Herniated disc surgery is a surgical procedure that is performed to relieve the pressure caused by compression on your spinal nerves. This pressure is mostly due to a slipped or displaced disc, and the procedure is also known as Discectomy or Spinal decompression surgery. The purpose of surgery is to relieve the pressure being applied by the herniated disc on your nerve. Your doctor might recommend surgery when your herniated disc symptoms have not gone away for more than six months or other treatments have failed.1Yoon WW, Koch J. Herniated discs: when is surgery necessary? EFORT Open Rev. 2021 Jun 28;6(6):526-530. Doi: 10.1302/2058-5241.6.210020. PMID: 34267943; PMCID: PMC8246101. It may also be advised when your condition is severely hampering your activity. You may also need surgery if you lose bowel or bladder control.
What is a Herniated Disc?
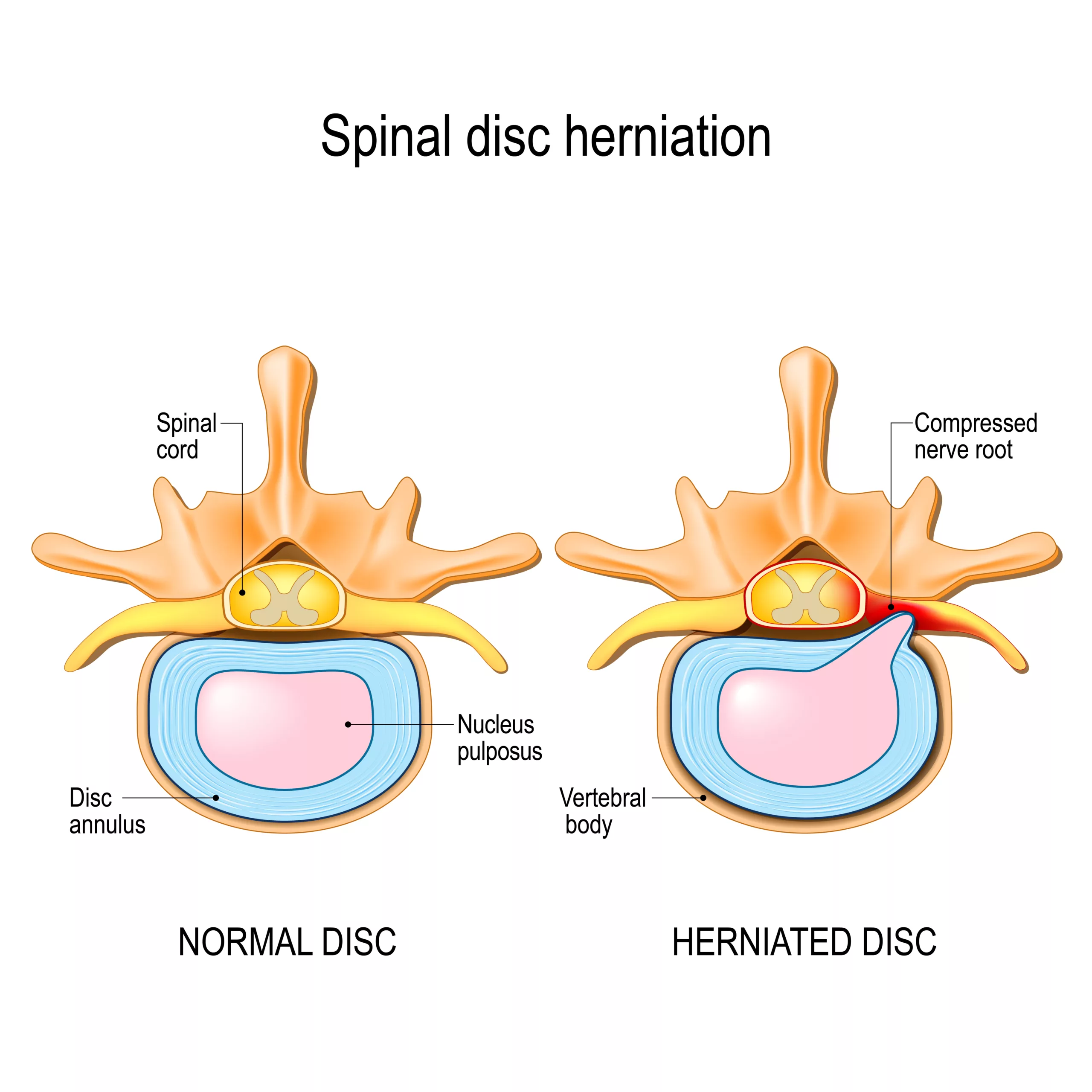
Your spine is a group of bones(vertebrae) separated by discs. These discs act as shock absorbers for your spine when you perform daily activities like walking, lifting, twisting, etc. When a disc herniates, it means that the soft inner core of the disc, called the nucleus pulposus, pushes through the tough outer layer, known as the annulus fibrosus. This can occur due to age-related degeneration, repetitive stress on the spine, improper lifting techniques, or sudden trauma.
This condition can compress nearby nerves, leading to pain, numbness, weakness, and other symptoms. A herniated disc can occur anywhere along the spinal vertebral column, but it usually occurs in the lower back region.
What might cause a Herniated Disc?
You might suffer from a herniated disc due to a single traumatic event to your spine. This may be an injury or excessive strain. However, your disc material degrades naturally as you age, and the ligament that holds your disc in place also weakens. Hence, even simple twisting movements can lead to disc herniations in individuals of older age groups.
What are Herniated Discs Symptoms?
Herniated discs are also known as slipped discs. If a disc in your spine slips out of place, it can put pressure on the nerves in the surrounding area. If a spinal nerve is pressed, then it causes pain2Amin RM, Andrade NS, Neuman BJ. Lumbar Disc Herniation. Curr Rev Musculoskelet Med. 2017;10(4):507-516. doi:10.1007/s12178-017-9441-4 and numbness along the course of that nerve. Hence, a herniated disc involving your lower back may lead to sciatica, while one involving your neck may lead to issues like cervical(neck) pain. You may also feel numbness, tingling, or weakness due to the herniated disc. These symptoms may present as:
- Inability to bend or rotate your neck or back.
- Limping when walking.
- Increased pain when you cough, sneeze, reach for something or sit.
- You may be unable to stand up straight and become “stuck” in a position, like “stooped forward” or “leaning to the side.”
- You may have difficulty getting up from a chair.
- Inability to remain in one position for an extended period, such as sitting or standing, due to pain.
- You may have pain that is worse in the morning.

Usually, your doctor can diagnose a herniated disk with a physical exam, history, and imaging studies. X-rays may be ordered if they suspect other medical conditions or want to see which nerves are affected.
What are the Risk Factors for a Herniated Disc?
Some people are more at risk for herniated discs. If you are overweight, have a sedentary lifestyle, or do a lot of physically demanding work such as heavy lifting, you may be at an increased risk of slipped discs. Older adults are at a higher risk as they lose some of the protective water content in their discs. Moreover, men are at a higher risk than women of having herniated discs.3Zielinska, N., Podgórski, M., Haładaj, R., Polguj, M., & Olewnik, Ł. (2021). Risk Factors of Intervertebral Disc Pathology-A Point of View Formerly and Today-A Review. Journal of clinical medicine, 10(3), 409. https://doi.org/10.3390/jcm10030409
What are some Treatment Options before going for surgery?
Typically, spinal surgery is not recommended as the initial course of action. It is generally advised to exhaust all other options before considering surgical intervention. These alternative options4InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Slipped disc: Non-surgical treatment options. [Updated 2020 Apr 9]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279469/ may encompass the following:
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Medications that help reduce inflammation and alleviate pain.
- Pain relievers: Over-the-counter or prescription medications that provide pain relief.
- Exercise or physical therapy: Specific exercises or therapy programs designed to strengthen the back, improve flexibility, and alleviate symptoms.
- Steroid injections: Injections of corticosteroids into the affected area to reduce inflammation and provide temporary relief.
- Rest: Adequate rest and modified activities to allow the body to heal and minimize strain on the spine.
If these measures prove ineffective and you continue to experience persistent pain that significantly hampers your quality of life, then surgical options can be explored.
Different Types of Surgical Interventions
There are many different surgical options available for treating herniated discs. The choice of surgical procedure depends on factors such as the severity of symptoms, the location of the herniation, and the patient’s overall health. Here are some commonly performed surgical treatments for herniated discs:
Discectomy/ Microdiscectomy
This is the most common procedure for herniated discs in the lumbar (lower back) region. Your surgeon will relieve the pressure on the affected nerve root by removing either a part of your disc or the entire disc (in some cases).5Butler AJ, Munakomi S, Donnally III CJ. Discectomy. [Updated 2023 Aug 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544281/
Your surgeon will make a small incision in your back or neck. This will allow your surgeon to access the affected discs. Some surgical centers may also have the newer and less invasive procedure known as microdiscectomy. These require specialized instruments and have smaller incisions.
Artificial Disc Replacement Surgery:
Artificial disc replacement involves removing and replacing the herniated disc with an artificial disc. This procedure aims to maintain motion at the affected spinal segment while relieving symptoms. This is only recommended for a single disc when the issue is in the lower back. Hence, this will not be recommended if you have multiple discs with degeneration. Moreover, if you have arthritis or osteoporosis, this procedure is not recommended.
Laminotomy/ Laminectomy
A laminotomy or laminectomy is a surgical procedure that involves removing a portion of the lamina, which is the bony arch of a vertebra. This procedure aims to create more space within the spinal canal, alleviating pressure on the spinal cord and nerves. During the surgery, a small incision is made in the vertebral arch to access the affected area and relieve compression on the nerve root. In certain cases, the entire lamina may need to be removed, and this specific procedure is referred to as a laminectomy.
Spinal Fusion
In some cases, the surgeon may perform a spinal fusion along with a discectomy. Individuals might necessitate a fusion procedure if the herniated disc is accompanied by notable spinal instability.
It’s important to note that a spinal fusion procedure has a limited impact on relieving pressure from nerves affected by a herniated disc. Its primary purpose is to provide stability to the spine, albeit with certain trade-offs. The introduction of a spinal fusion can potentially restrict flexibility and mobility, given that the fused or grafted section of the spine loses its capacity to flex and rotate.6Wang JC, Dailey AT, Mummaneni PV, Ghogawala Z, Resnick DK, Watters WC 3rd, Groff MW, Choudhri TF, Eck JC, Sharan A, Dhall SS, Kaiser MG. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 8: lumbar fusion for disc herniation and radiculopathy. J Neurosurg Spine. 2014 Jul;21(1):48-53. doi: 10.3171/2014.4.SPINE14271. PMID: 24980585.
Spinal fusion involves joining two or more vertebrae together using bone grafts or implants to stabilize the spine. This procedure is recommended if removing the disc causes instability in the spine. During the procedure, plastic or metal rods and screws may be inserted to provide additional support. You will undergo general anesthesia and remain hospitalized for several days. However, this procedure will immobilize the affected portion of your spine.
Choosing The Best Treatment Option: An Overview
Physical Examination
Upon discussing your symptoms and medical history, your doctor will conduct a comprehensive physical examination. This examination will include a neurological assessment to identify muscle weakness or sensory loss. During the examination, the doctor will evaluate the muscle strength in your lower legs (if your lower back is involved) by observing your ability to walk on your heels and toes. Additionally, they may assess your reflexes at the knee and ankle and evaluate muscle strength in other regions of your body. The physician will also check for any signs of sensory loss along the pathway of the affected nerve. These tests are crucial in helping the doctor determine the presence of a compressed nerve root in your spine.
Furthermore, your doctor may conduct specialized tests tailored to your specific condition. For cervical (neck) pain, these tests may include the Spurling test, distraction test, upper limb tension test, shoulder abduction test, and Tinel’s sign. In cases of lower back pain, your doctor may perform tests such as the straight leg raise test, contralateral (crossed) straight leg raise test, Lasègue’s test (which is essentially similar to the straight leg raise test), and the bowstring test, among others. These specialized tests provide further insight into your condition, aiding the diagnostic process.
Imaging Studies
Before recommending one type of herniated disc surgery, your surgeon may order a few imaging studies like7 Herniated Disc – Symptoms, Causes, Prevention, and Treatments. (n.d.). Retrieved from www.aans.org website: https://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Herniated-Disc#:~:text=A%20single%20excessive%20strain%20or
- X-rays can produce clear pictures of your vertebrae and joints. The doctor uses them to rule out other causes and bone abnormalities, but they are not typically used to diagnose disc herniations.
- Computed Tomography (CT/CAT scans) provides highly detailed images of your spinal canal and surrounding structures. Your surgeon may recommend it when MRI is not advised, such as in cases of claustrophobia, the presence of metal implants, pacemakers, implanted devices, or certain stages of pregnancy.
- CT Myelogram is also a computed tomography scan. This test is invasive and uses contrast dye injection into the spinal fluid, with X-rays to view the dye. This allows your surgeon to see the location and size of disc herniation.
- Magnetic Resonance Imaging (MRIs) produces 3-D images of your spinal cord, nerve roots, and spinal discs. Medical professionals routinely order this study, considering it the most preferred, to aid in surgical planning.
- Electromyography or Nerve Conduction Studies (EMG/NCS) measure electrical activity along your nerves and muscles.
Surgical Procedure: What to Expect?
Surgical preparation and interventions may vary between hospital settings, resources, and policies. Your surgeon will also consider your age, overall health, and the location of your slipped disc before recommending the appropriate surgical intervention. Some cases may require multiple surgeries. However, you can expect the following:
- Consent: Written consent will have to be provided for the procedure. Your doctor will explain your operation’s risks, procedure, and prognosis. Before the procedure, your surgeon will take certain measures, such as stopping food and water intake to prevent aspiration.
- Anesthesia: Local and general anesthesia have had comparable outcomes in disc herniation surgery. However, Local anesthesia generally has lower costs and risks. The use of local anesthesia for disc herniation surgery depends on factors such as the extent of the surgery, patient preferences, and the surgeon’s recommendation. Sometimes, your doctor may prefer general anesthesia to ensure the patient’s comfort and safety during the surgical procedure. The surgeon will determine the choice of anesthesia in consultation with the patient.
- Antibiotic Prophylaxis: Your surgery will take place in a sterile environment. To prevent infections, your doctor will give you antibiotic prophylaxis before the procedure.
- Incision and Access: Once under anesthesia, the surgeon will make an incision at the appropriate location on your back or neck, depending on the surgical approach. The incision size and placement will depend on the specific procedure.
- Surgical Procedure: The surgeon will perform the necessary steps based on the type of spinal surgery, which may include removing a herniated disc, fusing vertebrae, or decompressing the spinal cord or nerves. They will tailor the surgical technique to your specific condition and requirements.
Follow-up, Recovery, and Post-Surgical Interventions
After spine surgery, you can generally expect positive outcomes with more relief from leg and back pain. Following a recovery period, you should be able to return to your normal activities. The first symptom to improve post-surgery is typically pain, followed by muscle strength and sensation. Rehabilitation programs usually begin around 4-6 weeks after surgery, during which you are provided information about the program you will follow in the coming weeks. You may need assistance with daily activities such as getting out of bed, using the bathroom, and dressing up. Patients may require specialized ergonomic back supports or seats for added comfort.

Your recovery also heavily depends on your specific discharge instructions regarding physiotherapy, exercise, posture correction, medications, and when you should be able to resume normal activity.
Risks Associated with Herniated Disc Surgery
Most people will recover well after surgery. Usually, your surgical outcome will depend on the details of your surgery, your general state of health, and any complications that may arise during your surgery.
All surgeries carry risks such as infections, bleeding, and nerve damage. In some cases, if the disc is not removed, it can rupture again. Additionally, individuals with degenerative disc disease may experience issues with other discs. Patients should anticipate a certain level of stiffness following spinal fusion surgery.
How does a Lumbar Sprain differ from a Herniated Disc?
A lumbar sprain affects the ligaments between the vertebral bones, while disc herniation happens to discs between the vertebrae.
Herniated discs and sprains are not easy to tell apart. However, there are some key differences. Sprains cause pain that is usually limited to the back area. The pain also might reduce in intensity when bending forward and increase in intensity when straightening from a forward bend. Pain from a herniated disc will cause pain down the leg, especially if it’s a lumbar herniation. Moreover, there will be pain with any back movement.
How is a Herniated Disc Differentiated from a Bulging Disc?
Bulging discs happen when the vertebrae put more pressure on one side of the disc, leading it to press outward on the opposite side. However, it is important to note that the outer cartilage often remains intact in such cases. Bulging discs often occur in a series, and the discs may bulge around their entire circumference or along a small portion of it. A bulging disc may often not even cause pain unless it compresses a nerve or leads to inflammation.
A bulging disc may become herniated after worsening over time or bulging too far. This may lead to outer cartilage rupture and a spinal nerve root impingement. Herniated discs are more likely to cause you pain compared to bulging discs.
How to Prevent Slipped (Herniated) Discs?
You should maintain a healthy weight and exercise your back and abdominal muscles, which support your back. Always use the proper lifting technique when lifting heavy weights. Try not to remain seated for long periods. It is helpful to get up and stretch periodically to reduce the risk of slipped discs.
What are the Complications of a Slipped Disc?
Untreated, severe slipped discs can lead to permanent nerve damage. Long-term complications like saddle anesthesia may occur. In this condition, you lose sensation in your inner thighs, the back of your legs, and your rectum.
In some cases, the disc may cut off the impulses to cauda equina nerves, leading to you losing bowel and bladder control.
What are some Natural Treatments for Slipped (Herniated) Discs?
Natural treatments can be beneficial in managing the symptoms of herniated discs. They can include various approaches. Massages, when performed properly, help alleviate pain associated with a herniated disc. Acupuncture is another option that has shown promising results in reducing acute sciatica, neck pain, shoulder pain, and lower back pain caused by herniated discs. In a study, electrical acupuncture for lumbar disc herniation and sciatica demonstrated positive long-term clinical effects.8GU, H. (2019). A 10-year follow-up of electric acupuncture for lumbar disc herniation and sciatica. World Journal of Acupuncture – Moxibustion, 29(3), 221-223. https://doi.org/10.1016/j.wjam.2019.07.002 It’s important to note that while these natural treatments may provide relief for some individuals, their effectiveness can vary from person to person. It’s advisable to consult with a healthcare professional to determine the most suitable treatment options for your specific condition.
Conclusion
In conclusion, if you are experiencing herniated disc symptoms, it is important not to ignore them and seek medical evaluation. While conservative treatments are often the first line of defense, surgery may be necessary for those with persistent pain and functional limitations. You can determine the most appropriate course of action by discussing your symptoms with a healthcare professional and undergoing a thorough evaluation. Remember, early diagnosis and intervention can lead to better outcomes and improved quality of life.
Refrences
- 1Yoon WW, Koch J. Herniated discs: when is surgery necessary? EFORT Open Rev. 2021 Jun 28;6(6):526-530. Doi: 10.1302/2058-5241.6.210020. PMID: 34267943; PMCID: PMC8246101.
- 2Amin RM, Andrade NS, Neuman BJ. Lumbar Disc Herniation. Curr Rev Musculoskelet Med. 2017;10(4):507-516. doi:10.1007/s12178-017-9441-4
- 3Zielinska, N., Podgórski, M., Haładaj, R., Polguj, M., & Olewnik, Ł. (2021). Risk Factors of Intervertebral Disc Pathology-A Point of View Formerly and Today-A Review. Journal of clinical medicine, 10(3), 409. https://doi.org/10.3390/jcm10030409
- 4InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. Slipped disc: Non-surgical treatment options. [Updated 2020 Apr 9]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279469/
- 5Butler AJ, Munakomi S, Donnally III CJ. Discectomy. [Updated 2023 Aug 13]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK544281/
- 6Wang JC, Dailey AT, Mummaneni PV, Ghogawala Z, Resnick DK, Watters WC 3rd, Groff MW, Choudhri TF, Eck JC, Sharan A, Dhall SS, Kaiser MG. Guideline update for the performance of fusion procedures for degenerative disease of the lumbar spine. Part 8: lumbar fusion for disc herniation and radiculopathy. J Neurosurg Spine. 2014 Jul;21(1):48-53. doi: 10.3171/2014.4.SPINE14271. PMID: 24980585.
- 7Herniated Disc – Symptoms, Causes, Prevention, and Treatments. (n.d.). Retrieved from www.aans.org website: https://www.aans.org/Patients/Neurosurgical-Conditions-and-Treatments/Herniated-Disc#:~:text=A%20single%20excessive%20strain%20or
- 8GU, H. (2019). A 10-year follow-up of electric acupuncture for lumbar disc herniation and sciatica. World Journal of Acupuncture – Moxibustion, 29(3), 221-223. https://doi.org/10.1016/j.wjam.2019.07.002