Mucosal melanoma (MM) is an aggressive cancer that affects the protective lining (soft tissue) of internal organs i.e., mucosal membranes. Such types of cancers are rare and account for 2% of all melanomas. Usually, the condition is diagnosed in older individuals (above 65 years) and has an incidence rate of 6.3 per million.1Santeufemia, D. A., Palmieri, G., Miolo, G., Colombino, M., Doro, M. G., Frogheri, L., … & Corona, G. (2023). Current trends in mucosal melanomas: an overview. Cancers, 15(5), 1356. This cancer can arise in the moist linings of different areas such as the mouth and genitals. It spreads quickly to other parts of the body. Thus, timely diagnosis and treatment enhance outcomes. Doctors perform surgery to remove the tumors and may also use adjunctive therapies like radiotherapy, chemotherapy, and immunotherapy.
What is a Mucosal Membrane?
A mucosal membrane is a moist tissue lining present on the inside of several organs and body cavities. These membranes release mucus, lubricate the structures, and offer protection against pathogens. Melanomas can arise in any region of mucus membranes. However, the most common locations for melanomas are:
- Head/neck and oropharyngeal (mouth) region
- Sinonasal (nasal passage and sinuses) region
- Urogenital region (vulva and vagina) region
- Anorectal (anus and rectum) region
Mucosal Melanoma Staging
There is no specific staging system for mucosal melanomas. However, doctors use the American Joint Committee on Cancer (AJCC) Tumor, Node, and Metastasis system to stage cancers of the head/neck and vulva/vaginal regions.
AJCC TNM Staging:
| Stages | Tumor | Node | Metastasis |
| Ⅲ | T3 | N0 | M0 |
| ⅣA | T4a
T3-T4a |
N0
N1 |
M0 |
| ⅣB | T4b | Any level of Node (N) | M0 |
| ⅣC | Any level of Tumor (T) | Any level of N | M1 |
Explaining The Reports:
At T3 stage mucosal melanoma is diagnosed as at an initial stage. However, T4A is assigned to a tumor that has spread to other soft tissues (like cartilage) and skin.
T4B indicates a highly advanced melanoma stage at which there is an invasion of important body parts by cancer cells. Structures that tend to get mets from mucosal melanoma include the base of the skull and the brain including the meninges (especially the dura matter) and the cranial nerves that innervate the voice box and muscles of the neck and tongue). Chewing muscles, carotid artery, and prevertebral space may also be affected. Mets from respiratory tract melanomas can also invade the mediastinal structures including the trachea, esophagus (food pipe), heart, and associated vessels/lymph nodes.
N0 means no nodal involvement while N1 means the cancer has spread to the lymph nodes (from where it can spread to other parts of the body). Similarly, M0 means no metastasis while M1 indicates that cancer has spread to other body parts.
As vaginal/anorectal melanomas do not have a specific staging system, the following system is used:
| Stages | Cancer Spread |
| 1 | Localized tumor |
| 2 | Cancer has spread to lymph nodes in the immediate neighboring area |
| 3 | Carcinoma has metastasized (spread to different regions/organs) |
Mucosal Melanoma Symptoms
Several patients often miss mucosal melanoma symptoms because they are mild. The symptoms of mucosal melanomas differ based on the region involved.
Oral Symptoms:
Primary oral mucosal melanomas account for only 0.2-0.8% of all melanomas. Most patients complain of having lesions/lumps on the palatal mucosa or the tongue.2Nisi, M., Izzetti, R., Gennai, S., Pucci, A., Lenzi, C., & Graziani, F. (2022). Oral mucosal melanoma. Journal of Craniofacial Surgery, 33(3), 830-834. The hard palate is the most common location. Patients also report non-healing mouth sores and occasional unexplained bleeding.
Diagnosis of this cancer is tough because generally there is no pain (despite growing hidden masses in the mouth). According to studies of clinical cases, common symptoms of oral mucosal melanoma include:3Symvoulakis, E. K., Kyrmizakis, D. E., Drivas, E. I., Koutsopoulos, A. V., Malandrakis, S. G., Skoulakis, C. E., & Bizakis, J. G. (2006). Oral mucosal melanoma: a malignant trap. Head & face medicine, 2, 1-4.
- Hoarseness of voice
- Swallowing difficulties (dysphagia)
- Drooling of saliva
Nasal Symptoms:
Unilateral nasal obstruction and epistaxis (nasal bleeds) from one nostril are the most common symptoms when melanoma arises in the region involving the sinuses and the nose.4Behranwala, R., Waduge, B. H. L., & Teo, B. (2019). Nasal mucosal melanoma as a cause of epistaxis. BMJ Case Reports CP, 12(7), e228640. In the vast majority of cases, melanoma arises in the lateral wall or the septum of the nasal cavity.
Severe forms of the cancer may present with nasal swelling and deformities. Sometimes, patients also complain of a runny nose (rhinorrhea). You may experience pain and lacrimation (tear production) if the carcinoma invades the inferior meatus and the lacrimal duct inside the nose.
Laryngopharyngeal Symptoms:
In the throat, you can encounter serious manifestations such as dysphagia (swallowing difficulties) which can be attributed to the mass/lump present on the outside of your neck. Esophageal melanoma can present as a unique cause of dysphagia.5Schizas, D., Mylonas, K. S., Bagias, G., Mastoraki, A., Ioannidi, M., Kanavidis, P., … & Liakakos, T. (2019). Esophageal melanoma: a systematic review and exploratory recurrence and survival analysis. Diseases of the Esophagus, 32(12), doz083.
Hoarseness of voice is seen in more than half of the patients with mucosal melanoma of the larynx/pharynx. Supraglottis (within the larynx) is the most frequently affected site, leading to hoarseness. Large masses can also interfere with normal glottic function and cause airway obstruction leading to dyspnea (trouble breathing).6Valjarević, S., Jovanović, A., Vučić, S., Tomić, A. M., & Jovanović, M. B. (2025). Transglottic laryngeal melanoma presented as a severe dyspnea. Srpski arhiv za celokupno lekarstvo, (00), 11-11.
Gastrointestinal Symptoms:
In most cases, mucosal melanoma of the gastrointestinal tract develops as secondary (mets from another site) melanoma. It can involve the stomach and the bowels. There is a wide range of GIT melanoma symptoms including:7Kohoutova, D., Worku, D., Aziz, H., Teare, J., Weir, J., & Larkin, J. (2021). Malignant melanoma of the gastrointestinal tract: symptoms, diagnosis, and current treatment options. Cells, 10(2), 327.
- Abdominal pain
- Nausea/vomiting
- Indigestion (dyspepsia)
- Unexplained weight loss
- Acute gastrointestinal bleeding
- Chronic iron-deficiency anemia
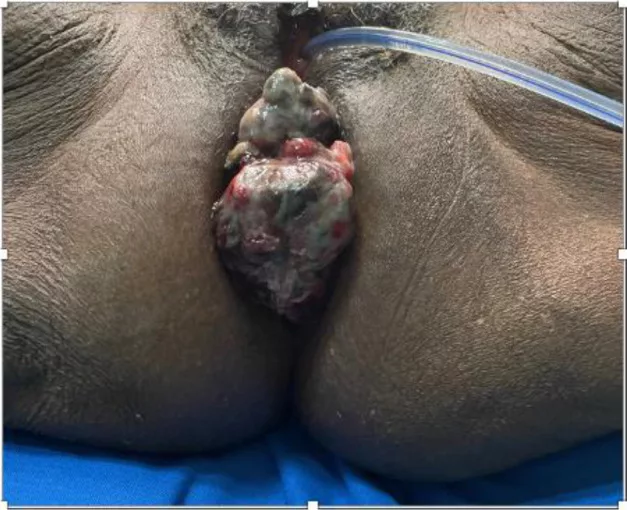
Anorectal Symptoms:
Large melanomas growing in the large intestine and rectal region can contribute to rectal pain (or anal pain) and bleeding. Anorectal melanomas are common types that can cause itchiness (pruritus ani) and constipation. You may also notice blood in vomit or feces due to GIT melanomas.
Urogenital:
Mucosal membranes of the vulva, cervix and vagina can develop melanomas. The urogenital tract melanomas can present with multiple symptoms. Patients most commonly report vaginal bleeding, vaginal nodules (local masses and lumps), and itching with discharge. The itching site may also be painful and the itch does not go away with conventional therapies. Less common symptoms of genital tract melanoma include mucosal thickening and urinary incontinence.8Wu, Y., Li, H., Tan, L., Lai, Y., & Li, Z. (2023). Different clinicopathological and prognostic features of vulvar, vaginal, and cervical melanomas. Human Pathology, 131, 87-97. Pain during urination and blood in urine may also point towards underlying MM.
Mucosal Melanoma Causes
The exact causes of mucosal melanomas are unknown. Abrupt division of the pigment-producing cells i.e., mucosal melanocytes is largely attributed to genetic mutations. The list of genes in which mutations can lead to mucosal melanomas includes:9Broit, N., Johansson, P. A., Rodgers, C. B., Walpole, S. T., Newell, F., Hayward, N. K., & Pritchard, A. L. (2021). Meta-analysis and systematic review of the genomics of mucosal melanoma. Molecular Cancer Research, 19(6), 991-1004.
- KIT
- BRAF
- NRAS
- SF3B1
- SPRED1
Mutations in the KIT genes promote faster multiplication of the cells and contribute to vaginal/valvular melanomas. On the other hand, BRAF gene mutations cause uncontrollable multiplication of cells leading to the formation of tumors/cancers.
Mucosal Melanoma Risk Factors:
Researchers have noted the following risk factors in mucosal melanomas:
Evidence of tobacco use and ill-fitting dentures causing cancers is scarce but as they tend to erode the mucosal surfaces, there is a possibility of cancer development. However, smoking has been linked to a higher prevalence of oral-pigmented lesions.
Infections (HPV and HIV, etc.), chronic inflammation, and exposure to environmental toxins can also increase the risk of mucosal melanomas.
Unlike cutaneous melanomas, UV exposure does not contribute to mucosal melanomas.10Sergi, M. C., Filoni, E., Triggiano, G., Cazzato, G., Internò, V., Porta, C., & Tucci, M. (2023). Mucosal melanoma: epidemiology, clinical features, and treatment. Current Oncology Reports, 25(11), 1247-1258.
Mucosal Melanoma Diagnosis
These melanomas are difficult to diagnose because they are not always visible easily.
Healthcare providers take a complete history of your symptoms and may order different types of imaging tests to visualize the tumorous growths.
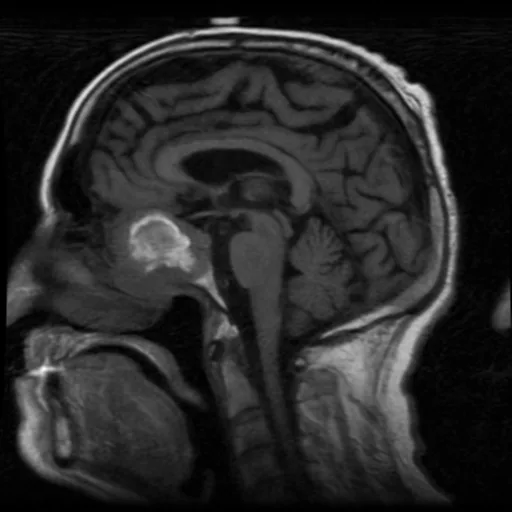
Computed Tomography (CT) scans and Magnetic Resonance Imaging (MRI) scans provide a great deal of tumor detail. Therefore, most healthcare providers advise these scans. Doctors may also use another type of advanced imagery i.e., Positron Emission Tomography (PET) scanning for diagnosing and staging mucosal melanomas.
These diagnostic scans play an integral role in tracking treatment progress and checking for any cancer recurrence too (especially in anorectal and genital MMs).11de Meira Júnior, J. D., Sobrado, L. F., Guzela, V. M., Nahas, S. C., & Sobrado, C. W. (2021). Anorectal mucosal melanoma: a case report and literature review. The American Journal of Case Reports, 22, e933032-1.
Genetic mutation is considered an important aspect of melanomas. So, when suspected, doctors advise genetic testing of the patient to check abruptions in genes.
In some cases, the doctor will remove a small piece of the tumor and send it to the pathology lab. In the laboratory, pathologists examine the biopsy tissues for malignant changes.
Differential Diagnosis:
Mucosal Melanoma Vs Cutanoeus Melanoma
Both tumors arise from the same type of cells i.e., melanocytes. Mucosal melanomas develop on the moist surfaces (mucous membranes) of the body, are rare, and generally more aggressive than MMs. Cutaneous melanomas are common skin lesions. Exposure to UV causes skin melanomas but radiation has no impact on MMs. The treatment prognosis for cutaneous melanomas is better than for mucosal melanomas.
Mucosal Melanoma Treatment
This type of cancer is rare and complicated, mainly because these tumors grow and spread aggressively. Diagnosis is difficult in most cases. Management generally requires a multidisciplinary approach. Treatment options for mucosal melanomas include:
Surgery:
Surgery is the first line of treatment for most types of MMs. Surgeons have to consider certain factors including:
- Tumor location
- Size of tumor
Radical surgery followed by radiation therapy is the mainstay of the treatment (especially for head/neck) for patients with multi-focal tumors or advanced-stage disease.12Pincet, L., Lambercy, K., Pasche, P., Broome, M., Latifyan, S., & Reinhard, A. (2021). Mucosal melanoma of the head and neck: a retrospective review and current opinion. Frontiers in Surgery, 7, 616174. Surgical resection with adjuvant radiotherapy is the primary treatment for sinonasal melanomas as well.13Andrianakis, A., Kiss, P., Pomberger, M., Wolf, A., Thurnher, D., & Tomazic, P. V. (2021). Sinonasal mucosal melanoma: treatment strategies and survival rates for a rare disease entity: A single center experience and review of the literature. Wiener klinische Wochenschrift, 1-11.


Several doctors chose to resect the primary lesions along with negative margins to minimize the chances of recurrence. However, some tumors are challenging to remove due to their anatomical location. Advanced metastasized cancers have poorer prognosis.14Zhang, J., Tian, H., Mao, L., & Si, L. (2024). Treatment of acral and mucosal melanoma: current and emerging targeted therapies. Critical Reviews in Oncology/Hematology, 193, 104221.
Radiation Therapy:
To ensure a complete clearance from cancerous cells, your medical team may also opt for adjuvant radiotherapy. This is mostly administered after surgery to ensure better outcomes.
Immunotherapy:
Poor prognoses of conventional treatments have prompted researchers to find new and effective modalities for treating MM. Immunotherapy is a new type of cancer treatment type that stimulates a patient’s immune system to recognize and attack the defective cells. This therapy relies on medicines that act as immune checkpoint inhibitors (such as PD-1, and CTLA-4 blockers), adoptive cell therapy (ACT), and anti-angiogenic therapy to identify and destroy cancerous cells.
According to small studies, immunotherapy has shown promising results and contributed to increasing survival rates in head/neck MMs.15Wehbe, J., Jaikaransingh, D., & Walker, A. (2022). Immunotherapy as a treatment modality for mucosal melanoma of the head and neck: a systematic review. Medicine, 101(31), e29979. However, the available immunotherapeutic interventions are not clinically reliable. But the good news is that research is ongoing and we may see effective combination therapies in the future.16Mao, L., Qi, Z., Zhang, L., Guo, J., & Si, L. (2021). Immunotherapy in acral and mucosal melanoma: current status and future directions. Frontiers in immunology, 12, 680407.
Targeted Therapy:
Another latest treatment modality to cure mucosal melanomas is targeted therapy. It involves the use of drugs to attack specific/unique molecular anomalies in the cancerous melanocytes. This therapy mostly targets disease-specific gene mutations like KIT or BRAF, etc. Like immunotherapy, it has shown good results in trials and we hope to see more effective options soon.17Cohen Goldemberg, D., Claudio Santos Thuler, L., & Cristina de Melo, A. (2019). An update on mucosal melanoma: future directions. Acta Dermatovenerologica Croatica, 27(1), 11-11.
Mucosal Melanoma Prognosis
Unfortunately, mucosal melanoma has a poor prognosis with an overall 5-year survival rate of less than 20%. However, with new and potent treatment strategies we can expect to see improvements in the treatment outcomes.18Sergi, M. C., Filoni, E., Triggiano, G., Cazzato, G., Internò, V., Porta, C., & Tucci, M. (2023). Mucosal melanoma: epidemiology, clinical features, and treatment. Current Oncology Reports, 25(11), 1247-1258.
Final Word
Melanomas of the moist mucous membranes are rare yet aggressive cancers. Due to the wide distribution of mucosal membranes in the body, melanomas can arise in different parts but are most commonly seen in the head/neck, urogenital, and anorectal regions. Patients experience lumps, swallowing difficulties, and voice hoarseness when the cancer develops in the oral/pharyngeal mucosa. Nasal obstruction and epistaxis are the most common symptoms of nasal melanomas. Individuals with GIT and anorectal melanomas suffer from weight loss, abdominal pain, and rectal pain. Itchiness and blood in stools/vomit may accompany rectal pain. Vaginal discharge and itching are the most frequently seen symptoms of urogenital melanomas.
The cause of MMs is unknown but experts have identified mutations in specific genes (KIT, BRAF, etc.). Diagnosis is made with the help of CT and MRI scans, genetic testing, and sometimes biopsy. Doctors treat it with surgery and adjuvant radiotherapy but there is a poor prognosis. Newer therapies like immunotherapy and targeted therapy are being improved to increase survival rates.
Refrences
- 1Santeufemia, D. A., Palmieri, G., Miolo, G., Colombino, M., Doro, M. G., Frogheri, L., … & Corona, G. (2023). Current trends in mucosal melanomas: an overview. Cancers, 15(5), 1356.
- 2Nisi, M., Izzetti, R., Gennai, S., Pucci, A., Lenzi, C., & Graziani, F. (2022). Oral mucosal melanoma. Journal of Craniofacial Surgery, 33(3), 830-834.
- 3Symvoulakis, E. K., Kyrmizakis, D. E., Drivas, E. I., Koutsopoulos, A. V., Malandrakis, S. G., Skoulakis, C. E., & Bizakis, J. G. (2006). Oral mucosal melanoma: a malignant trap. Head & face medicine, 2, 1-4.
- 4Behranwala, R., Waduge, B. H. L., & Teo, B. (2019). Nasal mucosal melanoma as a cause of epistaxis. BMJ Case Reports CP, 12(7), e228640.
- 5Schizas, D., Mylonas, K. S., Bagias, G., Mastoraki, A., Ioannidi, M., Kanavidis, P., … & Liakakos, T. (2019). Esophageal melanoma: a systematic review and exploratory recurrence and survival analysis. Diseases of the Esophagus, 32(12), doz083.
- 6Valjarević, S., Jovanović, A., Vučić, S., Tomić, A. M., & Jovanović, M. B. (2025). Transglottic laryngeal melanoma presented as a severe dyspnea. Srpski arhiv za celokupno lekarstvo, (00), 11-11.
- 7Kohoutova, D., Worku, D., Aziz, H., Teare, J., Weir, J., & Larkin, J. (2021). Malignant melanoma of the gastrointestinal tract: symptoms, diagnosis, and current treatment options. Cells, 10(2), 327.
- 8Wu, Y., Li, H., Tan, L., Lai, Y., & Li, Z. (2023). Different clinicopathological and prognostic features of vulvar, vaginal, and cervical melanomas. Human Pathology, 131, 87-97.
- 9Broit, N., Johansson, P. A., Rodgers, C. B., Walpole, S. T., Newell, F., Hayward, N. K., & Pritchard, A. L. (2021). Meta-analysis and systematic review of the genomics of mucosal melanoma. Molecular Cancer Research, 19(6), 991-1004.
- 10Sergi, M. C., Filoni, E., Triggiano, G., Cazzato, G., Internò, V., Porta, C., & Tucci, M. (2023). Mucosal melanoma: epidemiology, clinical features, and treatment. Current Oncology Reports, 25(11), 1247-1258.
- 11de Meira Júnior, J. D., Sobrado, L. F., Guzela, V. M., Nahas, S. C., & Sobrado, C. W. (2021). Anorectal mucosal melanoma: a case report and literature review. The American Journal of Case Reports, 22, e933032-1.
- 12Pincet, L., Lambercy, K., Pasche, P., Broome, M., Latifyan, S., & Reinhard, A. (2021). Mucosal melanoma of the head and neck: a retrospective review and current opinion. Frontiers in Surgery, 7, 616174.
- 13Andrianakis, A., Kiss, P., Pomberger, M., Wolf, A., Thurnher, D., & Tomazic, P. V. (2021). Sinonasal mucosal melanoma: treatment strategies and survival rates for a rare disease entity: A single center experience and review of the literature. Wiener klinische Wochenschrift, 1-11.
- 14Zhang, J., Tian, H., Mao, L., & Si, L. (2024). Treatment of acral and mucosal melanoma: current and emerging targeted therapies. Critical Reviews in Oncology/Hematology, 193, 104221.
- 15Wehbe, J., Jaikaransingh, D., & Walker, A. (2022). Immunotherapy as a treatment modality for mucosal melanoma of the head and neck: a systematic review. Medicine, 101(31), e29979.
- 16Mao, L., Qi, Z., Zhang, L., Guo, J., & Si, L. (2021). Immunotherapy in acral and mucosal melanoma: current status and future directions. Frontiers in immunology, 12, 680407.
- 17Cohen Goldemberg, D., Claudio Santos Thuler, L., & Cristina de Melo, A. (2019). An update on mucosal melanoma: future directions. Acta Dermatovenerologica Croatica, 27(1), 11-11.
- 18Sergi, M. C., Filoni, E., Triggiano, G., Cazzato, G., Internò, V., Porta, C., & Tucci, M. (2023). Mucosal melanoma: epidemiology, clinical features, and treatment. Current Oncology Reports, 25(11), 1247-1258.

