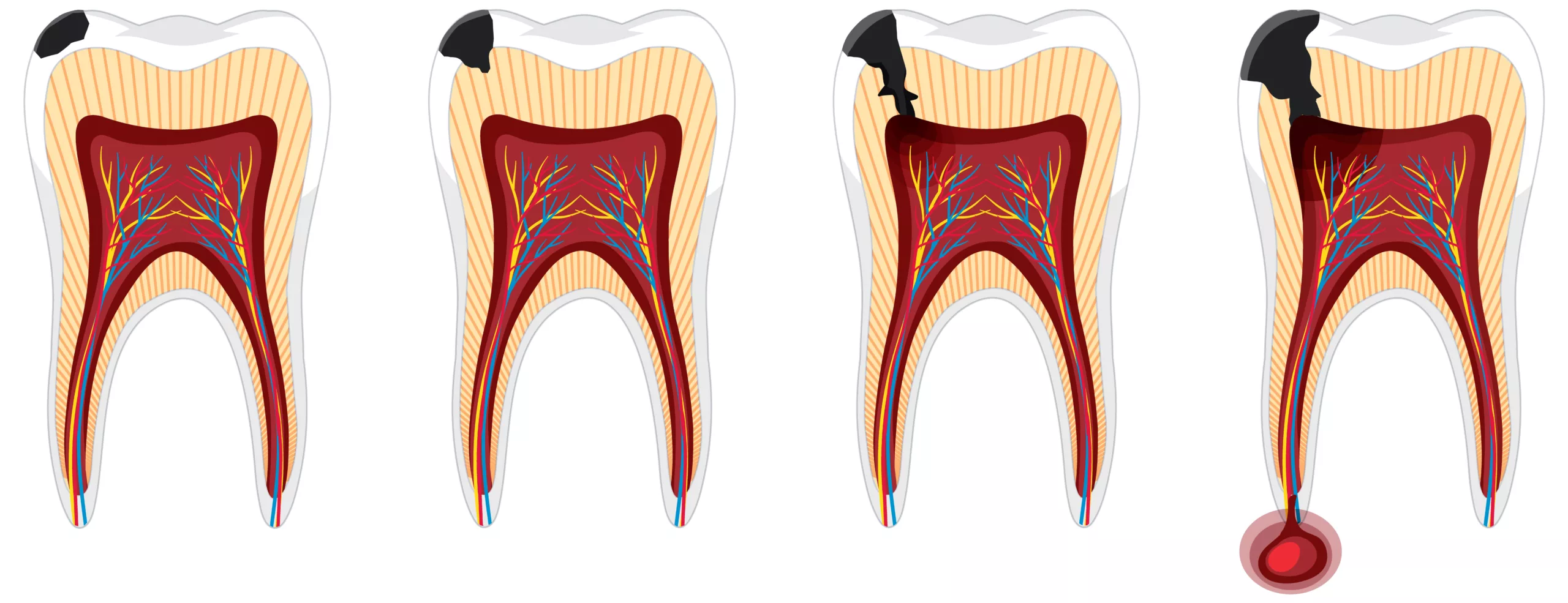
Dental pulp necrosis is the death of the tooth’s innermost layer, called the pulp. The dental pulp is the soft tissue found in the center of the tooth.1Yu, Christine, and Paul V. Abbott. “An overview of the dental pulp: its functions and responses to injury.” Australian Dental Journal 52 (2007): S4-S6. It keeps the tooth vital and plays a crucial role in the overall health and function of the tooth. The pulp extends from the crown of the tooth, where it lies within the pulp chamber, down through the root canals to the tip of the root (or apex) in the jawbone. It contains blood vessels, nerves, and connective tissue.
Pulp necrosis can significantly affect the oral health of an individual and can lead to severe complications if not managed properly.

Dental Pulp Necrosis
The pulp tissue is in the center of the tooth and has a pivotal role in maintaining the vitality of the tooth by providing nutrients and sensory function. Pulp necrosis occurs when the pulp tissue becomes irreversibly damaged causing its death. This process often results from ischemic conditions where the blood supply to the tooth is compromised or due to infection and inflammation.
Forms of Pulp Necrosis
Necrosis of the pulp can occur due to various pathophysiological mechanisms, ischemic and liquefactive being two primary forms. The two types of necrosis differ in their causes, progression, and histological characteristics. Understanding these types is crucial for proper diagnosis and management of pulp necrosis.
Ischemic Pulp Necrosis
Ischemic pulp necrosis occurs when the blood supply to the dental pulp is significantly reduced or completely cut off, leading to tissue death due to a lack of oxygen and nutrients. The pulp tissue relies on a healthy vascular system to function properly, and any disruption to this blood supply can result in ischemic damage.
Causes of Ischemic Pulp Necrosis:
There can be various contributing factors for ischemic pulp necrosis but the most common are as follows.
Trauma
Physical trauma, like a blunt blow to the tooth, can lead to damage of the blood supply of the tooth. This can occur due to accidents, sports injuries, and other situations where the tooth experiences a sudden blow. The result can be disruption of blood flow eventually leading the pulp to become ischemic and ultimately necrotic.2Andreasen, J. O. “Textbook and color atlas of traumatic injuries to the teeth.” Munksgard. Copenhagen 155 (1993): 172-173.
Excessive Pressure
Prolonged pressure on the pulpal tissue due to bruxism (teeth grinding) or because of deep tooth restoration can compress the blood supply to the pulp, thus reducing the blood flow and causing ischemic necrosis.3Jafarzadeh, Hamid, and P. V. Abbott. “Review of pulp sensibility tests. Part I: general information and thermal tests.” International endodontic journal 43.9 (2010): 738-762.
Repetitive Dental Procedures
If a tooth undergoes treatment repeatedly, especially for deep fillings and restorations like crown placement, it may induce chronic pressure and stress on the dental pulp. Multiple treatments on the same inflamed tooth pulp can compromise the vascular system of the pulp. This, in turn, leads to ischemia.4Bergenholtz, Gunnar. “Pathogenic mechanisms in pulpal disease.” Journal of Endodontics 16.2 (1990): 98-101.
Pathophysiology of Ischemic Necrosis:
When blood flow to the pulp is disrupted, the tissue becomes hypoxic, meaning it is deprived of oxygen. Without oxygen, the cells within the pulp can not produce the energy needed to thrive. Subsequently, they led to cell death and necrosis. The process of ischemic necrosis typically results in a dry, coagulative form of tissue death, where the overall structure of the pulp may remain intact for some time, even though the cells within the tissue are no longer viable.55. Hargreaves, Kenneth M., Harold E. Goodis, and Franklin R. Tay, eds. Seltzer and Bender’s dental pulp. Batavia, IL, USA: Quintessence Pub., 2012.
Clinical Presentation of Ischemic Pulp Necrosis:
Below are some of the clinical features that can be observed in patients with ischemic necrosis.
Initial Sensitivity
Patients may experience mild sensitivity to temperature changes. They might feel a cold sensation in the tooth in the initial stages. The sensation may be brief and less intense than in cases of pulpitis.
Diminishing Pain
As ischemia progresses, the tooth starts losing its vitality, thus giving the false impression that the issue has been resolved. Reduction and absence of pain due to loss of nerve function mask the symptoms.
Tooth Discoloration
One of the hallmark signs of ischemic necrosis is tooth discoloration. Due to the breakdown of blood cells in the pulp chamber, the tooth may appear grey, yellow, or darkened. This is often the first visible sign of a traumatic injury to the tooth.
Asymptomatic Period
A tooth may become completely asymptomatic for a long period in ischemic necrosis. This happens due to loss of pulp vitality and the patient does not feel any pain. This makes the condition harder to detect without routine dental checkups.
Tenderness on Percussion
Despite the lack of spontaneous pain, the patient may feel tenderness on biting pressure or percussion. This is due to inflammation in the periapical area surrounding the tooth.
Minimal Swelling
Unlike liquefactive necrosis, ischemic necrosis typically presents with minimal to no swelling unless there is a secondary infection.
Radiographic Findings
Initially, no changes are visible in the radiograph, but gradually, a radiolucency may appear in the periapical area, indicating the onset of periapical inflammation.
Liquefactive Pulp Necrosis
Liquefactive pulp necrosis is characterized by the breakdown of pulp tissue into a liquid state. This necrosis is typically caused by bacterial infection, leading to severe inflammation and accumulating pus and other fluids within the pulp chamber.
Causes of Liquefactive Necrosis:
The most common causes of liquefactive necrosis are listed below
Bacterial infection
Bacterial invasion is the most common cause of liquefactive necrosis. It usually occurs when deep caries or a crack in the tooth allows bacteria to reach the pulp. Once inside the pulp chamber, the bacteria proliferate, triggering an inflammatory response. Immune cells accumulate and release enzymes that break down the pulp tissue.

Untreated pulpitis
If reversible or irreversible pulpitis is not treated timely, the inflammation can progress, leading to liquefactive necrosis.6Nair, PN Ramanchandran. “Pathogenesis of apical periodontitis and the causes of endodontic failures.” Critical Reviews in Oral Biology & Medicine 15.6 (2004): 348-381.
Pathophysiology of Liquefactive Necrosis:
In liquefactive necrosis, bacterial toxins and the human immune response lead to the breakdown of the dental pulp tissue into a liquid form. Lysosomal enzymes from neutrophils and other immune cells infiltrate the pulp in response to infection. As a result, a pus-filled, liquid mass of necrotic tissue is formed, often leading to a periapical abscess at the root tip.
This necrosis is more aggressive than ischemic due to bacterial infection and immune response. The pulp tissue is liquified and may lead to immense pain, swelling, and, eventually, abscess formation if not managed properly.
Clinical Presentation of Liquefactive Necrosis:
Severe Spontaneous Pain
Liquefactive necrosis often presents with intense, spontaneous pain that may be throbbing or continuous. The pain is usually exacerbated by biting, chewing, or exposure to heat, and it may radiate to adjacent areas.
Swelling & Abscess
Liquefactive necrosis is commonly associated with gum swelling due to pus accumulation in the pulp chamber and the periapical area. If left untreated, the pus can spread to the surrounding tissue, leading to facial asymmetry.
Pain of Percussion
The affected tooth is painful on palpation due to an underlying infection in the periapical area. Applying pressure on the tooth can elicit sharp pain.
Foul Taste or Odor
Patients with liquefactive necrosis often report a foul taste and bad breath due to pus drainage in the oral cavity. This often indicates an advanced stage of infection.
Tooth Mobility
As the infection spreads, it destroys the adjacent bone structure. This is particularly common when the abscess is large, and the periodontal tissue is also affected. This results in tooth mobility.
Radiographic Findings
Radiographs usually show signs of periapical pathology, such as periapical radiolucency which indicates bone loss and abscess formation on the root tip. This radiolucency is the key diagnostic feature of liquefactive necrosis.
Systemic Symptoms
In severe cases, the patient may complain of fever, malaise, and lymphadenopathy—the swelling of lymph nodes. This indicates that the infection has spread beyond the localized area of the tooth, potentially leading to more dangerous outcomes like cellulitis or osteomyelitis.
Drainage of Pus
In cases where an abscess ruptures, patients may experience drainage of pus through a fistula in the gum tissue. This can temporarily alleviate pain but does not resolve the underlying infection.
Progressive Spread of Infection
If left untreated, the infection associated with liquefactive necrosis can spread to adjacent teeth, the jawbone, and even distant areas such as the sinuses or facial spaces, leading to potentially life-threatening complications.
Types of Pulp Necrosis
There is another classification of pulp necrosis based on the extent of damage. It is primarily classified into two main categories.
Partial Necrosis
In partial necrosis of the tooth, only a segment of the pulp has died, and the remaining portion retains vitality. This scenario occurs when a localized portion of the pulp becomes affected while the remaining portion continues receiving blood supply and responds to stimuli. Although the tooth retains some sensitivity, it feels less sensitive than a normal tooth. Despite the partial nature of the tooth’s vitality, the tooth still must undergo treatment. Root canal therapy is usually the go-to option to prevent the necrosis from spreading throughout the pulp. Early diagnosis and intervention are key to managing partial necrosis effectively and preserving the tooth’s health.7Hargreaves, Kenneth M., Harold E. Goodis, and Franklin R. Tay, eds. Seltzer and Bender’s dental pulp. Batavia, IL, USA: Quintessence Pub., 2012
Complete Necrosis
Complete necrosis occurs when the entire pulp tissue within a tooth has died, rendering the tooth non-vital. In cases of total necrosis, the pulp completely loses its blood supply, nerve function, and ability to respond to external stimuli. Typically, the tooth will not respond to temperature or vitality tests, and the patient may experience no pain initially, though periapical inflammation or infection often follow if left untreated. Total necrosis occurs due to prolonged deep cries or untreated trauma. Endodontic treatment- root canal therapy is necessary to remove the necrotic tissue and prevent infection spread.
Diagnosing Pulp Necrosis
Diagnosing dental pulp necrosis involves a combination of clinical evaluation and diagnostic tests. Accurate diagnosis is essential for determining the appropriate treatment plan.
Clinical Examination
A dentist should thoroughly examine teeth and surrounding tissue to check for abscess, swelling, discoloration, or any visible tooth decay and necrosis.
Pulp Vitality Test
Pulp vitality tests are essential diagnostic tools used by dentists to assess the health and function of dental pulp. These tests help determine whether the pulp is vital (alive and healthy) or non-vital (necrotic or dead). The most used tests include thermal tests and electric pulp tests. Each evaluates the pulp’s sensory response, which indicates its vitality.
Thermal tests
Thermal tests involve exposing the tooth to extreme temperatures. The test aims to elicit a response from the tooth under extreme conditions. If the tooth is healthy, the patient will feel sensitive to heat and cold stimuli. A lack of response to these stimuli indicates a dead or necrosed tooth.8afarzadeh, Hamid, and P. V. Abbott. “Review of pulp sensibility tests. Part I: general information and thermal tests.” International endodontic journal 43.9 (2010): 738-762.
-
Cold Test
A cold stimulus, such as ice, ethyl chloride spray, or CO2 snow, is applied to the tooth. A healthy pulp typically responds with a sharp, brief sensation that subsides when the stimulus is removed. In necrosed or dead pulp, the tooth will not give any response.9Peters, Donald D., J. Craig Baumgartner, and Lewis Lorton. “Adult pulpal diagnosis. I. Evaluation of the positive and negative responses to cold and electrical pulp tests.” Journal of Endodontics 20.10 (1994): 506-511.
-
Heat Test
This is less commonly used. In this test, the tooth is exposed to a heated gutta percha or hot water. Pain on stimulus indicates that the tooth is healthy, whereas no reaction indicates necrosis.
Electric Pulp Test
The Electric Pulp Testing (EPT) is another important diagnostic tool that evaluates the pulp’s vitality by applying a small electric current to the tooth. The EPT stimulates the nerve fibers within the pulp, and the patient reports whether they feel a tingling sensation.
- In a vital pulp, the patient will feel the sensation as the electric current stimulates the nerve fibers. The strength of the current required to elicit a response can provide insights into the degree of pulp vitality.
- A lack of response during an electric pulp test indicates that the pulp is non-vital, suggesting pulp necrosis.
Percussion & Palpation Tests
Dentists often percuss or palpate the tooth to check for signs of pain and tenderness. If the patient complains of pain, it indicates inflammation in the tooth or the surrounding area.
Radiographic Examination
X-rays assess the condition of the tooth’s root and surrounding bone. Radiographs can reveal signs of infection, such as periapical radiolucency, indicating an abscess or bone loss.
Cone Beam Computed Tomography (CBCT)
In complex cases, CBCT imaging may be used to provide a detailed view of the tooth and surrounding structures. This advanced imaging technique can help visualize the extent of infection and necrosis.
Treatment
Treating pulp necrosis aims to eliminate infection, preserve the tooth, and restore its function. The treatment plan depends on the degree of damage to the tooth. Some treatment options are as follows.
Root Canal Therapy
Dentists most commonly perform root canal procedure on necrosed teeth. They remove the non-vital dental pulp, cleanse the root canal, and fill it with a biocompatible material to restore the tooth’s function.
Endodontic Treatment
Sometimes dentists fail in root canal therapy, requiring them to retreat the tooth. In this procedure, they remove the previous filling, cleanse the root canal again, and reseal it.
Apicoectomy
This surgical procedure involves removing the root tip and any infected tissue, followed by sealing the root end to prevent further infection. Apicoectomy is typically performed when conventional root canal treatment is not sufficient to resolve the infection.
Pulp Capping
In cases of partial necrosis or reversible pulpitis, dentists may apply a protective dressing to the pulp to encourage healing and preserve its vitality. This conservative approach aims to avoid more extensive treatment if the pulp can recover.10Bergenholtz, Gunnar, et al. “Treatment of pulps in teeth affected by deep caries–A systematic review of the literature.” Singapore Dental Journal 34.1 (2013): 1-12.
Extraction
This is the last option if the tooth is damaged beyond repair. This is followed by replacement options such as dental implants, bridges, or dentures to restore function and aesthetics.
Conclusion
In conclusion, pulp necrosis whether partial or complete significantly impacts the tooth vitality. Correct diagnosis is crucial for treatment planning. Early diagnosis and prompt endodontic therapy are essential to manage necrotic pulp tissue and preserve oral health.
Refrences
- 1Yu, Christine, and Paul V. Abbott. “An overview of the dental pulp: its functions and responses to injury.” Australian Dental Journal 52 (2007): S4-S6.
- 2Andreasen, J. O. “Textbook and color atlas of traumatic injuries to the teeth.” Munksgard. Copenhagen 155 (1993): 172-173.
- 3Jafarzadeh, Hamid, and P. V. Abbott. “Review of pulp sensibility tests. Part I: general information and thermal tests.” International endodontic journal 43.9 (2010): 738-762.
- 4Bergenholtz, Gunnar. “Pathogenic mechanisms in pulpal disease.” Journal of Endodontics 16.2 (1990): 98-101.
- 55. Hargreaves, Kenneth M., Harold E. Goodis, and Franklin R. Tay, eds. Seltzer and Bender’s dental pulp. Batavia, IL, USA: Quintessence Pub., 2012.
- 6Nair, PN Ramanchandran. “Pathogenesis of apical periodontitis and the causes of endodontic failures.” Critical Reviews in Oral Biology & Medicine 15.6 (2004): 348-381.
- 7Hargreaves, Kenneth M., Harold E. Goodis, and Franklin R. Tay, eds. Seltzer and Bender’s dental pulp. Batavia, IL, USA: Quintessence Pub., 2012
- 8afarzadeh, Hamid, and P. V. Abbott. “Review of pulp sensibility tests. Part I: general information and thermal tests.” International endodontic journal 43.9 (2010): 738-762.
- 9Peters, Donald D., J. Craig Baumgartner, and Lewis Lorton. “Adult pulpal diagnosis. I. Evaluation of the positive and negative responses to cold and electrical pulp tests.” Journal of Endodontics 20.10 (1994): 506-511.
- 10Bergenholtz, Gunnar, et al. “Treatment of pulps in teeth affected by deep caries–A systematic review of the literature.” Singapore Dental Journal 34.1 (2013): 1-12.

