What is Secondary Dysmenorrhea?
Secondary dysmenorrhea refers to menstrual pain that occurs due to an underlying pelvic pathology, such as endometriosis or adenomyosis. It is characterized by recurrent, crampy, lower abdominal pain during menses. The pain starts a few hours before menses and can persist for almost three days. The cramps could be episodic and radiate to your back, pelvis, and thighs. Secondary dysmenorrhea can negatively impact your emotional and physical well-being.1UpToDate. Dysmenorrhea in adult females: Treatment. Retrieved from https://www.uptodate.com/contents/dysmenorrhea-in-adult-females-treatment?search=secondary%20dysmenorrhea&source=search_result&selectedTitle=2%7E150&usage_type=default&display_rank=2
Difference between Primary & Secondary Dysmenorrhea
Primary dysmenorrhea starts after 1 or 2 years of your menarche (the age at which your menstrual cycle begins). You do not get primary dysmenorrhea due to any disease or pathology. The reason for primary dysmenorrhea is a chemical imbalance in your body. A higher level of prostaglandins in the menstrual blood causes pain. These prostaglandins cause constriction of your uterus by increasing uterine pressure, leading to crampy pain in your lower abdomen that may radiate to your lower back. Moreover, this constriction causes a decreased level of oxygen in your tissues, further causing pain and nausea.
On the other hand, secondary dysmenorrhea occurs when you have any ongoing disease or structural abnormality inside or outside of your uterus. In most cases, you diagnose secondary dysmenorrhea in your middle age, and you may experience some other symptoms along with pain like heavy bleeding and pain during or after intercourse (sex).2Bernardi, M., Lazzeri, L., Perelli, F., Reis, F. M., & Petraglia, F. (2017). Dysmenorrhea and related disorders. F1000Research, 6, 1645. https://doi.org/10.12688/f1000research.11682.1
Why does Secondary Dysmenorrhea Occur?
Secondary dysmenorrhea is the pain you feel during periods due to any pathology or disease in your reproductive organs. The following pathologies may cause painful menstruation:
Endometriosis:
In endometriosis, tissue similar to the uterus grows outside the uterus, primarily in the ovaries, fallopian tubes, and pelvic organs. This condition affects fertility and also causes severe pain during menstrual cycles.
Interstitial Cystitis:
Interstitial cystitis is inflammation of the bladder’s lining. It causes pain when the bladder is full or when you try to pee. This condition can also increase the severity of your menstrual pain.
Fibroids:
Fibroids are abnormal growths of fibrous tissue in your uterus, causing pain in your lower abdomen and heavy menstrual bleeding. They put pressure on your pelvic organs due to their size, which is the cause of the severe pain you feel during your menstrual cycle.

Endometrial Polyps:
Endometrial polyps are abnormal projections of growth in your uterine cavity that are sometimes cancerous. These polyps can fill your entire uterine cavity and cause secondary dysmenorrhea. They also affect your fertility.
Pelvic Inflammatory Disease:
PID is the infection of your uterus, ovaries, or fallopian tubes that spreads through unprotected intercourse. In PID, you feel pain in your lower abdomen along with vaginal discharge. The pain increases in severity during your menstrual cycle.
Use of Intrauterine Contraceptive Devices:
You are more at risk of having secondary dysmenorrhea if you use intrauterine devices for contraception, especially Copper-T devices. You feel more pain during the first one or two years after Copper-T insertion.
Adenomyosis:
In adenomyosis, the uterine wall tissue grows inside your uterus as finger-like projections, causing your uterus to enlarge. It causes heavy menstrual bleeding, and due to increased levels of prostaglandins in your body, adenomyosis also causes secondary dysmenorrhea.
Cervical Stenosis:
In cervical stenosis, the opening of your cervix gets narrowed due to various factors like surgery, cancer, or it can be congenital. Due to narrowing, you feel severe pain during your menses.
Large Cesarean Scar Niche:
You may get a C-section scar niche (unhealed part) due to improper suturing methods, poor surgical technique, or your own decreased immunity. The presence of a niche in your scar becomes a cause of heavy menstrual bleeding and secondary dysmenorrhea.3Harada T. (2013). Dysmenorrhea and endometriosis in young women. Yonago acta medica, 56(4), 81–84.
Symptoms of Secondary Dysmenorrhea
In addition to pain, you may feel the following associated symptoms during your menstrual cycle:4Abreu-Sánchez, A., Parra-Fernández, M. L., Onieva-Zafra, M. D., Ramos-Pichardo, J. D., & Fernández-Martínez, E. (2020). Type of Dysmenorrhea, Menstrual Characteristics and Symptoms in Nursing Students in Southern Spain. Healthcare (Basel, Switzerland), 8(3), 302. https://doi.org/10.3390/healthcare8030302
- Menorrhagia (heavy bleeding in your menstrual cycle)
- Dyspareunia (pain during or after having sex)
- Intermenstrual bleeding (bleeding between your periods)
- Post-coital bleeding (bleeding after you had sex)
- Diarrhea and nausea
- Irritability
- Headache
- Fatigue
- Fainting
- Vomiting
How to Diagnose Secondary Dysmenorrhea?
Your doctor diagnoses secondary dysmenorrhea by taking a proper and detailed history and performing your abdominal as well as pelvic examinations.
Detailed History of Your Symptoms:
For an accurate diagnosis of secondary dysmenorrhea, providing a detailed history of menstrual cycle symptoms is crucial. Your doctor may inquire about the onset, duration, nature, and severity of pain, as well as associated symptoms such as details of vaginal discharge, bleeding between your menstrual cycles, pain during intercourse, cesarean section history, and family history of dysmenorrhea. Comprehensive information is essential for practical medical evaluation and identification of potential causes.
Abdominal & Pelvic Examination:
Your doctor performs superficial and deep palpation of your abdomen and pelvis to check the size of the uterus and to observe whether you have any mass like fibroids, which can be the cause of secondary dysmenorrhea. During a pelvic examination, your physician put a speculum in your vagina after applying a numbing cream. This speculum helps your doctor to see the internal structures like the cervix and walls of the uterus.
Ultrasound:
Ultrasound is the initial evaluation to diagnose secondary dysmenorrhea because it helps to analyze its causes, such as endometriosis, adenomyosis, congenital disorders, or fibroids.
Endocervical or Vaginal Swabs:
If there is a suspicion of ongoing infection, your doctor uses an endocervical or vaginal swab to take a sample from the cervical opening or your inner vaginal wall. The swab test shows the presence of bacteria and an abnormal pH of your cervix if the pelvic inflammatory disease is the cause of secondary dysmenorrhea.
Hysteroscopy:
In hysteroscopy, your doctor uses a hysteroscope to see the inside of your uterine cavity. Hysteroscopy helps to diagnose any anomaly in your uterus that is causing secondary dysmenorrhea like fibroids or endometriosis.

Laparoscopy:
If secondary dysmenorrhea is not diagnosed by ultrasound or hysteroscopy, laparoscopy is the next best option. In laparoscopy, your surgeon makes small incisions in your abdomen and inserts a video camera through these incisions. This helps to see your pelvic organs and diagnose the cause of secondary dysmenorrhea, such as fibroids or polyps.
MRI:
Suppose you have secondary dysmenorrhea due to adenomyosis or due to any congenital disability like the Mullerian anomaly. The ultrasound cannot diagnose it properly, so your doctor may need an MRI. However, your doctor might not suggest it as an initial investigation because it is expensive.5Proctor, M., & Farquhar, C. (2006). Diagnosis and management of dysmenorrhoea. BMJ (Clinical research ed.), 332(7550), 1134–1138. https://doi.org/10.1136/bmj.332.7550.1134
Management & Treatment of Secondary Dysmenorrhea
Treatment for primary and secondary dysmenorrhea often begins similarly. Management and treatment of secondary dysmenorrhea focus mainly on pain relief so that you can do your daily life activities with ease. Essential interventions that your doctor can implement to manage secondary dysmenorrhea are general education about the disease, reassurance, and then medical and surgical treatment. The treatment inlcudes both PAhrmavological and non-pharmavological interventions.6Nagy H, Carlson K, Khan MAB. Dysmenorrhea. [Updated 2023 Nov 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560834/
Non-Pharmacological Treatment:
These are some common and effective management options that you can consider to relieve your pain other than taking painkillers:
Heating pad
A heating pad helps relieve your pain by dilating the blood vessels and increasing blood flow. Types of heating pads that you can use are electrical or hot water bottles. Place it on your lower abdomen for 15 to 20 minutes to relieve the menstrual pain.

Healthy Diet
You should have a healthy diet to reduce menstrual pain. Take a diet containing iron, magnesium, and Vitamin E, like fish, vegetables, whole grains, and nuts. Also, consider taking calcium and vitamin D supplements as they boost your immunity. Avoid salt intake as much as possible to reduce abdominal pain and bloating.
Exercise
Exercise can effectively reduce menstrual pain by releasing endorphins (hormones that reduce stress and improve mood). Moreover, exercise increases your blood flow, reducing pain severity.
Massage
You should get an abdominal massage if you experience severe pain during menses. Massages help to relax your uterus and increase blood flow, ultimately decreasing the intensity of your pain.
Rest
You should lie down on your back for a few hours as it reduces the pressure on your abdomen and thus reduces the menstrual pain.
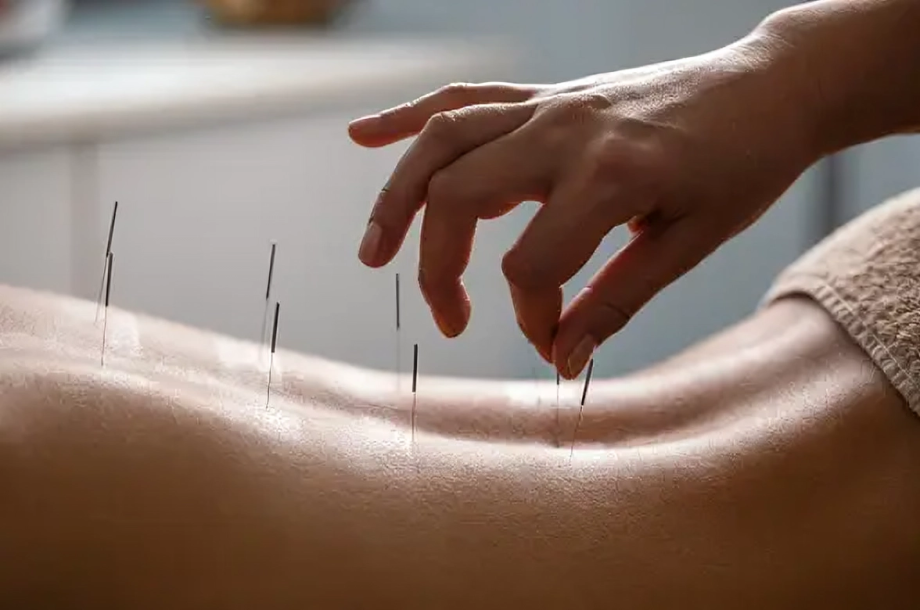
Acupuncture
In acupuncture, your physician injects thin needles into specific points of your body that activate the central nervous system. Then, your CNS releases certain hormones like serotonin that help to reduce the intensity of your menstrual pain. Acupuncture may cause you some discomfort and pain during the insertion of needles.
Transcutaneous Electrical Nerve Stimulation
In TENS, your doctor attaches an electrical machine with electrodes to your skin with the help of small pads. This machine sends signals to your brain and spinal cord, which help reduce the severity of your menstrual pain. However, you only get temporary relief from pain through this technique.7Armour, M., Smith, C. A., Steel, K. A., & Macmillan, F. (2019). The effectiveness of self-care and lifestyle interventions in primary dysmenorrhea: a systematic review and meta-analysis. BMC complementary and alternative medicine, 19(1), 22. https://doi.org/10.1186/s12906-019-2433-8
Pharmacological Treatment:
Medicines that you can take to reduce menstrual pain are:
Nonsteroidal Anti-inflammatory drugs (NSAIDs)
The first treatment that you can take for menstrual pain is NSAIDs, as they decrease the production of prostaglandins in your body, thereby reducing the pain. They are very effective in reducing the menstrual pain in less time. NSAIDs that you can take are ibuprofen, aspirin, and mefenamic acid.
Acetaminophen
If you cannot take NSAIDs for menstrual pain, the next best option is acetaminophen. The most common acetaminophen that you can take is panadol, which is readily available.
Hormonal Medications
Your doctor may prescribe combined hormonal contraception methods (both estrogen and progesterone), contraceptive pills, patches, or vaginal rings to treat the pain associated with menses. Estrogen and progesterone together make your endometrial thin, leading to decreased menstrual bleeding. Less bleeding eventually helps to reduce your pain. You can also take progestin-only contraception in the form of implants, intrauterine devices, or injections, especially if you have dysmenorrhea due to endometriosis.
Gonadotropin-Releasing Hormone Pills
GnRH agonists and antagonists are also helpful in reducing the intensity of menstrual pain, especially if you have endometriosis. Agonists and antagonists that you can use are Nafarelin and Elagolix, respectively.
Aromatase Inhibitors
Aromatase inhibitors cause your menstrual cycle to stop, thereby reducing the pain you feel during menses. However, they also cause weakness in your bones. Your doctor might not recommend these medications as a first-line therapy, especially without prescribing combined contraceptive medicines.
Surgical Treatment:
Your doctor may suggest surgical treatment for addressing the underlysing pathology for Secondary dysmennhorea. The surgical options available are:
Laparoscopy
Your doctor may advise you to have a laparoscopy if you have secondary dysmenorrhea due to endometriosis and it is not relieved by any medication. In laparoscopy, your surgeon resects the endometrial tissue and also gives you hormonal medications to use post-operatively.
Endometrial Ablation
Your surgeon only cuts the inner lining of your uterus in endometrial ablation. If you are suffering from heavy menstrual bleeding along with dysmenorrhea, endometrial ablation is an excellent surgical option.
Hysterectomy
If the results are not satisfactory by all other methods of treatment, you can go for a hysterectomy (removal of your uterus) to treat secondary dysmenorrhea. It is a recommended option only if you have completed your family.8Proctor, M. L., & Murphy, P. A. (2001). Herbal and dietary therapies for primary and secondary dysmenorrhoea. The Cochrane database of systematic reviews, (3), CD002124. https://doi.org/10.1002/14651858.CD002124
Complications of Secondary Dysmenorrhea
Complications of secondary dysmenorrhea depend upon the disease associated with it. Some of the complications that you can experience are:
- Infertility
- Pelvic organ prolapse
- Heavy menstrual bleeding
- Anemia
How do Metrorrhagia & Secondary Dysmenorrhea Differ?
Secondary dysmenorrhea is the pain you endure in your periods due to any disease in the reproductive system. However, metrorrhagia is a disturbance in the average duration of your periods, and you get periods for more than seven days. It is an irregular bleeding that you experience if you have fibroids, adenomyosis, or polycystic ovarian syndrome (cysts in your ovaries).
Conclusion
In conclusion, if you have any disease or pathology in the reproductive system, you might get secondary dysmenorrhea, and its leading cause is endometriosis. You may get heavy menstrual bleeding, irregular bleeding, nausea, or vomiting along with the pain. Take NSAIDS to reduce the pain intensity, and choose a healthy diet. You can also go for surgery if medical treatment doesn’t give good results.
Refrences
- 1UpToDate. Dysmenorrhea in adult females: Treatment. Retrieved from https://www.uptodate.com/contents/dysmenorrhea-in-adult-females-treatment?search=secondary%20dysmenorrhea&source=search_result&selectedTitle=2%7E150&usage_type=default&display_rank=2
- 2Bernardi, M., Lazzeri, L., Perelli, F., Reis, F. M., & Petraglia, F. (2017). Dysmenorrhea and related disorders. F1000Research, 6, 1645. https://doi.org/10.12688/f1000research.11682.1
- 3Harada T. (2013). Dysmenorrhea and endometriosis in young women. Yonago acta medica, 56(4), 81–84.
- 4Abreu-Sánchez, A., Parra-Fernández, M. L., Onieva-Zafra, M. D., Ramos-Pichardo, J. D., & Fernández-Martínez, E. (2020). Type of Dysmenorrhea, Menstrual Characteristics and Symptoms in Nursing Students in Southern Spain. Healthcare (Basel, Switzerland), 8(3), 302. https://doi.org/10.3390/healthcare8030302
- 5Proctor, M., & Farquhar, C. (2006). Diagnosis and management of dysmenorrhoea. BMJ (Clinical research ed.), 332(7550), 1134–1138. https://doi.org/10.1136/bmj.332.7550.1134
- 6Nagy H, Carlson K, Khan MAB. Dysmenorrhea. [Updated 2023 Nov 12]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560834/
- 7Armour, M., Smith, C. A., Steel, K. A., & Macmillan, F. (2019). The effectiveness of self-care and lifestyle interventions in primary dysmenorrhea: a systematic review and meta-analysis. BMC complementary and alternative medicine, 19(1), 22. https://doi.org/10.1186/s12906-019-2433-8
- 8Proctor, M. L., & Murphy, P. A. (2001). Herbal and dietary therapies for primary and secondary dysmenorrhoea. The Cochrane database of systematic reviews, (3), CD002124. https://doi.org/10.1002/14651858.CD002124

