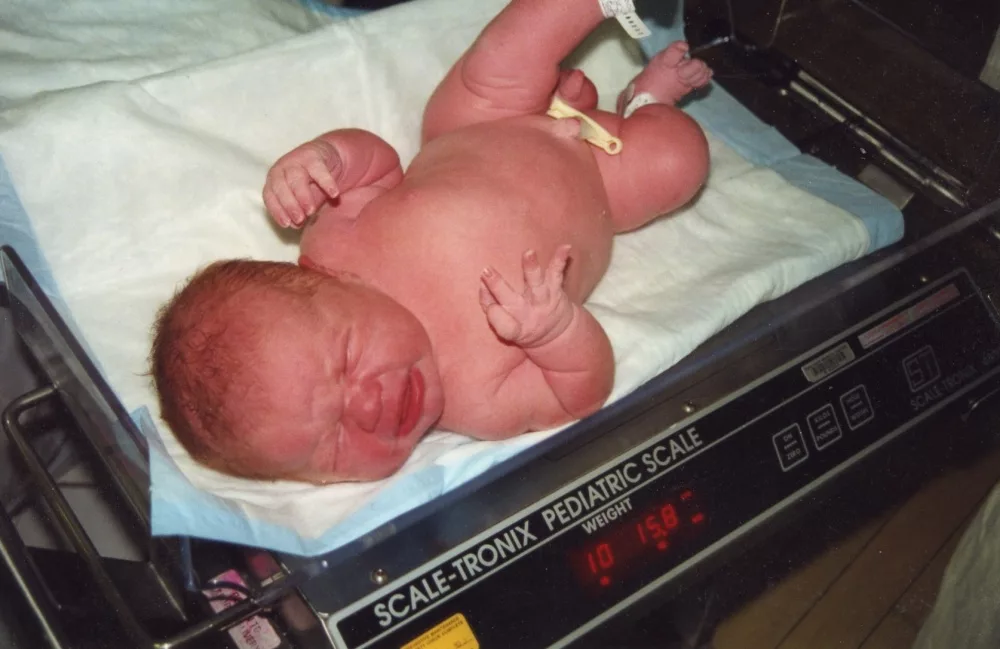
Macrosomia is a condition characterized by fetal overgrowth. In Greek, “macro” means large, and “somia” refers to the body; hence, Macrosomia means “a large body.” In medicine, it refers to a disorder in which a newborn has an unusually high birth weight. About 10% of babies are bigger than normal at birth worldwide. This condition poses a challenge during labour and may lead to fetal and maternal complications.1McFarland MB, Trylovich CG, Langer O. Anthropometric differences in macrosomic infants of diabetic and nondiabetic mothers. J Matern Fetal Med. 1998 Nov-Dec. 7 (6):292-5. Understanding it is crucial for early diagnosis and planning.
What is Macrosomia?
The American College of Obstetricians and Gynaecologists (ACOG) defines macrosomia as “a newborn weighing more than 4000g at birth, irrespective of gestational age.”2[Guideline] Committee on Practice Bulletins—Obstetrics. Macrosomia: ACOG Practice Bulletin, Number 216. Obstet Gynecol. 2020 Jan. 135 (1):e18-35. In some classifications, especially for more severe cases, macrosomia is further stratified:
- >4000 g = Macrosomia
- >4500 g = Severe macrosomia
Globally, the normal birth weight varies between 2500g and 4000g. Macrosomia can result from maternal conditions such as diabetes mellitus (gestational or pregestational), obesity, excessive weight gain during pregnancy, or certain genetic or fetal syndromes.3Stuebe AM, Landon MB, Lai Y, et al. Maternal BMI, glucose tolerance, and adverse pregnancy outcomes. Am J Obstet Gynecol. 2012 Jul. 207 (1):62.e1-7. As fetal weight increases, the likelihood of complications such as injury to birth canal, fetal suffocation (asphyxia), shoulder dystocia, neonatal hypoglycemia, and the need for operative delivery (vaginal or C-section) also rises.
Macrosomia Causes
Research suggests that the main cause of the disorder is a maternal and fetal condition causing elevated blood glucose levels. This glucose crosses the placenta and causes over-secretion of insulin in the fetus, hence disrupting fetal metabolism. In addition, Insulin and insulin-like growth factors serve as anabolic hormones and store fat and glycogen in the fetal body, especially shoulders and upper torso. It results in fetal overgrowth and disproportionate fetal size. In some cases, macrosomia seems to be hereditary; parents who previously delivered large babies are more likely to do so again. In other instances, no specific cause can be identified.
Macrosomia Risk Factors
Certain factors increase the risk of macrosomia, such as:
Maternal Diabetes:
A baby is at risk of developing macrosomia if the mother had diabetes before pregnancy or develops it during pregnancy (Gestational diabetes). The risk increases greatly if diabetes is poorly controlled. Excessive maternal glucose level stimulates overproduction of insulin in the fetus, causing excessive fat storage and a large baby.
Maternal Obesity:
Risk of macrosomia increases 4 to 12 times4Akanmode AM, Mahdy H. Macrosomia. StatPearls. 2023 May 16. if maternal BMI is more than the normal range, i.e., 19.5–24.9. This happens because lipid metabolism in the mother affects the metabolism of the baby as well.
Post-term Pregnancy:
If pregnancy continues beyond 42 weeks, the fetus continues to receive a supply of nutrients and oxygen, hence causing fetal overgrowth.
Previous Macrosomic Pregnancy:
According to research, a history of a previous macrosomic baby increases the risk 5–10 fold of having another one.5Modanlou HD, Dorchester WL, Thorosian A, Freeman RK. Macrosomia–maternal, fetal, and neonatal implications. Obstet Gynecol. 1980 Apr. 55 (4):420-4.
Maternal Age:
Women aged more than 35 years are more at risk of having a big baby.
Multiple Pregnancies:
Although it is not a major risk factor, scientists believe that every new pregnancy increases the risk of diabetes and weight gain in the mother. Women with more than 3 babies are prone to have a macrosomic baby.
Fetal Gender:
Male babies are generally heavier than females, although this may not be a significant standalone factor.
Fetal Syndromes:
Some rare medical conditions also cause fetal macrosomia. These include:
- Beckwith-Wiedemann syndrome
- Sotos syndrome
- Fragile X syndrome
- Weaver syndrome
Macrosomia Symptoms
Some signs and symptoms that give a clue to fetal macrosomia include:
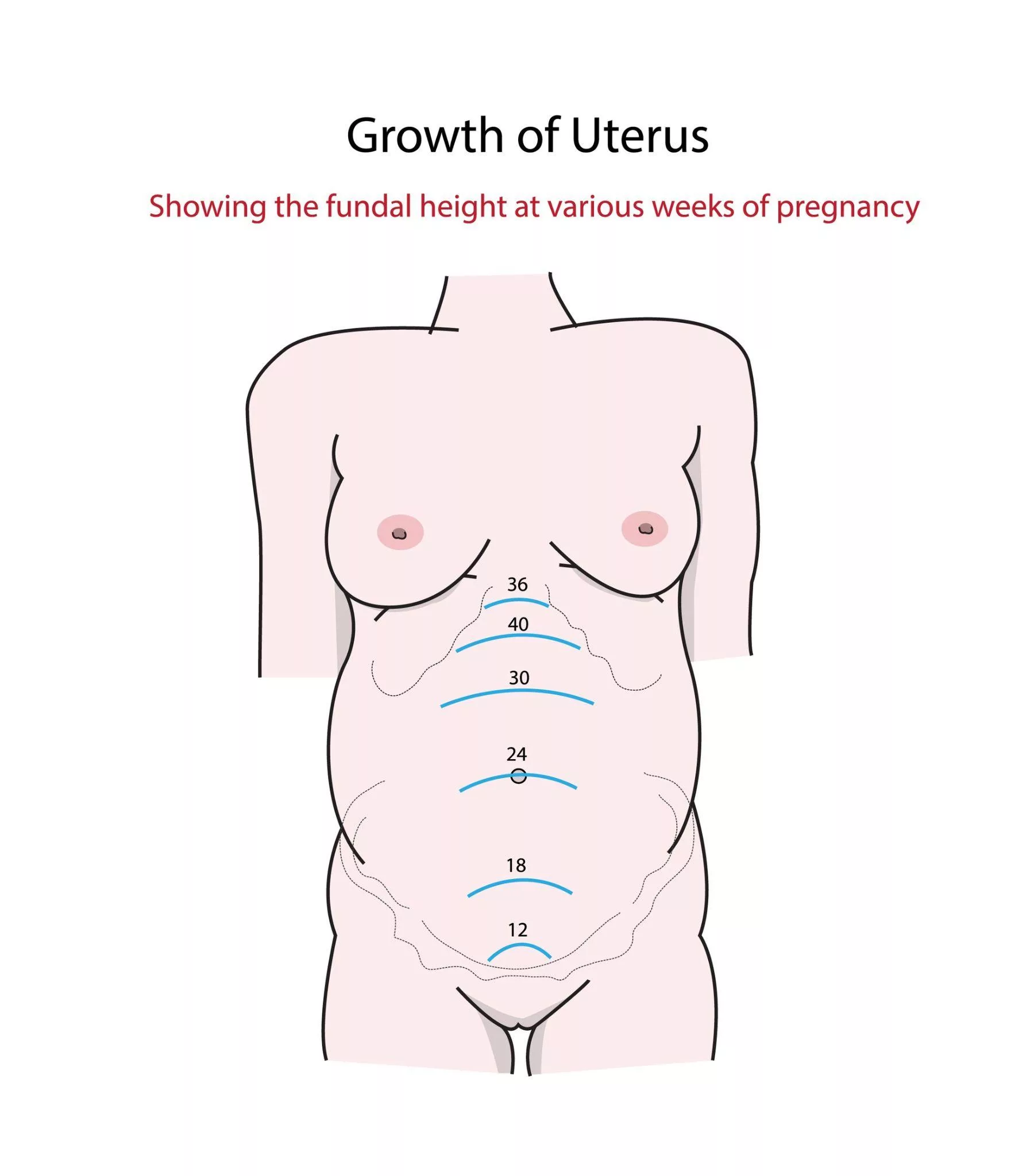
Large Fundal Height:
In every antenatal visit, the healthcare provider measures fundal height. It is measured from the symphysis pubis to the upper margin of the uterus. After 20 weeks of pregnancy, the fundal height in centimetres is almost the same as weeks of gestation. More than normal fundal height raises the suspicion of fetal macrosomia.
Excessive Weight Gain:
For a normal healthy woman whose BMI is in the normal range, 19.5 to 24.9, the weight gain of 11.5kg to 16kg is safe. A weight gain beyond this range may alert to the diagnosis of macrosomia.
Polyhydramnios:
Amniotic fluid is a watery substance that surrounds the developing fetus. It acts as a cushion, provides nutrients, and regulates the temperature of the developing baby. Excess amniotic fluid on an antenatal scan may be a clue to macrosomia, gestational diabetes or fetal oesophageal abnormalities.6Hackmon R, Bornstein E, Ferber A, Horani J, O’Reilly Green CP, Divon MY. Combined analysis with amniotic fluid index and estimated fetal weight for prediction of severe macrosomia at birth. Am J Obstet Gynecol. 2007 Apr. 196(4):333.e1-4.
Macrosomia Complications
Having a big baby may lead to significant complications during pregnancy, at the time of labour, or in the newborn. These include:
Maternal Complications:
In a pregnant woman, macrosomia can cause:
1. Prolonged Labour
On average, labour lasts for 12-18 hours in first-time mothers and 6-8 hours in multiparas. A big fetus may get stuck in the birth canal, prolonging the normal duration of labour.
2. Genital Tract Injury & Postpartum Bleeding
While trying to push out a big baby, mother may have vaginal, cervical,7McFarland LV, Raskin M, Daling JR, Benedetti TJ. Erb/Duchenne’s palsy: a consequence of fetal macrosomia and method of delivery. Obstet Gynecol. 1986 Dec. 68(6):784-8. or perineal tears. These tears are hard to repair and cause blood loss. In addition, a macrosomic baby causes a baggy uterus, which is hard to contract after delivering the baby, consequently leading to excessive bleeding, which can even be fatal.
3. Uterine Rupture
In women with a previous C-section history, a macrosomic baby can cause significant strain on scar tissues and poses the risk of uterine rupture.
Fetal & Childhood Complications:
An unusually big fetus can experience certain complications during delivery. These include:
1. Shoulder Dystocia
In some situations, after the fetal head is delivered, the shoulders fail to follow due to impaction behind the maternal pubic bone—a condition known as shoulder dystocia. This is a medical emergency. If not managed promptly or if excessive force is used, it can result in serious complications such as clavicle or humerus fractures, brachial plexus injuries (e.g., Erb-Duchenne palsy), and birth asphyxia due to prolonged compression of the umbilical cord or chest.8Acker DB, Gregory KD, Sachs BP, Friedman EA. Risk factors for Erb-Duchenne palsy. Obstet Gynecol. 1988 Mar. 71(3 Pt 1):389-92.
2. Fetal Asphyxia
It means fetal suffocation. Delayed or obstructed labour disrupts the blood and oxygen supply to the baby. On CTG, we can notice an unusually increased or decreased heart rate. As a result of compromised blood supply to the vital organs, especially the brain, dreadful outcomes such as fetal distress, cerebral palsy, or, in some cases, fetal demise may occur.
3. Instrumental Delivery
Sometimes, in difficult cases, doctors use forceps or a vacuum to deliver the baby. These instruments are of great help in delivering the obstructed baby. However, the use of forceps can cause scalp and facial bruising and lacerations, whereas vacuum (ventouse suction cup) may lead to hematoma formation under the skull soft tissues. Skilled service providers and appropriate case selection can minimise these risks.
After birth, big newborns can experience:
- Hypoglycemia or episodes of low blood sugar levels
- Polycythemia or increased red blood cells
- Respiratory distress
Additionally, in upcoming years, infants and children are more prone to excessive weight gain and developing metabolic syndrome. Metabolic syndrome is a group of disorders including obesity and elevated cholesterol, glucose, and blood pressure levels. Moreover, they are also at elevated risk of hearing disorders, developmental and intellectual delays.
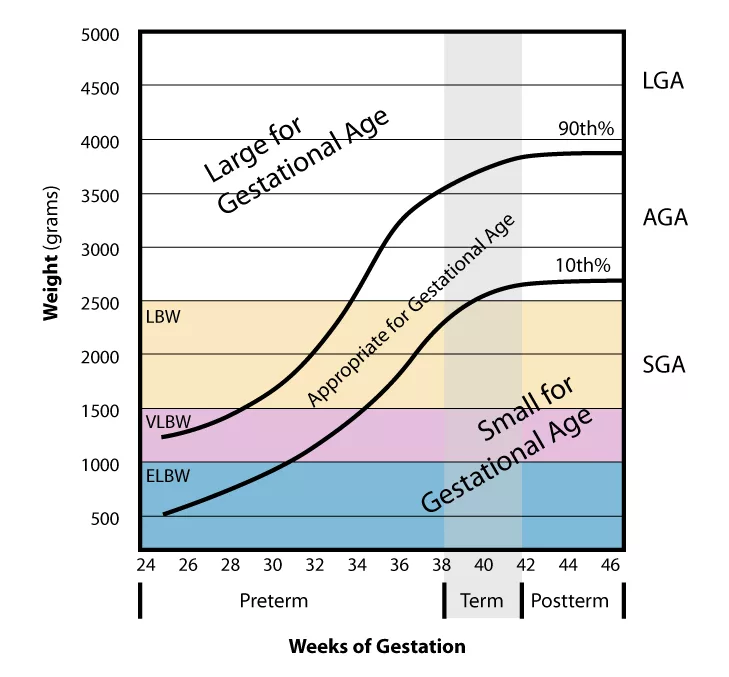
Macrosomia vs Large for Gestational Age(LGA)
These terms are used interchangeably, but are not the same. Key differences include:
| Macrosomia | LGA |
| Definition: Birth weight more than 4000 g | Definition: Weight more than the 90th percentile for a gestational age |
| Gestational age is not considered | Gestational age is essential for diagnosis |
| Postnatal diagnosis on measuring the weight | Prenatal diagnosis by growth charts |
Macrosomia Diagnosis
Since we can measure the weight of the baby only after birth, it is hard to establish a diagnosis of macrosomia during pregnancy. However, some techniques may be helpful, such as:
Fundal Height & Leopold Manoeuvre:
Measuring fundal height is an inaccurate way to diagnose macrosomia. According to research, only 15.8% of patients referred for size greater than dates actually had a fetal weight of more than the 90th percentile for that gestational age.9Sibai, B. M. (2023). Shoulder dystocia: Clinical presentation. Medscape. Retrieved June 24, 2025, from https://emedicine.medscape.com/article/262679-clinical Leopold manoeuvres are techniques of physical examination to determine fetal lie, presentation, and size. However, just like fundal height measurement, it has its limitations. Nevertheless, they can give a general idea and are helpful for initial screening.
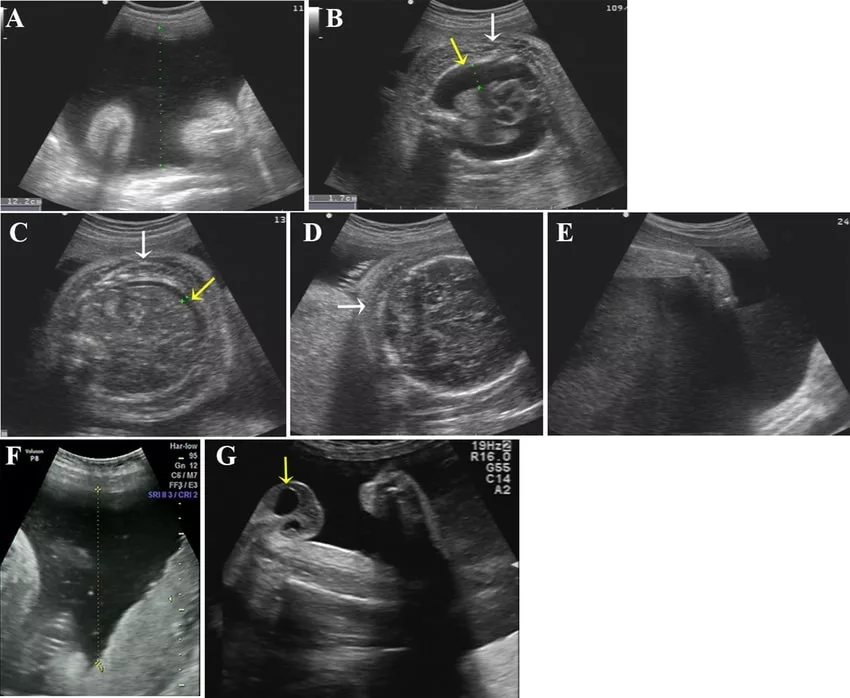
Ultrasonography:
This is a method of using high-frequency sound waves to look at internal organs of the body. In pregnancy, we can see fetal structures with its help. Measurement of abdominal circumference(AC) is a good way to predict fetal weight. In particular, research shows that an abdominal circumference of 35cm or more measured within 2 weeks of delivery is a strong clue to have a baby weighing more than 4000g.10Faschingbauer F, Dammer U, Raabe E, et al. Sonographic weight estimation in fetal macrosomia: influence of the time interval between estimation and delivery. Arch Gynecol Obstet. 2014 Dec 23. Along with AC, an increased amount of liquor is also an indicator of probable macrosomia, especially if these two occur together. However, ultrasound is not a precise method and has a significant room for error.
Glucose Tolerance Test:
On finding excessive amniotic fluid on ultrasound, doctors recommend a glucose tolerance test. The peak time to perform this test is at 24-28 weeks of gestation. In this, a doctor measures the patient’s fasting blood sugar. Then, the patient drinks a solution of 75 grams of glucose. After two hours, they check the blood glucose level again. If the level is higher than normal, the patient is diagnosed as having gestational diabetes mellitus (GDM). Disrupted glucose metabolism is a big indicator of fetal macrosomia.
Biophysical Profile:
A Biophysical Profile (BPP) is a prenatal test to assess the well-being of the fetus. It includes assessment of 5 fetal parameters: body movements, muscle tone, breathing movements, amniotic fluid, and heartbeat. Each one of these is given a score of either 2 (normal) or 0 (abnormal). Though it is not a part of the routine test for diagnosing macrosomia, a lower BPP score (less than 6) indicates high-risk pregnancy, including macrosomia, signalling the need for continuous monitoring or early delivery.
Macrosomia Treatment
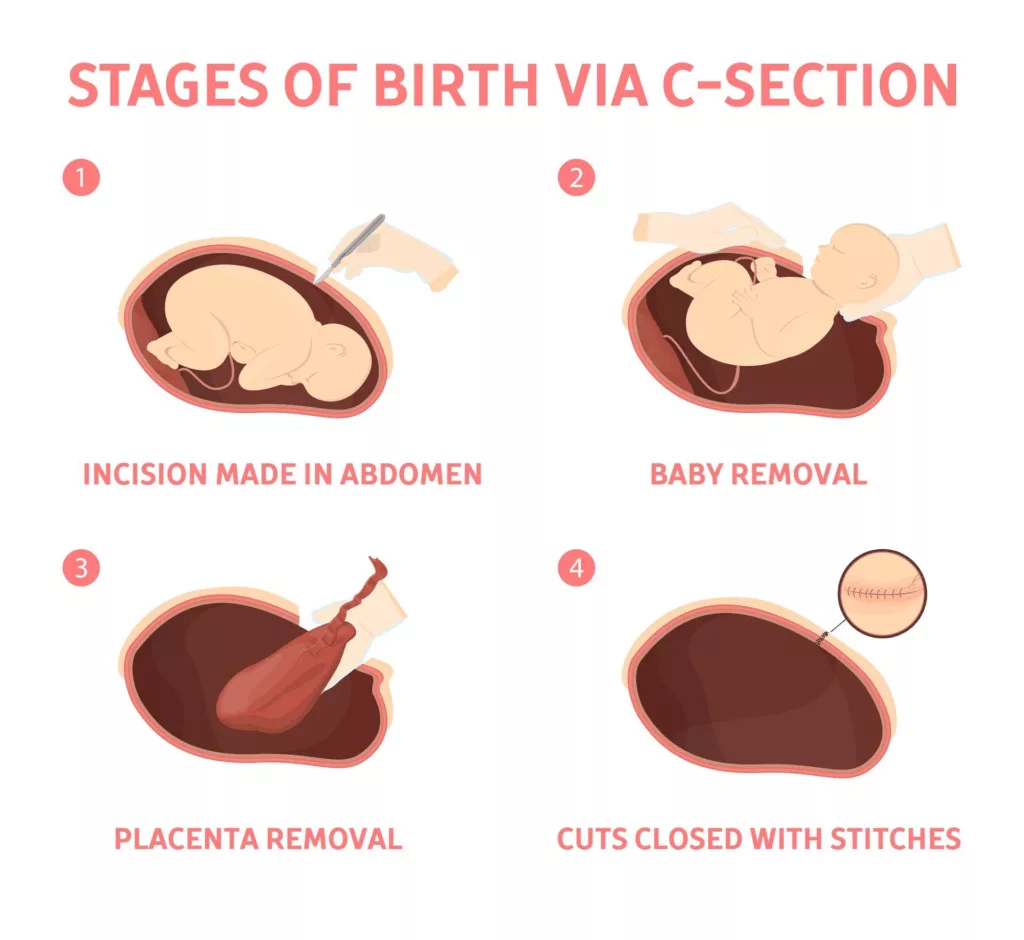
There is no specific treatment for macrosomia, and management focuses on ensuring a safe pregnancy and delivery. Antenatal management involves blood glucose control, exercise, and appropriate weight gain. If a mother manages to do so, a vaginal delivery may still be possible. As the time of delivery approaches, the healthcare provider decides the mode of delivery according to the situation. Induction of labour has unclear benefits and is therefore not preferred. A C-section is typically indicated if:
- Have had a history of shoulder dystocia
- The patient has diabetes, and the baby is estimated to weigh over 10 pounds.
- Doesn’t have diabetes, and the baby is estimated to weigh more than 11 pounds.
Prevention of Macrosomia
Macrosomia is very unpredictable, and we can’t prevent it completely. However, with lifestyle modifications, regular antenatal visits, and adherence to healthcare provider instructions, its occurrence can be decreased. Some tips include:
- Try to maintain weight within the normal range before and during pregnancy.
- Do antenatal visits regularly and get ultrasound scans and lab tests done, as advised.
- Include a daily walk and mild strength training exercises in the routine. They help to regulate blood sugar metabolism and decrease insulin resistance.
- In case of diabetes, ensure to keep the disease well-controlled by taking oral hypoglycemic or insulin. For diabetics, the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) recommends a fasting glucose level of 70-95mg/dL. Try to keep it in the desired range.11National Institute of Diabetes and Digestive and Kidney Diseases. (2022). Diabetes and pregnancy. U.S. Department of Health and Human Services. Retrieved June 24, 2025, from https://www.niddk.nih.gov/health-information/diabetes/diabetes-pregnancy
Differential Diagnosis of Macrosomia:
Other than macrosomia, a large fundal height than normal may be due to:
- Polyhydramnios
- Fibroid uterus
- Pelvic mass
- Inaccurate gestational dates
- Multiple pregnancies
It is essential to rule out these causes by using ultrasound and other methods.
Conclusion
Macrosomia is a disorder of fetal overgrowth that usually happens due to irregular maternal blood glucose levels, which leads to overproduction of insulin and irregular fat deposition in the fetus. Other than that, some fetal syndromes can also cause excessive intrauterine weight gain. Doctors usually suspect macrosomia when a woman is diabetic, obese, has enlarged fundal height on physical examination, or has a high amount of liquor on ultrasound. This condition can’t be prevented, but lifestyle modifications, control of diabetes, and weight management can reduce its risk.
Refrences
- 1McFarland MB, Trylovich CG, Langer O. Anthropometric differences in macrosomic infants of diabetic and nondiabetic mothers. J Matern Fetal Med. 1998 Nov-Dec. 7 (6):292-5.
- 2[Guideline] Committee on Practice Bulletins—Obstetrics. Macrosomia: ACOG Practice Bulletin, Number 216. Obstet Gynecol. 2020 Jan. 135 (1):e18-35.
- 3Stuebe AM, Landon MB, Lai Y, et al. Maternal BMI, glucose tolerance, and adverse pregnancy outcomes. Am J Obstet Gynecol. 2012 Jul. 207 (1):62.e1-7.
- 4Akanmode AM, Mahdy H. Macrosomia. StatPearls. 2023 May 16.
- 5Modanlou HD, Dorchester WL, Thorosian A, Freeman RK. Macrosomia–maternal, fetal, and neonatal implications. Obstet Gynecol. 1980 Apr. 55 (4):420-4.
- 6Hackmon R, Bornstein E, Ferber A, Horani J, O’Reilly Green CP, Divon MY. Combined analysis with amniotic fluid index and estimated fetal weight for prediction of severe macrosomia at birth. Am J Obstet Gynecol. 2007 Apr. 196(4):333.e1-4.
- 7McFarland LV, Raskin M, Daling JR, Benedetti TJ. Erb/Duchenne’s palsy: a consequence of fetal macrosomia and method of delivery. Obstet Gynecol. 1986 Dec. 68(6):784-8.
- 8Acker DB, Gregory KD, Sachs BP, Friedman EA. Risk factors for Erb-Duchenne palsy. Obstet Gynecol. 1988 Mar. 71(3 Pt 1):389-92.
- 9Sibai, B. M. (2023). Shoulder dystocia: Clinical presentation. Medscape. Retrieved June 24, 2025, from https://emedicine.medscape.com/article/262679-clinical
- 10Faschingbauer F, Dammer U, Raabe E, et al. Sonographic weight estimation in fetal macrosomia: influence of the time interval between estimation and delivery. Arch Gynecol Obstet. 2014 Dec 23.
- 11National Institute of Diabetes and Digestive and Kidney Diseases. (2022). Diabetes and pregnancy. U.S. Department of Health and Human Services. Retrieved June 24, 2025, from https://www.niddk.nih.gov/health-information/diabetes/diabetes-pregnancy





