Granuloma Annulare is an inflammatory skin condition that generally affects the young. The skin inflammation presents as rashes, papules, raised patches, or lumps under the skin. The preferential sites for granuloma annulare include forearms, elbows, and feet. However, the disease can affect any part of the body. Studies show that the global prevalence of this disease is 0.1 to 0.4%. It can affect individuals of any age, but researchers have found a disease preference for women younger than 30 years of age.1Schmieder, S. J., Harper, C. D., & Schmieder, G. J. (2017). Granuloma annulare. Moreover, patients with comorbidities (such as thyroid disorders, diabetes, etc.) have a greater chance of developing granuloma annulare.
What Is Granuloma Annulare (GA)?
Also known as necrobiotic papulosis, granuloma annulare is a dermatological disorder that presents as a discolored rash or papules in otherwise normal individuals. These growths are benign, i.e., non-cancerous. Histological examination of the plaques/papules reveals the growth’s necrobiotic nature (physiologic death of skin cells). Patients report having raised bumps/papules that form a ring (thus the name “annulare” which means “ring-shaped”). The skin in the center of the raised bumps can be normal or sunken.
Types Of Granuloma Annulare
Generally, granuloma annulare has five types. In most cases, one predominant type is present in a patient. However, more than one type of granuloma annulare can affect you at one time.
Localized Granuloma Annulare:
As the name indicates, the formation of papules is limited to one area of the skin. The localized type presents as a circular rash. This is the most common form of disease that is highly prevalent in the US.2Barbieri, J. S., Rodriguez, O., Rosenbach, M., & Margolis, D. (2021). Incidence and prevalence of granuloma annulare in the United States. JAMA dermatology, 157(7), 824-830. Localized granuloma annulare responds well to topical treatment.
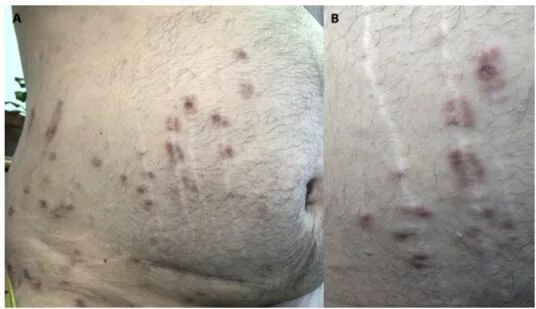
Generalized Granuloma Annulare:
Another common type of necrobiotic papulosis is the generalized or disseminated type. Disseminated granuloma annulare covers a broader area of the skin. There should be at least ten widespread annular papules to call it disseminated GA.3Thornsberry, L. A., & English, J. C. (2013). Etiology, diagnosis, and therapeutic management of granuloma annulare: an update. American journal of clinical dermatology, 14, 279-290. A generalized rash can completely cover your forearm or hand. In addition to the coverage, you can appreciate a greater concentration and intensity of the rash.
This subtype of granuloma annulare is generally more severe and does not respond to conventional therapies. Some clinicians believed there was a link between generalized GA and cancer. However, a 2019 study concluded no correlation exists between malignancy and generalized granuloma annulare.4Gabaldón, V. H., & Haro-González-Vico, V. (2019). Lack of an association between generalized granuloma annulare and malignancy: A case-control study. Journal of the American Academy of Dermatology, 80(6), 1799-1800.
Patch Granuloma Annulare:
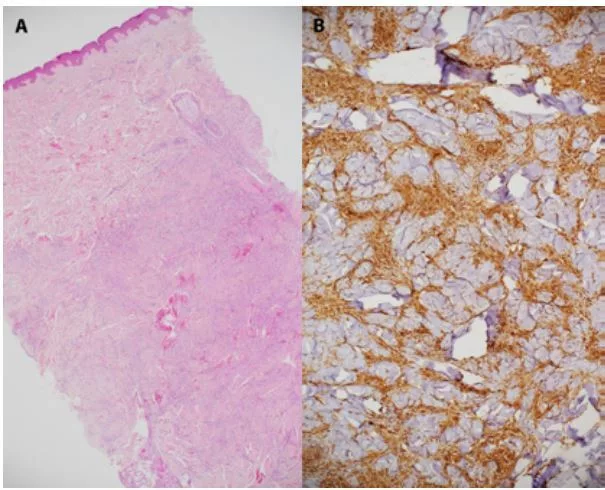
This is a less common type of GA. Purple-red (violaceous-erythematous) patches form on the extremities and are present on both sides of the body (bilateral presentation). You may find flat rash areas in skin patches. Histopathologically, it resembles interstitial mycosis fungoides (a variant of lymphoma). Therefore, proper diagnosis is important.5Khanna, U., & North, J. P. (2020). Patch‐type granuloma annulare: an institution‐based study of 23 cases. Journal of Cutaneous Pathology, 47(9), 785-793.
Perforating Granuloma Annulare:
Patients in the perforating type suffer from painful bumps that crust over time. The papules can attach via umbilicals (cords), i.e., umbilicated papules. Clinicians have noted localized and generalized forms of painful perforating GA. However, the condition is rare. 6Pap, N., Bradamante, M., & Ljubojević-Hadžavdić, S. (2019). Localized perforating granuloma annulare. Acta Dermatovenerologica Croatica, 27(1), 33-33. This type mostly affects the fingers of the hands.
Subcutaneous Granuloma Annulare:
As the name indicates, lumps of disease form underneath the skin. Though rare, subcutaneous granuloma annulare is most commonly seen in the pediatric population. Young females are most prone to developing subcutaneous GA. The most affected sites include the lower legs, feet, and scalp.7Endo, Y., Sekiguchi, A., Motegi, S. I., & Ishikawa, O. (2020). Subcutaneous granuloma annulare on the heel: a case report and review of the Japanese published work. The Journal of Dermatology, 47(6), 677-679.
There is also an atypical form of the disease that causes a rash in unusual locations such as the palm and face (and ears). It spreads on areas exposed to light, i.e., a photosensitive distribution.
Symptoms Of Granuloma Annulare
The symptomatic presentation of the disease is different for the various types. The following are the most common symptoms of granuloma annulare:
Localized GA
In the initial stages, you will notice a few small bumps that later merge to form a circular rash. The most common site in children is the knuckles (it affects the fingers of both hands). Patients have small individual circles of rash that merge to form one big circle whose center is depressed. The color of the rash is the same as that of the skin or may vary from purple to red.
Generalized GA
Most patients complain of papules over a large skin area. These papules are present in the armpits and groin and have a symmetrical arrangement. Over time, small bumps/papules merge to form a large discolored area. The bumps lack any coloration. You can appreciate the raised, discolored areas on ten (or more) different skin locations.
Patch GA
Red to reddish-brown rash areas are most commonly seen in the patch form. The rash appears on the hands and feet of both sides of the body. It may involve large areas of skin.
Perforating GA
This type starts with forming small, scaly bumps that itch and pain. Generally, there are multiple painful bumps on patients’ fingers (and hands). These yellow-colored bumps may leak fluid. Dermoscopic examination reveals perforations in the papules. As the disease progresses, these widespread bumps join together to form large areas of rashes.
Subcutaneous GA
Patients report small, painless lumps under the skin. The rapid growth of the firm and round lumps alarms many patients. These rubbery nodules on the fingertips, shins, and scalp mimic rheumatoid nodules. The lumps range in color from colorless to red-pink.
What Causes Granuloma Annulare?
The exact cause of this granulomatous skin condition is unknown. However, some researchers suggest a link between an immune response and the disease. Healthcare providers believe it may be a delayed hypersensitivity reaction to a trigger that causes skin inflammation. A delayed hypersensitivity reaction is an immune-mediated response in which the skin tries eliminating a foreign antigen. Specialized chemical structures i.e., tumor necrosis factor alpha (TNFɑ) mediate skin inflammation in response to a trigger.
There are numerous triggers for granuloma annulare, including:
Skin Trauma/Lesions:
Local trauma to the skin is a major trigger in pediatric GA.8Albert, M., Maruani, A., & Leducq, S. (2023). Clinical Manifestations and Management of Pediatric Granuloma Annulare: A Systematic Review. The Journal of Pediatrics. Certain skin lesions (such as insect bites) may also contribute to GA.
Infections:
Several infections such as Epstein bar virus (EBV), hepatitis C, HIV infection, and even SARS-CoV (COVID infection) can trigger GA.9Monte‐Serrano, J., García‐Gil, M. F., García‐García, M., Casas‐Flecha, I., Matovelle‐Ochoa, C., & Ara‐Martín, M. (2021). Granuloma annulare triggered by SARS‐CoV‐2 infection: Immunohistochemical staining. Dermatologic Therapy, 34(3).
Comorbidities:
Systemic conditions such as diabetes mellitus, autoimmune thyroiditis, and hyperlipidemia can trigger granuloma annulare.10Fornons-Servent, R., Bauer-Alonso, A., Llobera-Ris, C., Penín, R. M., & Marcoval, J. (2022). Granuloma annulare: a case-control study of possible associated diseases. Dermatology Practical & Conceptual, 12(4).
Certain Medicinal Drugs:
Medicines like allopurinol can trigger granulomatous skin inflammation.
Stress/Anxiety:
An onset of psychiatric comorbidity can lay the foundation for granuloma annulare.11Joshi, T. P., Chen, V., Dong, J. L., Golden, K., Iacobucci, A., Lim, Y., … & Duvic, M. (2022). Psychiatric comorbidities associated with granuloma annulare: a case-control study in the All of Us database. Journal of the American Academy of Dermatology, 87(3), e119-e120.
Granuloma Annulare Diagnosis
Diagnosing skin conditions can be tricky at times. However, granuloma annulare is not that hard to diagnose, thanks to its characteristic appearance. The initial investigation involves a thorough physical examination of the lesions on the skin by the doctor.
In most cases, a doctor performs a skin biopsy. This involves taking a small part of the affected skin and visualizing it under the microscope. Under magnification, the skin lesions appear necrobiotic and show regions of collagen degeneration. The disintegrated part is surrounded by inflammatory cells.
Differential Diagnosis (DD)
Due to similarity in appearance, granuloma annulare can be mistaken for several other skin pathologies. The most common differential diagnoses for GA are:
Granuloma Annulare Vs. Ringworm (Tinea)
Many GA patients self-diagnose themselves as ringworm patients. Tinea corporis is a fungal skin infection that presents like GA. Like GA, patients experience erythematous (red) papules/plaques on the skin with good demarcations. The edge of the lesion may be scaly or raised. In one case, a 3-year-old was declared to be a persistent ringworm patient by her mother. Careful examination of the skin lesions revealed her to be a localized and subcutaneous GA patient. 12Choe, C. S., Hao, L. M., & Mancini, A. J. (2023). Taking the “Worm” out of Ringworm: A Different Annular Rash in Children. The Journal of Pediatrics, 260. Therefore, a skin biopsy is important to rule out ringworm infection. Ringworm rash is generally scalier than granuloma annulare.
Other DDs for GA include:
- Psoriasis
- Discoid eczema
- Actinic granuloma annulare
- Erythema annulare centrifugum
- Necrobiotic lipoidica diabetricorum
- Perforating collagenosis
- Rheumatoid nodules
Is It Contagious?
No, granuloma annulare is not contagious and can’t spread through skin-to-skin contact.
Granuloma Annulare Treatment
In most cases, GA goes away independently and does not require treatment. Usually, the period for complete disappearance of lesions is two years. However, the recurrence of the rash remains a major issue.
The following treatment modalities are proven to be beneficial in the management of granuloma annulare:
Medications
Various medications are employed to shrink and resolve the rash. Dermatologists prescribe local or systemic therapy depending on the condition severity, type of GA, and patient’s age.
Topical Application
Physicians prefer treating GA with corticosteroid ointments first. But most cases require intralesional steroid injections to amp up healing. Calcineurin inhibitors such as tacrolimus and pimecrolimus are also advised to patients. Several individuals report positive outcomes with topical application of pimecrolimus and tacrolimus.13Lukács, J., Schliemann, S., & Elsner, P. (2015). Treatment of generalized granuloma annulare–a systematic review. Journal of the European Academy of Dermatology and Venereology, 29(8), 1467-1480.
Additionally, a skin wart cream i.e., Imiquimod 5% can help with GA. This particular cream can push annular lesions/plaque to remission with significant improvements in pain.14Wang, J., & Chen, W. Y. (2021). Imiquimod 5% Cream for an Annular Plaque with Progressive Pain on the Right Distal Arm in the Cubital Fossa: Acquired Tufted Angioma. Clinical, Cosmetic and Investigational Dermatology, 855-858. Isotretinoin cream is reserved only for refractory GA patients due to adverse effects.15Looney, M., & Smith, K. M. (2004). Isotretinoin in the treatment of granuloma annulare. Annals of Pharmacotherapy, 38(3), 494-497.
Systemic Therapy
Your doctor may try different drugs to get the best results. The most commonly prescribed systemic drug is hydroxychloroquine. It is an anti-malarial drug that has shown positive effects over time.16Grewal, S. K., Rubin, C., & Rosenbach, M. (2017). Antimalarial therapy for granuloma annulare: results of a retrospective analysis. Journal of the American Academy of Dermatology, 76(4), 765-767.Furthermore, certain drugs, including methotrexate, dapsone, potassium iodide, pentoxifylline, and isotretinoin, have been tested but have limited scope. Biologics (particularly TNF-α inhibitors) used in treating auto-immune disorders may also be a part of the regimen. However, there is limited research to advocate long-term, definitive use of biologics in GA management. Supplementation via Vitamin E tablets also seems to improve skin conditions.
Phototherapy (PUVA)
PUVA is a light therapy that combines Psoralen (P) and Ultraviolet radiation type-A (UVA). Psoralen is an anti-psoriatic drug taken orally. This very drug makes the skin pathology more sensitive to light therapy. After the drug is administered, UV light is shone onto the skin, causing the growth of affected skin cells to regress. As it combines chemical and light therapies, the modality is also known as photochemotherapy. Studies show that PUVA and PUVB (with UV-B light) help achieve satisfactory remission of generalized GA.17Cunningham, L., Kirby, B., Lally, A., & Collins, P. (2016). The efficacy of PUVA and narrowband UVB phototherapy in the management of generalized granuloma annulare. Journal of Dermatological Treatment, 27(2), 136-139.
Cryotherapy
In cryotherapy, the doctor halts the growth of an annular rash by freezing the affected area. This is done with the help of specialized instruments and equipment.
Laser Therapy
Treatment with controlled lasers aims to prevent the rash from spreading while decreasing inflammation. Excimer laser and pulsed dye lasers are commonly used in GA treatment.

How To Care For Your Skin?
Though you can’t prevent GA from developing, you can try to alleviate the effects. Patients can adopt some simple home remedies to keep the symptoms minimal. A mild soap and bathing with lukewarm water can help ease the skin. Applying a moisturizer/ointment right after drying the skin (post-bathing) can help seal the moisture in dermal layers.
Final Word
Granuloma annulare is a skin condition that leads to rash/plaque/papule formation with a characteristic ring of raised skin surrounding a central portion. There are different types of disease based on the areas of skin affected. There are no known causes of the skin malady, but researchers believe it is a hypersensitivity reaction to a trigger (infection, trauma, drugs, stress, etc.)
In most patients, the rash resorbs itself but might need treatment in others. It responds well to systemic and topical therapy of steroids and psoriatic medicines. Light therapy, cryotherapy, and laser therapy also have positive outcomes in some cases.
Refrences
- 1Schmieder, S. J., Harper, C. D., & Schmieder, G. J. (2017). Granuloma annulare.
- 2Barbieri, J. S., Rodriguez, O., Rosenbach, M., & Margolis, D. (2021). Incidence and prevalence of granuloma annulare in the United States. JAMA dermatology, 157(7), 824-830.
- 3Thornsberry, L. A., & English, J. C. (2013). Etiology, diagnosis, and therapeutic management of granuloma annulare: an update. American journal of clinical dermatology, 14, 279-290.
- 4Gabaldón, V. H., & Haro-González-Vico, V. (2019). Lack of an association between generalized granuloma annulare and malignancy: A case-control study. Journal of the American Academy of Dermatology, 80(6), 1799-1800.
- 5Khanna, U., & North, J. P. (2020). Patch‐type granuloma annulare: an institution‐based study of 23 cases. Journal of Cutaneous Pathology, 47(9), 785-793.
- 6Pap, N., Bradamante, M., & Ljubojević-Hadžavdić, S. (2019). Localized perforating granuloma annulare. Acta Dermatovenerologica Croatica, 27(1), 33-33.
- 7Endo, Y., Sekiguchi, A., Motegi, S. I., & Ishikawa, O. (2020). Subcutaneous granuloma annulare on the heel: a case report and review of the Japanese published work. The Journal of Dermatology, 47(6), 677-679.
- 8Albert, M., Maruani, A., & Leducq, S. (2023). Clinical Manifestations and Management of Pediatric Granuloma Annulare: A Systematic Review. The Journal of Pediatrics.
- 9Monte‐Serrano, J., García‐Gil, M. F., García‐García, M., Casas‐Flecha, I., Matovelle‐Ochoa, C., & Ara‐Martín, M. (2021). Granuloma annulare triggered by SARS‐CoV‐2 infection: Immunohistochemical staining. Dermatologic Therapy, 34(3).
- 10Fornons-Servent, R., Bauer-Alonso, A., Llobera-Ris, C., Penín, R. M., & Marcoval, J. (2022). Granuloma annulare: a case-control study of possible associated diseases. Dermatology Practical & Conceptual, 12(4).
- 11Joshi, T. P., Chen, V., Dong, J. L., Golden, K., Iacobucci, A., Lim, Y., … & Duvic, M. (2022). Psychiatric comorbidities associated with granuloma annulare: a case-control study in the All of Us database. Journal of the American Academy of Dermatology, 87(3), e119-e120.
- 12Choe, C. S., Hao, L. M., & Mancini, A. J. (2023). Taking the “Worm” out of Ringworm: A Different Annular Rash in Children. The Journal of Pediatrics, 260.
- 13Lukács, J., Schliemann, S., & Elsner, P. (2015). Treatment of generalized granuloma annulare–a systematic review. Journal of the European Academy of Dermatology and Venereology, 29(8), 1467-1480.
- 14Wang, J., & Chen, W. Y. (2021). Imiquimod 5% Cream for an Annular Plaque with Progressive Pain on the Right Distal Arm in the Cubital Fossa: Acquired Tufted Angioma. Clinical, Cosmetic and Investigational Dermatology, 855-858.
- 15Looney, M., & Smith, K. M. (2004). Isotretinoin in the treatment of granuloma annulare. Annals of Pharmacotherapy, 38(3), 494-497.
- 16Grewal, S. K., Rubin, C., & Rosenbach, M. (2017). Antimalarial therapy for granuloma annulare: results of a retrospective analysis. Journal of the American Academy of Dermatology, 76(4), 765-767.
- 17Cunningham, L., Kirby, B., Lally, A., & Collins, P. (2016). The efficacy of PUVA and narrowband UVB phototherapy in the management of generalized granuloma annulare. Journal of Dermatological Treatment, 27(2), 136-139.