A Macular Pucker is an eye condition that causes distorted or wavy vision. People with this condition have mild symptoms and don’t need treatment. But if it makes daily activities difficult, you may need surgery to help you see clearly.
What is Macular Pucker?
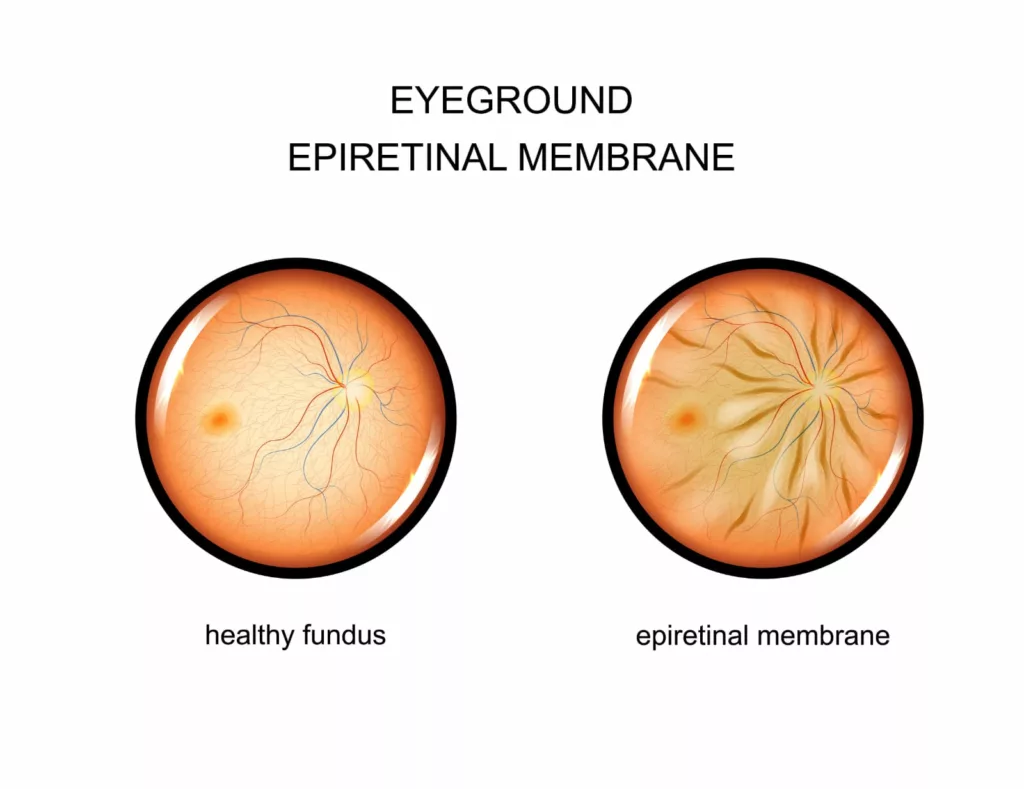
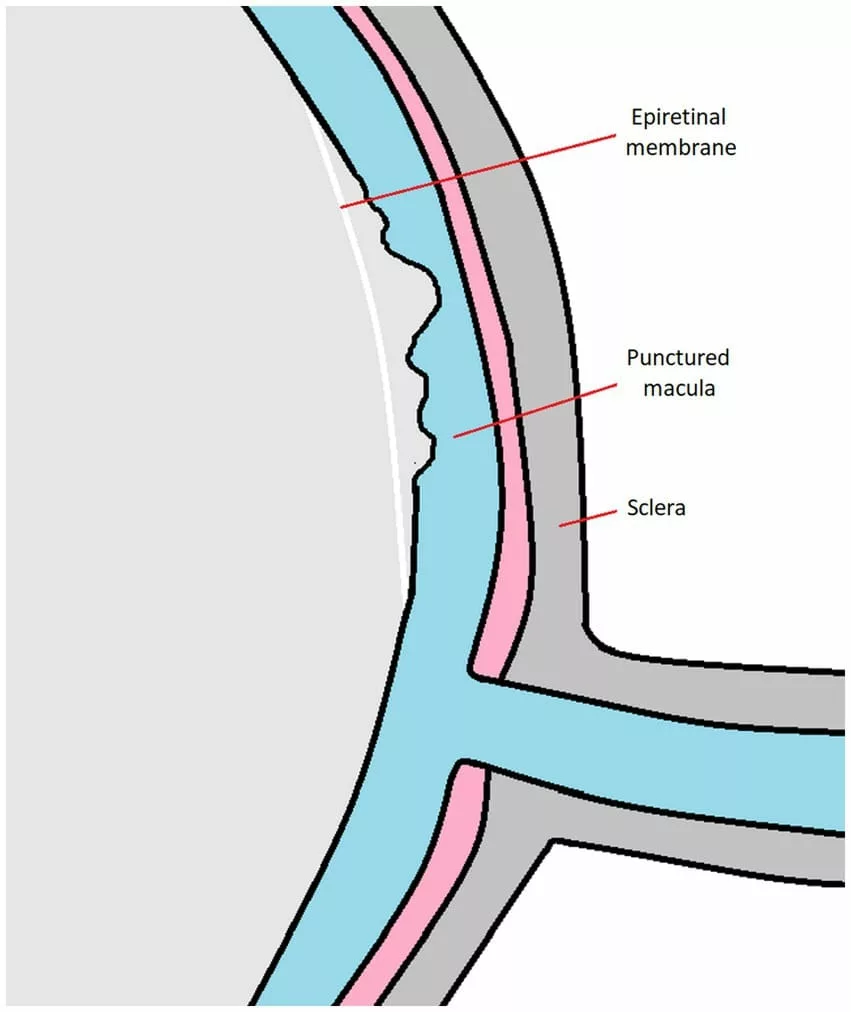
The epiretinal membrane (ERM), or macular pucker, is a pathological tissue that forms at the vitreoretinal interface—the junction between the vitreous body and the retina. This tissue formation is associated with various visual disturbances. ERM can develop idiopathically or secondary to several eye diseases, injuries, or retinal surgeries.1Dupas, B., Tadayoni, R., & Gaudric, A. (2015). Les membranes épirétiniennes maculaires [Epiretinal membranes]. Journal francais d’ophtalmologie, 38(9), 861–875. https://doi.org/10.1016/j.jfo.2015.08.004
Macular pucker is also known by other names, including preretinal membrane, cellophane maculopathy, surface wrinkling retinopathy, and pre-macular fibrosis.
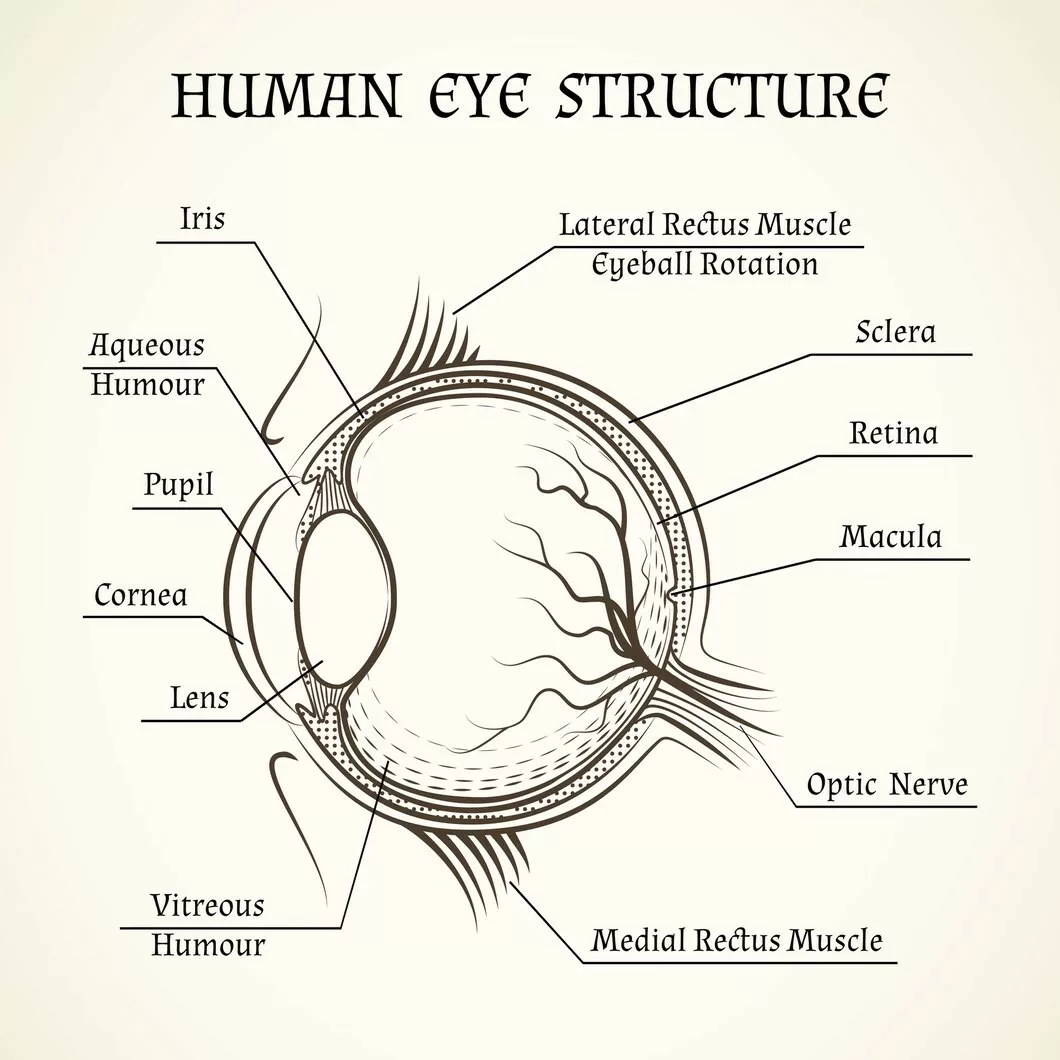
The Basic Structure of the Eye
The understanding of the eye structure will help you identify where a macular pucker occurs. The eye is the sensory organ responsible for helping you see the world. It has numerous parts that work together to accomplish the goal.
- Cornea: It is a thin and transparent covering in front of the eye. It lets the light enter your eyes.
- Sclera: The white part of your eye is the sclera. It maintains the round shape of your eye.
- Pupil: The pupil is the black part of your eye. It controls the amount of light entering your eye by narrowing and widening it.
- Lens: It helps light entering your eye fall on the retina.
- Vitreous body: It is a clear and transparent gel that fills the space between the lens and the retina and gives the eye shape.
- Retina: It is a thin layer at the back of your eyes. It has light-sensitive cells called rods (which help you see in low light) and cons (which help you see colors). When light falls on the retina, it changes into signals your brain receives and becomes an image.
- Macula: This is a small central part of the retina. It is responsible for vision and helps you see colors and fine details.
What causes Macular Pucker?
A macular pucker occurs when a scar tissue layer appears on the eye’s macula, a light-sensitive layer located in the retina’s center. The macula makes your vision sharp and central for daily activities like reading, writing, driving, and paying attention to fine details. When a macular pucker condition occurs, it makes your vision wavy and distorted.
With advancing age, this condition appears due to wrinkling or shrinkage of the vitreous gel. It is a transparent gel inside your eye that gives your eye a round shape. The vitreous gel has millions of fine fibers connected to your retina. This vitreous gel shrinks and pulls away from your retina surface as you age. This condition is called vitreous detachment, which is a natural process. The shrinking of vitreous gel usually does not affect the retina; however, sometimes, it causes micro damage to the retina’s surface.
A scar tissue called epiretinal membrane begins appearing on the retinal surface as a healing process. This scar tissue is strongly attached to the retina’s surface, and with time, this scar tissue contracts and wrinkles slowly, causing the retina to wrinkle without affecting central vision. But if this scar tissue is made on the macula, its shrinkage will affect your central vision and make straight lines look wavy and crooked.
Symptoms of a Macular Pucker
The main symptom of this condition is blurry and distorted vision, with straight lines appearing bent and wavy (also known as metamorphopsia). Vision loss from this condition varies from no vision loss to severe loss.
In addition to distorted vision, you may feel double vision, or the image from one eye may appear larger than the other. There may also be a gray area or blind spot in the center of your vision.
You might notice a decline in visual clarity that eyeglasses cannot correct. However, this condition only affects central vision, leaving your peripheral (side) vision unaffected.
Am I at risk of a Macular Pucker?
The most common risk for macular pucker is advancing age, but if you have any other eye problem, you may be at risk of developing the condition. These conditions include;
- History of retinal detachment
- Presence of the swelling in the eye
- Previous surgery of the eye, including cataract eye surgery
- Infection
- Serious damage to the eye from injury or trauma
- Blood vessel problems in the retina
- Diabetes-related retinopathy
- Retinal tear (damage to the retina)
How is a Macular Pucker Diagnosed?
Your eye doctor will take a thorough medical history and ask a few questions about your symptoms. Then, he will do a detailed eye examination. He will put eye drops to dilate the eyes (widen the eyes) and examine your retina.
During the eye examination, your doctor will use light and magnifiers to examine your eyes closer. He may also use the following eye tests to diagnose the condition.
- Amsler Grid Eye Test: This test uses a page of little squares made from horizontal and vertical lines to check for distorted vision.
- Optical Coherence Tomography: This imaging method takes pictures of the retina and macula to study the condition.
Treatment of the Macular Pucker
The treatment for the macular pucker depends on the symptoms. If you have mild symptoms, you might not need any treatment. However, the invasive and non-invasive treatment options include;
Non-invasive Treatment:
- Your doctor may change your eyeglasses and contact lenses to improve vision.
- He may suggest you use bifocals if you are reading or doing any work that requires a closer look.
- If you have other eye problems, he may also advise you on eye drops, medication, or laser surgery treatments.
Invasive Treatment:
If your symptoms are severe and making it difficult to see, your doctor may suggest surgery called vitrectomy with membranectomy. The main way of treating the macular pucker is with this surgery.2Fung, A. T., Galvin, J., & Tran, T. (2021). Epiretinal membrane: A review. Clinical & experimental ophthalmology, 49(3), 289–308. https://doi.org/10.1111/ceo.13914 This outpatient surgery is done under local anesthesia. Your doctor will remove the scar and vitreous tissue from the macula during this surgery. This will help the macula get back to its original position. With this surgery, your vision will slowly improve, but your sight may not be as good as before the macula pucker.
After the surgery, you will wear an eye patch for a few days or a week to protect your eye. Your eye doctor may also give you drops to protect your eye from infection.
How long will it take to see better after Surgery?
After the vitrectomy, you may experience imperfect vision for a few days, and your eye may become tender and irritated for a few days. You will need 2-3 months after the surgery to fully enjoy better and improved vision.
What are some Complications of the Surgery?
The surgery is minimally invasive; hence, it is a safe treatment for improving vision.3Inoue, M., & Kadonosono, K. (2014). Macular diseases: epiretinal membrane. Developments in ophthalmology, 54, 159–163. https://doi.org/10.1159/000360462 The surgery team will monitor vigilantly to avoid any complications, but there is always a risk during the surgery. These complications may include:
- Bleeding in the eye
- Retinal tear or detachment
- Cataract getting worse
- Eye infection
- Macular hole
- Glaucoma (increased pressure in the eye)
How successful is a Vitrectomy?
Vitrectomy to repair macular pucker improves vision quality and reduces metamorphopsia in the long term. However, sometimes cataracts can develop as a complication, reducing vision.4Crafoord, S., Jemt, M., Carlsson, J. O., Stenkula, S., & Shanks, G. (1997). Long‐term results of macular pucker surgery. Acta Ophthalmologica Scandinavica, 75(1), 85-88. If the condition is left untreated, it may further affect your visual function.5Chua, P. Y., Sandinha, M. T., & Steel, D. H. (2022). Idiopathic epiretinal membrane: progression and timing of surgery. Eye (London, England), 36(3), 495–503. https://doi.org/10.1038/s41433-021-01681-0.
Prognosis of the Macular Pucker
Most cases of macular pucker don’t need treatment. Your doctor will set up follow-ups to monitor eye vision and eye health. Although the condition may cause some difficulty, it is unlikely to cause blindness.
How can I prevent getting a Macular Pucker?
There is no way to prevent macular pucker. It is an age-related condition, and sometimes, the cause is unknown. However, avoiding diabetic-related eye problems and eye trauma can prevent the risk of developing it.
Macular Pucker Vs. Macular Degeneration
Both of these conditions are different, yet they both affect the macula, the central part of the retina. Macular pucker involves scar tissue forming on the macula, causing visual distortions and central vision loss that is generally stable and less progressive.
Age-related macular degeneration (AMD) is primarily associated with aging and shares risk factors with macular pucker, such as being over 60 years old. Other risk factors for AMD include smoking, genetic markers, high blood pressure, and obesity.6Ayoub, T., & Patel, N. (2009). Age-related macular degeneration. Journal of the Royal Society of Medicine, 102(2), 56-61. https://doi.org/10.1258/jrsm.2009.080298. AMD is the leading cause of vision loss in adults, affecting nearly 11 million people in the US.7National Eye Institute. (n.d.). Age-related macular degeneration. Retrieved from https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/age-related-macular-degeneration
AMD results from the breakdown or damage of the macula (dry AMD) or the growth and leakage of abnormal blood vessels (wet AMD), leading to fast and progressive vision loss in its late stages.
Are the Macular Pucker and Macular Hole the same?
No, a macular pucker occurs when a layer of tissue appears on the macula, whereas a macular hole occurs when a tear of the macula occurs due to ocular trauma. It can also be idiopathic, affecting elderly people. Both affect central vision, and patients with these conditions complain of metamorphopsia.8La Cour, M., & Friis, J. (2002). Macular holes: classification, epidemiology, natural history and treatment. Acta Ophthalmologica Scandinavica, 80(6), 579-587.
Conclusion
In conclusion, macular pucker is a common eye condition in older adults, characterized by the formation of scar tissue on the macula, leading to distorted vision. While symptoms are often mild and manageable without treatment, severe cases affecting daily activities may require vitrectomy surgery to restore vision.
Refrences
- 1Dupas, B., Tadayoni, R., & Gaudric, A. (2015). Les membranes épirétiniennes maculaires [Epiretinal membranes]. Journal francais d’ophtalmologie, 38(9), 861–875. https://doi.org/10.1016/j.jfo.2015.08.004
- 2Fung, A. T., Galvin, J., & Tran, T. (2021). Epiretinal membrane: A review. Clinical & experimental ophthalmology, 49(3), 289–308. https://doi.org/10.1111/ceo.13914
- 3Inoue, M., & Kadonosono, K. (2014). Macular diseases: epiretinal membrane. Developments in ophthalmology, 54, 159–163. https://doi.org/10.1159/000360462
- 4Crafoord, S., Jemt, M., Carlsson, J. O., Stenkula, S., & Shanks, G. (1997). Long‐term results of macular pucker surgery. Acta Ophthalmologica Scandinavica, 75(1), 85-88.
- 5Chua, P. Y., Sandinha, M. T., & Steel, D. H. (2022). Idiopathic epiretinal membrane: progression and timing of surgery. Eye (London, England), 36(3), 495–503. https://doi.org/10.1038/s41433-021-01681-0.
- 6Ayoub, T., & Patel, N. (2009). Age-related macular degeneration. Journal of the Royal Society of Medicine, 102(2), 56-61. https://doi.org/10.1258/jrsm.2009.080298.
- 7National Eye Institute. (n.d.). Age-related macular degeneration. Retrieved from https://www.nei.nih.gov/learn-about-eye-health/eye-conditions-and-diseases/age-related-macular-degeneration
- 8La Cour, M., & Friis, J. (2002). Macular holes: classification, epidemiology, natural history and treatment. Acta Ophthalmologica Scandinavica, 80(6), 579-587.