associated with Self-Medication with an Unregulated Potent Corticosteroid Acquired in Mexico. Tropical Medicine and Infectious Disease, 6(4), 207. https://doi.org/10.3390/tropicalmed6040207
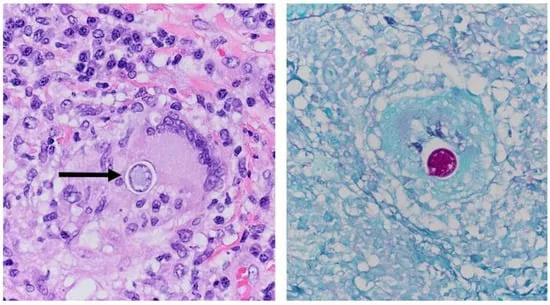
- Histological Examination: When tissue samples from patients suspected of having valley fever are examined under a microscope after H&E staining, characteristic features of the fungal infection caused by Coccidioides species can be observed. Specifically, H&E staining helps visualize the distinctive spherules of Coccidioides fungi within the affected tissues. These spherules are large, round structures containing endospores, the infective forms of the fungus.
- Polymerase chain reaction (PCR) testing: This molecular technique can detect Coccidioides DNA in clinical samples, providing a rapid and specific diagnosis.6Martinez-Del-Campo E, Kalb S, Rangel-Castilla L, Moon K, Moran A, Gonzalez O, Soriano-Baron H, Theodore N. Spinal Coccidioidomycosis: A Current Review of Diagnosis and Management. World Neurosurg. 2017 Dec;108:69-75.
Coccidioidomycosis: The Treatment
Normally, our bodies get rid of the fungus on their own. When planning coccidioidomycosis treatment, doctors aim to manage your symptoms to decrease discomfort. Moreover, depending on your immunity and the severity of your illness, doctors want to prevent any complications you may be at risk of acquiring.
Rest:
In most cases, you would require rest and nothing else to recover. Yes, if you have a strong immunity and mild-to-moderate illness, your doctor will advise you to rest adequately and maintain good fluid intake. He will also keep track of how well you are recovering.
Antifungal Treatments:
You may need antifungals like itraconazole and fluconazole if your illness progresses and you respond poorly to the conventional options. You may also require them if your doctor deems you at a higher risk for acquiring complications or if you have disseminated coccidioidomycosis.7Thompson GR, Lewis JS, Nix DE, Patterson TF. Current Concepts and Future Directions in the Pharmacology and Treatment of Coccidioidomycosis. Med Mycol. 2019 Feb 01;57(Supplement_1):S76-S84.
They need to be taken for at least three to six months and even longer in some individuals.
Prevention of Coccidioidomycosis
The most effective method to prevent coccidioidomycosis is to avoid exposure to fungus altogether. But no matter how hard you try, you can’t entirely prevent it while living in an endemic region.8Martinez-Del-Campo E, Kalb S, Rangel-Castilla L, Moon K, Moran A, Gonzalez O, Soriano-Baron H, Theodore N. Spinal Coccidioidomycosis: A Current Review of Diagnosis and Management. World Neurosurg. 2017 Dec;108:69-75.
Nevertheless, we can still adopt these precautions to minimize exposure as much as possible:
- Use an N95 filtration face mask whenever you go outside.
- Avoid dusty areas, such as farms, gardens, and construction sites.
- Close your doors and windows during a dust storm. Stay indoors.
- If you can’t avoid contact with soil, better to dampen it before working with it.
- Use soap and water to clean skin injuries. Maintain good hand hygiene.
Can Coccidioidomycosis be Fatal?
Yes, it can be fatal. But the good news is that deadly complications, such as meningitis or disseminated disease, are rare. Also, a vigilant diagnosis and prompt treatment can help prevent them.
Is Coccidioidomycosis Contagious?
No, it is a soil-borne disease. It doesn’t transmit from person to person. The only carrier is soil laden with fungal spores.
Prognosis
The prognosis is generally good, with most individuals recovering fully without complications. However, individuals with more severe infections or underlying health conditions may have a longer recovery time. They may be at a higher risk of complications and even reactivation of primary disease.
Conclusion
Coccidioidomycosis is a common fungal infection. Otherwise benign, it can potentially lead to deadly complications. People with compromised immunity are more at risk of contracting it. Symptoms vary from mild flu to rare, insuperable respiratory and nervous system problems. Though we can adopt preventive measures, the crux of the matter lies in timely diagnosis and vigilant management of the disease.
Refrences
- 1Brown, J., Benedict, K., Park, B. J., & Thompson III, G. R. (2013). Coccidioidomycosis: epidemiology. Clinical epidemiology, 185-197
- 2Valley fever. Cleveland Clinic. (n.d.). Retrieved April 19, 2023, from https://my.clevelandclinic.org/health/diseases/17754-valley-fever
- 3Bays DJ, Thompson GR III. Coccidioidomycosis. Infect Dis Clin North Am. 2021. 35(2):453-469
- 4Blair, J. E., Chang, Y. H. H., Cheng, M. R., Vaszar, L. T., Vikram, H. R., Orenstein, R., … & Parish, J. M. (2014). Characteristics of patients with mild to moderate primary pulmonary coccidioidomycosis. Emerging infectious diseases, 20(6), 983.
- 5Coba, A. J., Sallee, P. K., Dixon, D. O., Alkhateb, R., & Anstead, G. M. (2021). Pandora’s Box: Disseminated Coccidioidomycosis Associated with Self-Medication with an Unregulated Potent Corticosteroid Acquired in Mexico. Tropical Medicine and Infectious Disease, 6(4), 207. https://doi.org/10.3390/tropicalmed6040207
- 6Martinez-Del-Campo E, Kalb S, Rangel-Castilla L, Moon K, Moran A, Gonzalez O, Soriano-Baron H, Theodore N. Spinal Coccidioidomycosis: A Current Review of Diagnosis and Management. World Neurosurg. 2017 Dec;108:69-75.
- 7Thompson GR, Lewis JS, Nix DE, Patterson TF. Current Concepts and Future Directions in the Pharmacology and Treatment of Coccidioidomycosis. Med Mycol. 2019 Feb 01;57(Supplement_1):S76-S84.
- 8Martinez-Del-Campo E, Kalb S, Rangel-Castilla L, Moon K, Moran A, Gonzalez O, Soriano-Baron H, Theodore N. Spinal Coccidioidomycosis: A Current Review of Diagnosis and Management. World Neurosurg. 2017 Dec;108:69-75.

