Galactosemia is a rare but serious genetic metabolic condition resulting from a deficiency in one of the enzymes needed to metabolize galactose, a simple sugar found in milk and dairy products. The most common form, classic galactosemia, results from a deficiency of galactose-1-phosphate uridyltransferase (GALT).
Despite its rarity, affecting approximately 1 in 30,000 to 60,000 live births, early diagnosis through newborn screening and immediate dietary intervention are crucial to prevent life-threatening complications. Without treatment, affected infants may develop jaundice, hepatomegaly, liver failure, sepsis (often due to E. coli), cataracts, and developmental delays.
With early identification and strict lifelong adherence to a galactose-restricted diet, most children can avoid acute complications and lead relatively healthy lives, although some may still experience long-term issues such as speech delays, cognitive difficulties, or reproductive challenges.1life.Berry, G. T. (2023). Classic galactosemia. In M. P. Adam, G. M. Mirzaa, R. A. Pagon, et al. (Eds.), GeneReviews®. University of Washington, Seattle.
What Causes Galactosemia?
Mutations in the enzymes involved in the breakdown of galactose result in galactosemia. Normally, the body uses a range of chemical reactions to convert galactose into glucose. When one of these enzymes is absent or in limited quantities, galactose and its derivatives build up in the blood and become poisonous.2Elsas, L. J., & Lai, K. (1998). The molecular biology of galactosemia. Genetics in Medicine, 1(2), 40–48.
The Enzymes Involved:
- GALT (Galactose-1-phosphate uridylyltransferase): The enzyme most frequently involved in classic galactosemia. The primary factor is the mutations in the GALT gene.
- GALK1 (Galactokinase): Affects the first step of galactose metabolism.
- GALE (UDP-galactose-4-epimerase): Affects the last step of the pathway.
- GALM (Galactose mutarotase): Recently identified, it is responsible for converting beta-D-galactose to alpha-D-galactose.
Classic galactosemia is caused by a complete or near-complete deficiency of the GALT enzyme, which causes an accumulation of galactose-1-phosphate, a harmful metabolite that damages the liver, kidneys, brain, and eyes.3Berry, G. T. (2023). Classic galactosemia. In M. P. Adam, G. M. Mirzaa, R. A. Pagon, et al. (Eds.), GeneReviews®. University of Washington, Seattle.
Galactosemia Symptoms in Infants and Adults
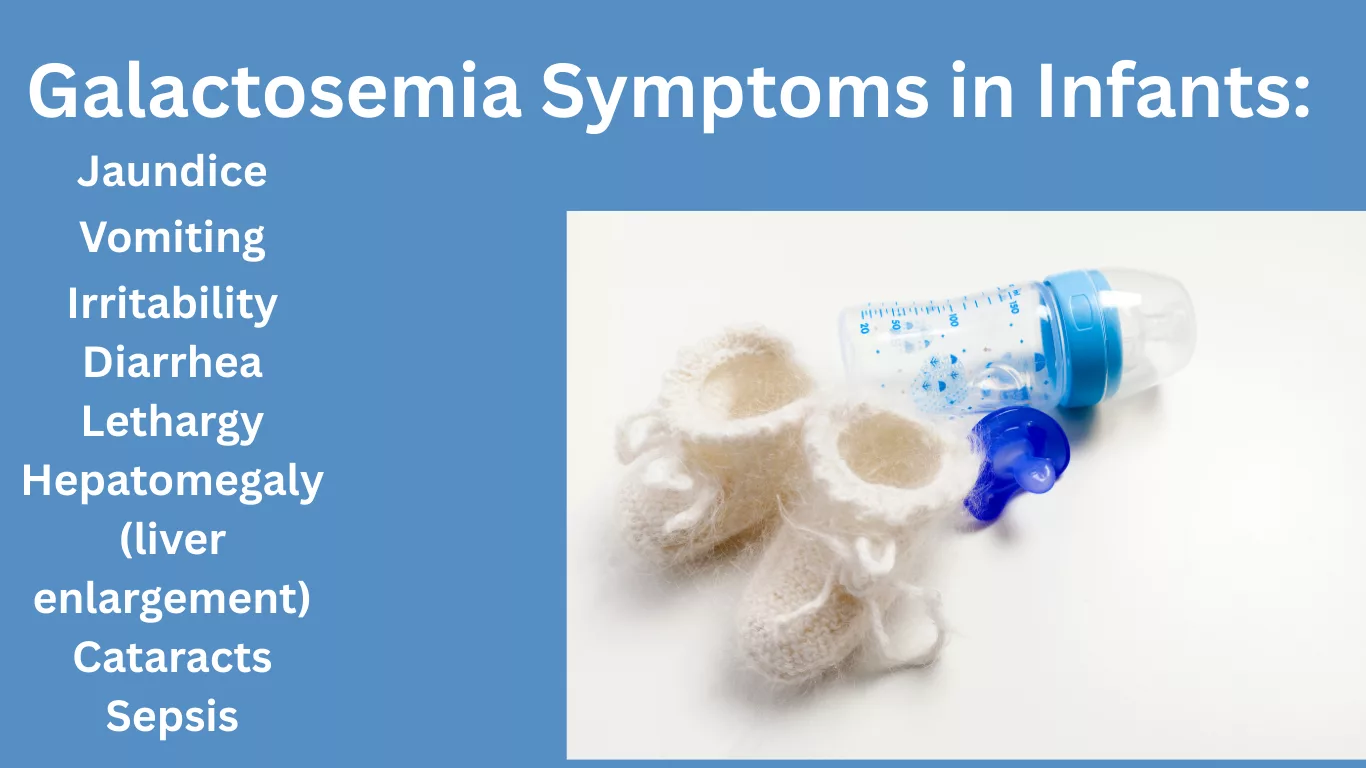
In Newborns & Infants:
Infants with galactosemia typically begin showing symptoms within the first few days after consuming milk or formula containing lactose. The most common clinical features include:4Baker, M. W., & Comeau, A. M. (2020). Newborn screening: Beyond PKU. Current Opinion in Pediatrics, 32(6), 731–737.
- Jaundice (yellowing of the skin and eyes)
- Vomiting
- Poor feeding or weight gain
- Irritability
- Diarrhea
- Lethargy
- Hepatomegaly (liver enlargement)
- Cataracts
- Sepsis (especially E. coli infections)
In Older Children & Adults:
Even with early dietary therapy, patients may develop chronic complications.
- Speech and language delay
- Learning disabilities
- Motor skill deficiency
- Ovarian failure in women
- Decreased bone density
Notably, early symptoms may mimic other neonatal conditions, and hence, early screening is critical.
Types of Galactosemia:
Galactosemia occurs in several forms based on the enzyme involved and the severity of the deficiency:5Fridovich-Keil, J. L. (2013). Galactosemia: The good, the bad, and the unknown. Journal of Cell Physiology, 228(11), 2477–2486.
Classic Galactosemia (Type I):
- Needs a strict lifelong galactose-free diet.
- Caused by GALT mutations.
- Most severe form.
Duarte Variant Galactosemia:
- Partial GALT enzyme activity (up to 25%).
- Milder symptoms; often no long-term consequences.
- There is some controversy regarding the need for dietary restrictions.
Galactokinase Deficiency (Type II):
- Impacts the GALK1 enzyme.
- Generally, causes cataracts, but not liver or brain damage.
Galactose Epimerase Deficiency (Type III):
- Affects the GALE enzyme.
- Ranges from benign to severe.
Each form requires specific testing to determine the correct treatment plan.
How Is Galactosemia Diagnosed?
Newborn Screening:
In many countries with a newborn screening program, galactosemia is routinely detected through the heel-prick blood test.6Bosch, A. M. (2006). Classical galactosaemia revisited. Journal of Inherited Metabolic Disease, 29(4), 516–525.
Initial screening includes:
- Measurement of GALT (galactose-1-phosphate uridylyltransferase) enzyme activity
- Elevated levels of galactose and galactose-1-phosphate in the blood
Confirmatory Testing:
If the screening test is abnormal, confirmatory testing should follow:
- Quantitative GALT enzyme assay in red blood cells
- Molecular genetic testing to identify pathogenic variants in genes associated with galactose metabolism:
– GALT (classic galactosemia)
– GALK1 (galactokinase deficiency)
– GALE (epimerase deficiency)
– GALM (mutarotase deficiency)
Early diagnosis is critical to avoid complications. If screening test results are positive, parents must stop lactose-containing formulas immediately.7Berry, G. T. (2023). Galactosemia: Symptoms, causes, and diagnosis. In R. A. Hoppin & D. M. Nathan (Eds.), UpToDate.
Treatment & Management: Living Well with Galactosemia
Lifelong Dietary Management:
The backbone of treatment for classic galactosemia is a lifelong, strict dietary restriction. This means that both galactose and lactose need to be completely removed from the diet as people with this condition are unable to metabolise these sugars appropriately. Here are some of the major dietary recommendations:
- Dairy Products: Avoid all dairy products as they are the primary sources of lactose. This covers milk, cheese, yogurt, ice cream, butter, and everything that has these ingredients.
- Infants need to be fed alternative formulas free from lactose or galactose. These may consist of soy-based formulas or elemental formulas tailored for metabolic disorders.
- As the child matures, total avoidance of all lactose-containing foods remains critical, and careful reading of labels is essential to avoiding their inadvertent consumption.8Komrower, G. M. (2004). The complications of galactosaemia. Archives of Disease in Childhood, 89(4), 361–364.
Monitoring & Follow-Up:
Patients need to have regular medical follow-ups to monitor for the progression of the disease and to prevent complications. Monitoring recommendations include:
- Routine blood tests for galactose-1-phosphate levels in red blood cells help gauge metabolic control.
- Developmental screenings to identify and respond to possible delays in cognitive or physical development.
- Because people with galactosemia often have speech and motor skill problems, speech and occupational therapy may be needed.
- Regular bone density scans should be performed to screen for osteopenia or osteoporosis, both of which can develop from prolonged dietary restrictions and hormonal problems.
Supplementation:
Omitting dairy products can bring certain nutritional deficiencies. It is suggested as follows:
- As dairy is a major source of calcium and Vitamin D, supplementation is also necessary.
- Hormonal treatment might be needed because female patients may have primary ovarian insufficiency, which is a frequent long-term complication of galactosemia. Hormone replacement therapy can induce and maintain puberty. 9Welling, L., Bernstein, L. E., Berry, G. T., et al. (2017). The International Galactosemia Network consensus guidelines for the diagnosis, treatment, and follow-up of galactosemia. Journal of Inherited Metabolic Disease, 40(2), 171–176.
Supportive Care:
Beyond diet and monitoring is the comprehensive care for galactosemia. Supportive services include:
- Genetic counseling: To understand the hereditary nature of the condition, genetic counseling is very necessary to assess the risk of recurrence in future pregnancies, and options for prenatal diagnosis in affected females.
- Access to support groups: Experienced nutritionists or dietitians can provide emotional support, practical advice for managing dietary restrictions, and updated guidance on safe food choices and supplements.
With careful management — and a galactose-free diet — many children with galactosemia live into adulthood with good health and normal cognitive function
Galactosemia vs. Lactose Intolerance
Although both conditions represent adverse responses to milk, they differ widely regarding cause, timing, severity, treatment, and complications. Appreciating those variances can be critical for the timely and appropriate care, particularly in infants.10Coelho, A. I., Rubio-Gozalbo, M. E., Vicente, J. B., & Rivera, I. (2017). Sweet and sour: An update on classic galactosemia. Journal of Inherited Metabolic Disease, 40(3), 325–342.
Cause:
- Galactosemia results from a genetic deficiency of the enzyme galactose-1-phosphate uridylyltransferase (GALT), which is needed to metabolize galactose (a component of lactose). The buildup of toxic substances in the body results in this.
- Lactose Intolerance: A result of a deficiency in lactase, the enzyme that digests lactose, the sugar in milk. Lactose that isn’t fully digested ferments in the colon and leads to gastrointestinal symptoms.
Onset:
- Galactosemia: Symptoms usually start in the first few days of life, when the newborn starts to feed on breast milk or formula. Poor feeding, vomiting, jaundice, lethargy, and failure to thrive can be the initial signs to notice.
- Lactose Intolerance: Generally, it begins later in life (late childhood, adolescence, or adulthood). It can happen slowly and be brought on by gut illness or age. Rarely seen in infants.
Severity:
- Galactosemia: This is a condition that can be life-threatening if not treated early. The buildup of galactose and its metabolites can cause damage to the liver, kidneys, brain, and other organs.
- Lactose Intolerance: Not much harm, but causes bloating, cramps in the abdomen, gas, and diarrhea after eating dairy. Does not lead to organ damage or severe health issues.
Management:
- Galactosemia: Needs a strict, lifelong elimination of all foods containing galactose and lactose. These include all milk and milk products and foods with occult lactose or galactose. Babies receive soy-based or elemental formulas. You require ongoing medical supervision.
- Lactose Intolerance: Managed by avoidance of lactose-containing food. Most can still tolerate a little dairy or take lactase enzyme supplements to help with lactose digestion.
Complications:
- Galactosemia: Galactosemia has life-threatening dangers if untreated. When exposed to galactose, one may cause liver malfunction, kidney damage, blood poisoning, clouding of the lenses in the eyes, delayed development, mental impairments, and ovarian dysfunction in women. Although treatment prevents additional injury, some permanent effects remain.
- Lactose Intolerance: In comparison, lactose intolerance primarily affects the gastrointestinal tract. Abstaining from a diet that excludes lactose avoids any medical problems or permanent impairment.
Importance of Accurate Diagnosis
- Distinguishing galactosemia from lactose intolerance proves crucial. Presuming the former to be the latter can be lethal, notably in newborns. Delayed intervention for galactosemia may result in irreparable damage or death.
- Galactosemia needs urgent medical care, including immediate dietary changes and metabolic surveillance.
- On the other hand, lactose intolerance seldom warrants clinical management and can often be self-managed without therapy. Correct diagnosis is paramount given their contrast in severity and management.11Clarke, J. T. R. (2006). A Clinical Guide to Inherited Metabolic Diseases (3rd ed.). Cambridge University Press.
Can Galactosemia be Prevented?
Currently, you can’t stop it from happening because it is a genetic disorder. But if you’re planning to have children, genetic screening can help evaluate your risk. You can be a carrier of the gene without exhibiting symptoms yourself.
Carriers can benefit from genetic counseling to understand the risks of being passed along to their children. Timely diagnosis is still the best tool we have to try to minimize complications, and nothing beats population-based newborn screening, as was done in the study.
Life Expectancy with Galactosemia
With early diagnosis and a galactose-free diet, many people with galactosemia lead long and healthy lives. But if organ damage already occurred before the diagnosis or treatment, it could affect the person’s long-term health. Ongoing medical monitoring helps detect and treat complications early.
Living with Galactosemia
For adults, living well with galactosemia includes a very strict galactose-free diet and regular health checks. Lactose or galactose-containing food must be avoided. This means not only all dairy products, but certain processed foods and even some medications that use lactose as a filler. Support groups are great for sharing recipes and keeping motivate12Lorey, F. W., Cunningham, G. C., & Robison, L. L. (2020). Newborn screening for galactosemia. National Newborn Screening and Global Resource Center.
The following are important Health Monitoring:
- Eye exams for cataracts
- Neurological assessments (ADHD, tremors, motor issues)
- Bone density testing
- Hormonal assessments, especially for women
Prenatal Testing
Prenatal screening is available, specifically for people with a known family heritage of galactosemia or when each parent has been verified as a carrier of the GALT gene mutation. There are two main approaches:
Carrier Screening (Preconception or Early Pregnancy):
Carrier screening involves a straightforward blood or saliva test to ascertain whether the expected parents carry mutations in the GALT gene. If the two parents are carriers, there is a 25% possibility with each pregnancy that the child will have galactosemia.
Prenatal Diagnostic Testing:
If both parents are validated carriers, prenatal diagnostic methods may be proposed:
- Chorionic Villus Sampling (CVS): Performed between 10 and 13 weeks of gestation, this test examines placental tissue for genetic anomalies.
- Amniocentesis: Generally done between 15 and 20 weeks of pregnancy, this test scrutinizes fetal DNA from amniotic fluid to check for the existence of galactosemia-causing mutations.
These prenatal tests can help families make informed decisions about pregnancy and prepare for early intervention if the baby is diagnosed with galactosemia.
Clinical Trials for New Treatment Options
Ongoing scientific research continues to pursue encouraging fresh remedies aimed toward bettering results and addressing long-lasting complications of galactosemia. These include:13Waggoner, D. D., Buist, N. R. M., & Donnell, G. N. (2023). Living with galactosemia. Galactosemia Foundation.
- Gene Therapy and Gene Editing: Scientists are correcting the faulty GALT gene using advanced gene-editing technologies such as CRISPR-Cas9.14Innovative Genomics Institute. (2023, March 17). CRISPR Clinical Trials: A 2023 Update. Retrieved from https://innovativegenomics.org/news/crispr-clinical-trials-2023/ The goal is to restore normal enzyme function, potentially delivering a lasting treatment.
- Enzyme Replacement Therapy (ERT): This approach involves substitution of the functional GALT enzyme in the body to compensate for the deficiency. ERT has shown success in other metabolic conditions and is currently undergoing investigation for galactosemia.
- Pharmacological Chaperones: Additionally, pharmacological chaperones, small molecules intended to stabilize the aberrant GALT enzyme, improving its function, which could prove particularly useful for individuals with partial enzymatic activity
- Substrate Reduction Therapy (SRT): ISRT aims to decrease the accumulation of toxic galactose metabolites by inhibiting enzymes involved in their production. Govorestat (AT-007), an aldose reductase inhibitor developed by Applied Therapeutics, has shown potential in reducing galactitol levels and improving clinical outcomes in pediatric patients with galactosemia. Despite these promising results, the U.S. Food and Drug Administration (FDA) issued a Complete Response Letter in 2024, citing deficiencies in the application and delaying its approval.
While dietary management remains the mainstay of treatment, these experimental therapies hold the potential to significantly improve quality of life and reduce complications in the future.
Take Away
In conclusion, galactosemia is a rare yet serious inherited metabolic disorder that requires prompt diagnosis and strict dietary management to prevent life-threatening complications. While lifelong lactose restriction remains the mainstay of treatment, ongoing research into gene therapy, enzyme replacement, and pharmacological interventions offers hope for more effective, long-term solutions. Early intervention, regular monitoring, and multidisciplinary care are key to improving quality of life and long-term outcomes for those affected.
Refrences
- 1life.Berry, G. T. (2023). Classic galactosemia. In M. P. Adam, G. M. Mirzaa, R. A. Pagon, et al. (Eds.), GeneReviews®. University of Washington, Seattle.
- 2Elsas, L. J., & Lai, K. (1998). The molecular biology of galactosemia. Genetics in Medicine, 1(2), 40–48.
- 3Berry, G. T. (2023). Classic galactosemia. In M. P. Adam, G. M. Mirzaa, R. A. Pagon, et al. (Eds.), GeneReviews®. University of Washington, Seattle.
- 4Baker, M. W., & Comeau, A. M. (2020). Newborn screening: Beyond PKU. Current Opinion in Pediatrics, 32(6), 731–737.
- 5Fridovich-Keil, J. L. (2013). Galactosemia: The good, the bad, and the unknown. Journal of Cell Physiology, 228(11), 2477–2486.
- 6Bosch, A. M. (2006). Classical galactosaemia revisited. Journal of Inherited Metabolic Disease, 29(4), 516–525.
- 7Berry, G. T. (2023). Galactosemia: Symptoms, causes, and diagnosis. In R. A. Hoppin & D. M. Nathan (Eds.), UpToDate.
- 8Komrower, G. M. (2004). The complications of galactosaemia. Archives of Disease in Childhood, 89(4), 361–364.
- 9Welling, L., Bernstein, L. E., Berry, G. T., et al. (2017). The International Galactosemia Network consensus guidelines for the diagnosis, treatment, and follow-up of galactosemia. Journal of Inherited Metabolic Disease, 40(2), 171–176.
- 10Coelho, A. I., Rubio-Gozalbo, M. E., Vicente, J. B., & Rivera, I. (2017). Sweet and sour: An update on classic galactosemia. Journal of Inherited Metabolic Disease, 40(3), 325–342
- 11Clarke, J. T. R. (2006). A Clinical Guide to Inherited Metabolic Diseases (3rd ed.). Cambridge University Press.
- 12Lorey, F. W., Cunningham, G. C., & Robison, L. L. (2020). Newborn screening for galactosemia. National Newborn Screening and Global Resource Center.
- 13Waggoner, D. D., Buist, N. R. M., & Donnell, G. N. (2023). Living with galactosemia. Galactosemia Foundation.
- 14Innovative Genomics Institute. (2023, March 17). CRISPR Clinical Trials: A 2023 Update. Retrieved from https://innovativegenomics.org/news/crispr-clinical-trials-2023/

