What is Meningioma?
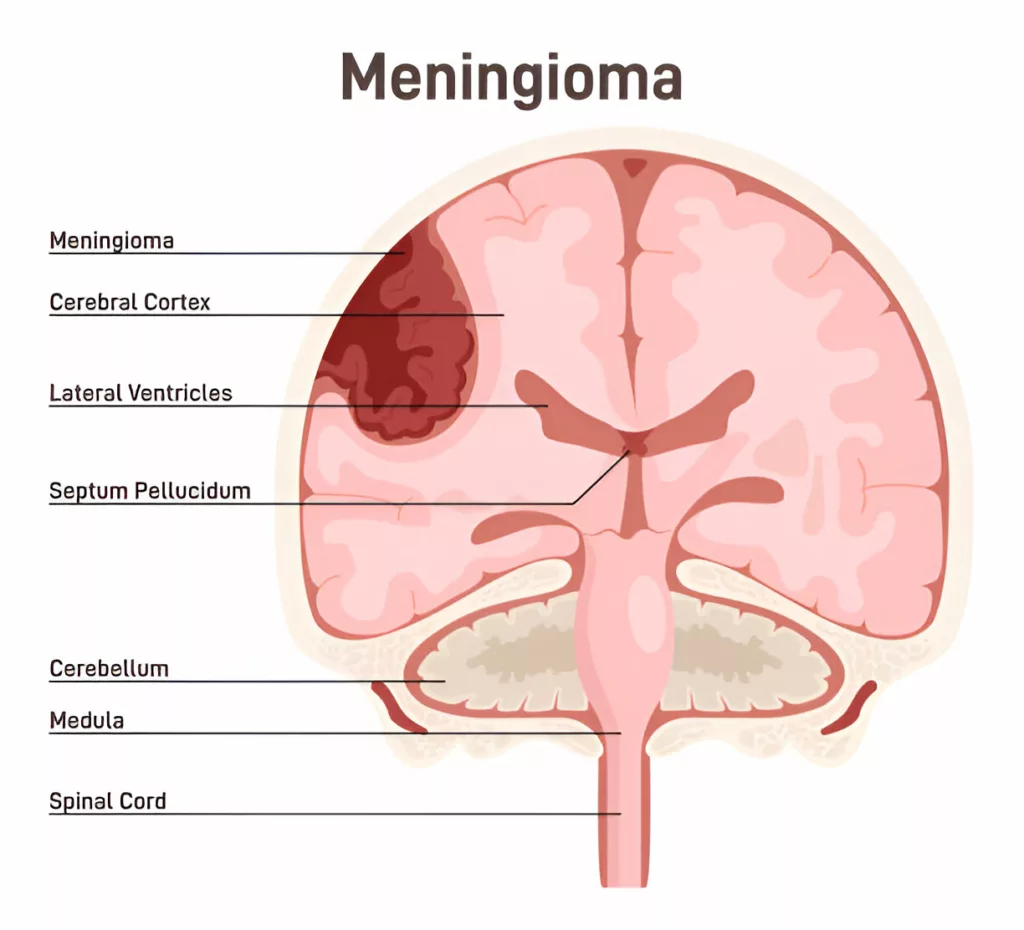
Meningioma is a cancer of the layers of the brain and the spinal cord i.e., meninges. It Is the most common type of brain tumor accounting for 36% of all central nervous system (CNS) tumors.1Walsh, K. M. (2020). Epidemiology of meningiomas. In Handbook of Clinical Neurology (Vol. 169, pp. 3-15). Elsevier. The disease is not very common and the annual incidence of meningiomas was found to be 1.3-7.8 cases/100,000 individuals in a study.2Baldi, I., Engelhardt, J., Bonnet, C., Bauchet, L., Berteaud, E., Grüber, A., & Loiseau, H. (2018). Epidemiology of meningiomas. Neurochirurgie, 64(1), 5-14. The majority of meningiomas are benign and generally do not spread to other parts of the body. Mostly asymptomatic, large tumors can cause neurologic symptoms by pressing on CNS structures. Doctors treat them with radiation therapy and surgery.
Meninges
There are three layers of the protective sheets of the central nervous system. The layers of meninges are as follows:
- Dura matter: It is the outermost layer (directly surrounding the skull and the spinal cord) that protects the brain from excessive movement.
- Arachnoid matter: The middle layer is filled with fluid and cushions the brain.
- Pia matter: It is the innermost layer made of a delicate, thin membrane.
The vast majority of meningiomas arise from the arachnoid cells. Based on the different locations, meningiomas are divided into different types.
Meningioma Types
The most common types of meningiomas include:
Brain Meningiomas:
The highest percentage of meningiomas is of brain meningiomas. There are certain preferred locations where meningiomas grow.3Sun, C., Dou, Z., Wu, J., Jiang, B., Iranmanesh, Y., Yu, X., … & Chen, G. (2020). The preferred locations of meningioma according to different biological characteristics based on voxel-wise analysis. Frontiers in oncology, 10, 1412.
Convexity Meningiomas
This meningioma usually grows on the front (surface) of the brain. Convexity meningiomas account for around 21% of all meningioma cases. Symptoms appear only when the tumor grows big.
Intraventricular Meningioma
The intraventricular system in the brain produces and distributes CSF through the CNS. Meningiomas of the intraventricular system can obstruct the flow which may lead to hydrocephalus.4Bamimore, M. A., Marenco-Hillembrand, L., Ravindran, K., Agyapong, D., Greco, E., Middlebrooks, E. H., & Chaichana, K. L. (2023). Management of Intraventricular Meningiomas. Neurosurgery Clinics, 34(3), 403-415.
Parasagittal aka Falcine Meningioma
Another common meningioma type is the parasagittal meningioma which makes up around 16% of all types. It grows in the region between two sides of the brain i.e., the parasagittal area. As there is a dense network of blood vessels in that region, parasagittal meningiomas can interfere with blood circulation.

Skull Base Meningiomas:
These meningioma types grow under the brain and along the skull base. Surgical treatment of skull base tumors is comparatively difficult.
- Clival meningiomas are located underneath the cerebrum and may grow into a large lesion.
- Foramen magnum meningiomas develop at the hole present between the base of the skull and the spinal cord i.e., foramen magnum.
- Cavernous sinus meningiomas are a rare cancer that affects the brain’s venous sinus and is responsible for eye movement control.
- Sphenoid wing meningiomas develop in the sphenoid ridge (behind the eyes) and can cause visual problems and facial numbness.
- Olfactory groove meningiomas arise near the olfactory nerve (present between the brain and the nose) and can lead to alterations in the sense of smell.
- Posterior fossa aka petrous meningiomas are present on the underside of the brain and make up 10% of meningiomas. They can press on the trigeminal nerve and cause trigeminal neuralgia.
- Suprasellar Meningiomas develop near the optic nerve and the pituitary gland (present at the base of the skull). These slowly progressing tumors can cause severe visual issues.
- Tentorial Meningiomas are rare tumors present in the tentorium cerebellum of the brain and generally cause walking difficulties along with headaches.
Spinal Meningiomas:
Meningiomas of the spinal cord are less common and can press against the spinal structures (especially in the thoracic region). This can lead to chest and back pain, numbness, tingling, etc.
Meningioma Grading
In general, meningiomas are not aggressive and grow slowly. The growth of the meningiomas is towards the inside of the brain (rather than growing towards the outside). Despite being benign, meningiomas can grow large enough to cause life-threatening complications by pressing on brain structures. Based on the growth patterns, doctors divide meningiomas into 3 grades:
Grade Ⅰ: Typical
Benign tumors that grow slowly are termed typical or grade Ⅰ meningiomas. The vast majority of meningeal tumors (80% of cases) are grade Ⅰ tumors.5Apra, C., Peyre, M., & Kalamarides, M. (2018). Current treatment options for meningioma. Expert review of neurotherapeutics, 18(3), 241-249.
Grade Ⅱ: Atypical
Upto 15% of meningiomas are atypical. Noncancerous meningiomas that grow quickly fall under this category. Grade Ⅱ meningiomas are more resistant to conventional therapies.
Grade Ⅲ: Anaplastic
When meningeal tumors become malignant (spread to other parts of the body) they are given grade Ⅲ. These types of cancer account for approximately 1.7% of all cases. They grow and spread very quickly!
Meningioma Symptoms
As mentioned, these slow-growing tumors generally do not cause any symptoms on their own. However, problems arise when the uncontrolled growths become large enough to push and press neighboring brain structures. A meningeal tumor tends to induce swelling of the neighboring brain structures.
You can experience a set of symptoms based on the location and extent of tumor spread within the brain. Patients report the following symptoms of meningiomas:

Headaches & Dizziness
A lot of patients suffering from meningiomas present with headaches. Modern studies highlight a direct link between headaches and intracranial tumors like meningiomas.6Guenther, F., Swozil, F., Heber, S., Buchfelder, M., Messlinger, K., & Fischer, M. J. (2019). Pre-and postoperative headache in patients with meningioma. Cephalalgia, 39(4), 533-543.
Cluster headaches from meningiomas have been extremely rare. However, doctors diagnosed one case of cluster-like headache in a patient with sphenoid ridge meningioma.7Kou, L., Huang, J., Xu, Y., Han, C., Ma, K., Guo, X., … & Wang, T. (2019). Cluster-Like headache secondary to anamnesis of sphenoid ridge meningioma: a case report and literature review. Frontiers in Neurology, 10, 23. Similarly, headaches are also seen in intraventricular meningiomas.8Nakamura, M., Roser, F., Bundschuh, O., Vorkapic, P., & Samii, M. (2003). Intraventricular meningiomas: a review of 16 cases with reference to the literature. Surgical neurology, 59(6), 490-503. In several instances dizziness and disorientation accompany headache. Oftentimes, vertigo/dizziness is present with hearing difficulties.
Nausea & Vomiting
Meningiomas may also present with symptoms of nausea and vomiting. Doctors noted nausea/vomiting as evident symptoms in a 59-year-old patient suffering from brain meningioma.9Sęk, P., & Chilińska, J. Z. (2024). Long-term care for a patient with brain meningioma-a case study. Polish Journal of Applied Sciences, 9(4), 5-13.
Seizures
Meningioma-associated epileptic seizures are a common finding of brain cancer. As per estimates, more than 1/3rd of patients with meningioma suffer from seizures at some point in their disease. Reports suggest that preoperative epilepsy affects approximately 30% of meningioma patients.10Harward, S. C., Rolston, J. D., & Englot, D. J. (2020). Seizures in meningioma. Handbook of Clinical Neurology, 170, 187-200. This gravely impacts the patient’s quality of life.
Muscle Weakness & Paralysis
Weakness of the limbs is mostly related to spinal meningiomas that press against the spinal nerves. Pediatric patients with underlying meningiomas often present with unstable gait and lower limb muscle weakness.11Piątek, P., Kwiatkowski, S., & Milczarek, O. (2022). Spinal meningiomas in pediatric patients–A case series and literature review. Surgical Neurology International, 13.
There have been cases of leg weakness and foot drop caused by giant intracranial meningiomas.12Valerio, J., Santiago, N., Gomez, M. P. F., Martinez, L. R., & Alvarez-Pinzon, A. M. (2024). Giant Meningioma Diagnosis and Clinical Treatment: A Case Report. Cureus, 16(8), e67029. Though rare, clivus meningiomas can induce unilateral paralysis of the hypoglossal nerve (tongue muscle).13Stamenović, J., Živadinović, B., & Đurić, V. (2024). Case report: Unilateral paralysis of the hypoglossal nerve as the only clinical sign of clivus meningioma – a case report and literature review. Frontiers in Oncology, 14, 1337680. According to a study, the three main symptoms of meningiomas are headache, altered mental status, and paralysis.14Krisnayanti, I. A. A., Suarjaya, I. P. P., Juwita, N., & Putra, H. G. S. A. (2024). Neuroanesthesia Management of Complex Meningioma Case: A Comprehensive Approach for Minimizing Edema and Bleeding. Majalah Anestesia & Critical Care, 42(3), 275-283.
Vision & Eye Problems
Spheno-orbital meningiomas are responsible for the development of visual disturbances. In several cases, visual impairment slowly progresses.15Wierzbowska, J., Zegadło, A., Patyk, M., & Rękas, M. (2022). Spheno-orbital meningioma and vision impairment—case report and review of the literature. Journal of Clinical Medicine, 12(1), 74. Patients often complain of blurred vision and monocular vision loss. Other eye symptoms that accompany blurriness include diplopia (double vision), orbital pain, and proptosis (protrusion of the eyeball).16Parish, J. M., Shields, M., Jones, M., Wait, S. D., & Deshmukh, V. R. (2020). Proptosis, orbital pain, and long-standing monocular vision loss resolved by surgical resection of intraosseous spheno-orbital meningioma: a case report and literature review. Journal of Neurological Surgery Reports, 81(01), e28-e32. There may even be a complete loss of vision.
Loss Of Smell
Olfactory groove meningiomas are known to cause alterations in your sense of smell. It may be an initial symptom17Prem, B., & Mueller, C. A. (2021). Smell loss as initial symptom of olfactory groove meningioma. BMJ Case Reports CP, 14(8), e241013. and continue as a chronic symptom for years.18Niklassen, A. S., Jørgensen, R. L., & Fjaeldstad, A. W. (2021). Olfactory groove meningioma with a 10-year history of smell loss and olfactory recovery after surgery. BMJ Case Reports CP, 14(8), e244145.
Hearing Difficulties
Impairments in hearing are rare but large meningeal tumors can lead to them. Sphenoid wing meningiomas can present as sudden sensorineural hearing loss.19Toro, E. D., Risbud, A., Khosravani, N., Vengerovich, G., & Archilla, A. (2021). Sphenoid wing meningioma presenting as sudden sensorineural hearing loss: a case report and literature review. Ear, Nose & Throat Journal, 100(3_suppl), 352S-355S. Even large periventricular meningiomas can lead to nonspecific symptoms like sensorineural hearing loss and tinnitus.
Personality Changes & Memory loss
These symptoms are rare but still can be manifested with a growing meningioma. Neurocognitive disturbances and psychiatric symptoms are understandable provided that meningiomas affect different brain structures. Patients may experience the following neuropsychiatric symptoms:
- Personality changes
- Anxiety
- Memory loss
- Psychosis
- Mood swings
Diagnosis of an underlying meningioma is usually made quite late.20Gyawali, S., Sharma, P., & Mahapatra, A. (2019). Meningioma and psychiatric symptoms: an individual patient data analysis. Asian journal of psychiatry, 42, 94-103.
Overactive Reflexes (Hyperreflexia)
Several meningioma patients show hyperactivation of the reflexes. Psychotic symptoms may accompany hyperreflexia. It is generally seen in individuals with giant meningiomas.21Cabello-Rangel, H., & Díaz-Castro, L. (2016). Frontal lobe syndrome with psychotic symptoms secondary to a giant meningioma in a 38 year old man. Actas Españolas de Psiquiatría, 44(6), 244-252.
Spinal Meningioma Symptoms:
While brain meningiomas manifest with headaches, vision/hearing loss, personality changes, and psychiatric issues, spinal meningiomas mostly cause a different set of symptoms:
Radiculopathy
Meningeal tumors in the spinal region tend to pinch/injure the neighboring nerve roots leading to pain, numbness, burning, and tingling in the area involved. You can suffer from cervical or back pain due to an ingrowing spinal meningioma.
Hyporeflexia
Unlike brain meningiomas, spinal meningiomas may present with underactivation of the reflexes. Multiple neurological issues may be present in patients with spinal meningiomas including poor muscle tone and absent reflex responses.
Meningioma Causes
The exact cause of meningiomas is not known. However, researchers have noted the vast majority (40-80%) of cases arise due to an abnormality (mutation) in chromosome 22. This particular chromosome is responsible for the suppression of tumor growth. The abnormality can either be inherited (from parents) or spontaneous.
Several factors increase your propensity of getting a meningioma:
Risk Factors
- Radiation exposure: Exposure to radiation can cause radiation-induced meningioma (RIM). As per a study, a higher prevalence of tumors with a greater proportion of multiple meningiomas is seen in participants with RIM.22Sadetzki, S., Flint-Richter, P., Ben-Tal, T., & Nass, D. (2002). Radiation-induced meningioma: a descriptive study of 253 cases. Journal of neurosurgery, 97(5), 1078-1082.
- Genetic disorders: Multiple studies show that individuals suffering from neurofibromatosis type 2 (NF2) are extremely likely to develop meningiomas.23Bachir, S., Shah, S., Shapiro, S., Koehler, A., Mahammedi, A., Samy, R. N., … & Sengupta, S. (2021). Neurofibromatosis type 2 (NF2) and the implications for vestibular schwannoma and meningioma pathogenesis. International journal of molecular sciences, 22(2), 690. NF2 is a rare, genetic disorder characterized by the development of tumors in the brain and spinal cord. Other disorders that can increase risk include Li-Fraumeni, Cowden syndrome, etc.
- Gender and age: Females are at a greater risk (three times more) than men. Moreover, individuals aged 70-80 years are at a higher risk of brain cancer as the average age of diagnosis is 66 years.
- Hormonal factors: Females using oral contraceptives and women on hormone replacement therapy are at greater risk too.
Meningioma Diagnosis
Generally, meningiomas are difficult to diagnose because they grow very slowly and do not cause any symptoms. It is only when they grow large enough to impinge neighboring structures that symptoms appear. Oftentimes, the symptoms (like memory loss, loss of balance, etc.) are so mild that they are mistaken for normal aging.
Physical Examination
If a meningioma is suspected, your physician will refer you to a neurologist. The nervous system specialist will start by performing a physical examination followed by neurological testing.
He will ask about the onset, side (of the body), and severity of your symptoms and get details regarding your family health history. In the next step, he may test your reflexes, hearing, vision, etc.
Radiographic Imaging
After physical examination and neurological testing, your healthcare provider may order a battery of imaging tests. Different types of tests provide different details. Some of the most common imaging tests for meningiomas include:
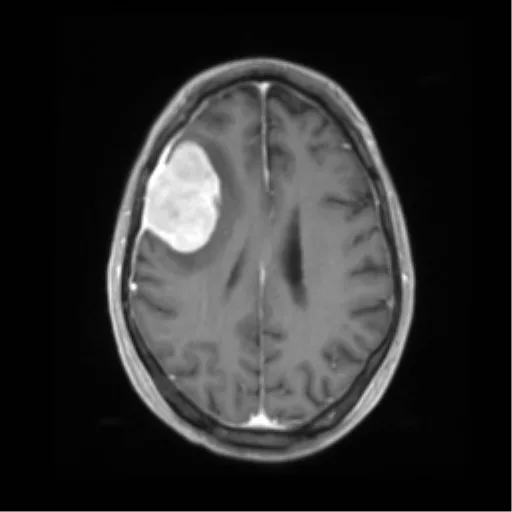
- Magnetic Resonance Imaging scans: A brain MRI scan with contrast helps differentiate and diagnose a meningioma. It provides a clear picture of the internal structures and anomalies. Most neurologists look for a visible thickening of the dura matter on an MRI scan known as the dural tail sign.24Xiao, D., Shi, J., Zhou, M., Yan, L., Zhao, Z., Hu, T., … & Jiang, X. (2021). Tumor volume and the dural tail sign enable the differentiation of intracranial solitary fibrous tumor/hemangiopericytoma from high-grade meningioma. Clinical Neurology and Neurosurgery, 207, 106769.
- Computerized Tomography (CT) scans: A brain CT scan provides a detailed image of the brain structures and layers. It is done by injecting a contrast dye (through IV injection) that highlights and improves brain images.
Pathological Testing
Sometimes, doctors are in doubt about the definitive diagnosis. So, neurosurgeons remove a part of the growing tumor and send it to the lab for microscopic/pathologic testing. Evaluation of the biopsy samples helps determine the grade of the tumor.
Differential Diagnosis:
Meningioma Vs. Glioblastoma
Both are brain tumors but differ in certain aspects. Meningiomas develop in the middle layer of the brain while glioblastomas arise from astrocytes (star-shaped supporter cells for nerves). Meningial tumors are benign, non-aggressive, and grow slowly while glioblastomas grow fast and are cancerous. Meningiomas are comparatively easier to treat.
Meningioma Treatment
Brain cancer treatment generally requires a team of different healthcare professionals. Treatment plans differ between individuals depending on the location, size, spread, type (grade) of the tumor, presence of swelling(edema) in the neighboring structures, and overall health of the patient.
Many times, meningiomas are diagnosed during a routine checkup. If the tumor is small and has no symptoms (or swelling in neighboring structures), doctors usually follow a “wait and see” approach.25Lee, E. J., Park, J. H., Park, E. S., & Kim, J. H. (2017). “Wait-and-see” strategies for newly diagnosed intracranial meningiomas based on the risk of future observation failure. World Neurosurgery, 107, 604-611.
Your doctor may also opt for this approach if:
- You are old and the tumor is non-progressing or progressing very slowly.
- The treatment is risky and offers more risks than benefits.
- You have mild symptoms and no significant impact on your quality of life.
Keeping you under observation does not mean you won’t ever need treatment. You should follow regular checkups with your healthcare provider and get regular scans (MRI/CT) to keep an eye on your tumor size.
Surgery:
The primary choice of treatment for most meningiomas is surgical resection. Neurosurgeons remove tumors that become large or symptomatic. Sometimes, doctors also remove large tumors that tend to cause symptoms later on.
Surgeons opt for different types of surgical procedures based on the following factors:
- Location of the tumor
- Prognosis of the particular approach
- Anatomy of the surrounding structures (important tissues, vessels, etc.)
Gross Total Resection (GTR)
A total removal i.e., gross total resection of the tumor works for most meningioma (70-80%). Neurosurgeons safely remove the whole of the tumor via different approaches. Modern surgeons prefer minimal incisions via your nose (endoscopic endonasal surgery) or the skull (neuro-endoscopic surgery). A complete removal is important to ensure minimal chances of recurrence.
Radiotherapy:
Delivering high doses of ionizing radiation is the treatment of choice for tumors that can’t be successfully removed via surgery (or where surgery risks outweigh benefits). Doctors use different types of radiation therapies to target meningeal tumors:
Gamma Knife Radiosurgery (GKRS)
It is a type of stereotactic radiosurgery which is minimally invasive. In this, doctors deliver high-intensity radiation (very precisely) toward the brain tumor. Unlike conventional radiotherapies, GKRS requires fewer doses. Studies have shown that even single-fraction gamma knife radiosurgery is highly efficacious in removing cavernous sinus meningiomas. In addition to being minimally invasive, it is also very safe and cost-effective.26Tripathi, M., Batish, A., Kumar, N., Ahuja, C. K., Oinam, A. S., Kaur, R., … & Kaur, A. (2020). Safety and efficacy of single-fraction gamma knife radiosurgery for benign confined cavernous sinus tumors: our experience and literature review. Neurosurgical review, 43, 27-40.
Brachytherapy
This highly prevalent method of treating cancers involves placing radioactive seeds (in capsule or implant forms) directly over the tumor (or in close proximity). Sometimes, doctors use brachytherapy to treat anaplastic, recurrent, and malignant meningiomas.27Koch, M. J., Agarwalla, P. K., Royce, T. J., Shih, H. A., Oh, K., Niemierko, A., … & Loeffler, J. S. (2019). Brachytherapy as an adjuvant for recurrent atypical and malignant meningiomas. Neurosurgery, 85(5), E910-E916.
External Beam Radiation Therapy (EBRT)
In this particular modality, beams of high-energy radiation (from an external source) are directed towards the tumor. EBRT is used in various cancer treatments and can work in the case of meningiomas too.
Oftentimes, doctors use what is called “helper therapy” or “adjuvant therapy” along with the main treatment of surgery. Radiation treatment works best as an adjuvant therapy. The adjuvant radiotherapy helps target the cancerous cells that may not be removed via surgery. This additional step helps minimize the risk of recurrence.
Very rarely, doctors use chemotherapy for meningeal tumors. In the case of recurrent meningiomas, the choice of chemical to kill cancers is bevacizumab. Oncologists usually combine chemo, radiotherapy, and surgery to manage malignant, anaplastic tumors.
Potential Side Effects Of Meningioma Treatment:
Unfortunately, meningioma treatment is associated with numerous side effects which include:
- Fatigue
- Appetite loss
- Headaches
- Cognitive disturbances and memory loss
- Post-surgical swelling
- Cerebral edema (build-up of fluid in the brain)
- Cranial nerve injury (which may affect your vision, hearing, swallowing, etc.)
Palliative Care:
Meningioma and its treatment can cause significant complications. Therefore, management of emotional/psychiatric and physical symptoms is a must. This type of care is called palliative care and is important to keep the patients motivated. It also helps improve the quality of life. Modalities include dietary changes, medications, and stress-relieving activities like yoga, massage, etc.
Meningioma Prognosis
The prognosis relies on factors like tumor size, location, grade, and patient factors. Generally, younger patients have a better prognosis. Moreover, the prognosis is better when the tumor is benign and completely removed via surgery (because meningiomas tend to recur).
Meningioma Survival Rates
The 10-year survival rate of meningiomas for grade 1 is 83.7%, for grade 2 is 53% and for grade 3 it is 0%. Benign and malignant spinal meningiomas have better survival rates than cerebral meningiomas.28Ogasawara, C., Philbrick, B. D., & Adamson, D. C. (2021). Meningioma: a review of epidemiology, pathology, diagnosis, treatment, and future directions. Biomedicines, 9(3), 319.
Conclusion
Meningiomas are benign tumors (mostly) that grow on the protective layers of the brain i.e., meninges. They can develop in different regions of the brain and cause issues with vision, smell, memory, and personality. Are mostly asymptomatic, but large tumors may cause symptoms by pressing on brain structures. Issues like headaches, nausea, and muscle paralysis require palliative care. Mutations in the chromosome 22 are suspected to cause the disorder. Old, women and black people are at a greater risk. Constant exposure to radiation and suffering from inherited disorders like NF2 also increases your propensity.
Diagnosis is made using CT and MRI scans. Doctors treat the tumor by gross total removal. In cases where surgery isn’t feasible, doctors opt for radiotherapy. Gamma knife stereotactic gammasurgery is the most effective. Chemotherapy is rarely used. A complete elimination of the tumor is a must because meningiomas tend to recur.
Refrences
- 1Walsh, K. M. (2020). Epidemiology of meningiomas. In Handbook of Clinical Neurology (Vol. 169, pp. 3-15). Elsevier.
- 2Baldi, I., Engelhardt, J., Bonnet, C., Bauchet, L., Berteaud, E., Grüber, A., & Loiseau, H. (2018). Epidemiology of meningiomas. Neurochirurgie, 64(1), 5-14.
- 3Sun, C., Dou, Z., Wu, J., Jiang, B., Iranmanesh, Y., Yu, X., … & Chen, G. (2020). The preferred locations of meningioma according to different biological characteristics based on voxel-wise analysis. Frontiers in oncology, 10, 1412.
- 4Bamimore, M. A., Marenco-Hillembrand, L., Ravindran, K., Agyapong, D., Greco, E., Middlebrooks, E. H., & Chaichana, K. L. (2023). Management of Intraventricular Meningiomas. Neurosurgery Clinics, 34(3), 403-415.
- 5Apra, C., Peyre, M., & Kalamarides, M. (2018). Current treatment options for meningioma. Expert review of neurotherapeutics, 18(3), 241-249.
- 6Guenther, F., Swozil, F., Heber, S., Buchfelder, M., Messlinger, K., & Fischer, M. J. (2019). Pre-and postoperative headache in patients with meningioma. Cephalalgia, 39(4), 533-543.
- 7Kou, L., Huang, J., Xu, Y., Han, C., Ma, K., Guo, X., … & Wang, T. (2019). Cluster-Like headache secondary to anamnesis of sphenoid ridge meningioma: a case report and literature review. Frontiers in Neurology, 10, 23.
- 8Nakamura, M., Roser, F., Bundschuh, O., Vorkapic, P., & Samii, M. (2003). Intraventricular meningiomas: a review of 16 cases with reference to the literature. Surgical neurology, 59(6), 490-503.
- 9Sęk, P., & Chilińska, J. Z. (2024). Long-term care for a patient with brain meningioma-a case study. Polish Journal of Applied Sciences, 9(4), 5-13.
- 10Harward, S. C., Rolston, J. D., & Englot, D. J. (2020). Seizures in meningioma. Handbook of Clinical Neurology, 170, 187-200.
- 11Piątek, P., Kwiatkowski, S., & Milczarek, O. (2022). Spinal meningiomas in pediatric patients–A case series and literature review. Surgical Neurology International, 13.
- 12Valerio, J., Santiago, N., Gomez, M. P. F., Martinez, L. R., & Alvarez-Pinzon, A. M. (2024). Giant Meningioma Diagnosis and Clinical Treatment: A Case Report. Cureus, 16(8), e67029.
- 13Stamenović, J., Živadinović, B., & Đurić, V. (2024). Case report: Unilateral paralysis of the hypoglossal nerve as the only clinical sign of clivus meningioma – a case report and literature review. Frontiers in Oncology, 14, 1337680.
- 14Krisnayanti, I. A. A., Suarjaya, I. P. P., Juwita, N., & Putra, H. G. S. A. (2024). Neuroanesthesia Management of Complex Meningioma Case: A Comprehensive Approach for Minimizing Edema and Bleeding. Majalah Anestesia & Critical Care, 42(3), 275-283.
- 15Wierzbowska, J., Zegadło, A., Patyk, M., & Rękas, M. (2022). Spheno-orbital meningioma and vision impairment—case report and review of the literature. Journal of Clinical Medicine, 12(1), 74.
- 16Parish, J. M., Shields, M., Jones, M., Wait, S. D., & Deshmukh, V. R. (2020). Proptosis, orbital pain, and long-standing monocular vision loss resolved by surgical resection of intraosseous spheno-orbital meningioma: a case report and literature review. Journal of Neurological Surgery Reports, 81(01), e28-e32.
- 17Prem, B., & Mueller, C. A. (2021). Smell loss as initial symptom of olfactory groove meningioma. BMJ Case Reports CP, 14(8), e241013.
- 18Niklassen, A. S., Jørgensen, R. L., & Fjaeldstad, A. W. (2021). Olfactory groove meningioma with a 10-year history of smell loss and olfactory recovery after surgery. BMJ Case Reports CP, 14(8), e244145.
- 19Toro, E. D., Risbud, A., Khosravani, N., Vengerovich, G., & Archilla, A. (2021). Sphenoid wing meningioma presenting as sudden sensorineural hearing loss: a case report and literature review. Ear, Nose & Throat Journal, 100(3_suppl), 352S-355S.
- 20Gyawali, S., Sharma, P., & Mahapatra, A. (2019). Meningioma and psychiatric symptoms: an individual patient data analysis. Asian journal of psychiatry, 42, 94-103.
- 21Cabello-Rangel, H., & Díaz-Castro, L. (2016). Frontal lobe syndrome with psychotic symptoms secondary to a giant meningioma in a 38 year old man. Actas Españolas de Psiquiatría, 44(6), 244-252.
- 22Sadetzki, S., Flint-Richter, P., Ben-Tal, T., & Nass, D. (2002). Radiation-induced meningioma: a descriptive study of 253 cases. Journal of neurosurgery, 97(5), 1078-1082.
- 23Bachir, S., Shah, S., Shapiro, S., Koehler, A., Mahammedi, A., Samy, R. N., … & Sengupta, S. (2021). Neurofibromatosis type 2 (NF2) and the implications for vestibular schwannoma and meningioma pathogenesis. International journal of molecular sciences, 22(2), 690.
- 24Xiao, D., Shi, J., Zhou, M., Yan, L., Zhao, Z., Hu, T., … & Jiang, X. (2021). Tumor volume and the dural tail sign enable the differentiation of intracranial solitary fibrous tumor/hemangiopericytoma from high-grade meningioma. Clinical Neurology and Neurosurgery, 207, 106769.
- 25Lee, E. J., Park, J. H., Park, E. S., & Kim, J. H. (2017). “Wait-and-see” strategies for newly diagnosed intracranial meningiomas based on the risk of future observation failure. World Neurosurgery, 107, 604-611.
- 26Tripathi, M., Batish, A., Kumar, N., Ahuja, C. K., Oinam, A. S., Kaur, R., … & Kaur, A. (2020). Safety and efficacy of single-fraction gamma knife radiosurgery for benign confined cavernous sinus tumors: our experience and literature review. Neurosurgical review, 43, 27-40.
- 27Koch, M. J., Agarwalla, P. K., Royce, T. J., Shih, H. A., Oh, K., Niemierko, A., … & Loeffler, J. S. (2019). Brachytherapy as an adjuvant for recurrent atypical and malignant meningiomas. Neurosurgery, 85(5), E910-E916.
- 28Ogasawara, C., Philbrick, B. D., & Adamson, D. C. (2021). Meningioma: a review of epidemiology, pathology, diagnosis, treatment, and future directions. Biomedicines, 9(3), 319.

