Osteochondritis Dissecans is a disease of joints with multifactorial causes. It mostly affects people in their teenage life, and the symptoms vary from person to person. Early diagnoses and adequate management are necessary for favorable results in osteochondritis dissecans.
What is Osteochondritis Dissecans?
Osteochondritis dissecans, also known as the osteochondritis lesion, is an idiopathic joint disorder mostly developing in teenagers. In this disease, a small fragment of bone or cartilage gets separated from its articular surface. The loose piece of bone or cartilage lodges in the knee, elbow, or ankle joint, leading to unfavorable symptoms. The bone from which the fragment gets separated doesn’t undergo ischemia (restricted blood supply), thereby maintaining its normal vascularity. The separation of bone and cartilage can make the affected joint unsteady and unstable. Symptoms of this condition depend upon the severity of the lesion, and untreated cases make the lesion complicated by developing degenerative changes in the joint.1Chau, M. M., Klimstra, M. A., Wise, K. L., Ellermann, J. M., Tóth, F., Carlson, C. S., Nelson, B. J., & Tompkins, M. A. (2021). Osteochondritis Dissecans: Current Understanding of Epidemiology, Etiology, Management, and Outcomes. The Journal of bone and joint surgery. American volume, 103(12), 1132–1151. https://doi.org/10.2106/JBJS.20.01399
Etiology of Osteochondritis Dissecans
This condition doesn’t have a single reason or factor behind it. It is caused by multifactorial elements, and a specific factor has not yet been identified. Some factors responsible are:
Trauma:
Direct and indirect trauma to the knee joint can cause osteochondritis dissecans. Sometimes, repetitive internal rotation of the tibia during any activity or exercise irritates the tibial spine on the lateral aspect of the medial femoral condyle. The impingement of the tibial spine is one contributing factor in causing this condition.
Osteochondritis dissecans in the ankle joint also occurs mostly due to any traumatic insult. Partial dislocation of the tibia and talar bone causes the talar to ping on the tibia and fibula, resulting in osteochondritis dissecans of the ankle joint. Some studies show that when your ankle joint is plantar flexed (sole downward) and you invert your ankle joint, it results in posteromedial talar lesions. Similarly, when you invert a dorsiflexed (sole upward) ankle, the talus puts pressure on the fibula, leading to anterolateral lesions. All of these lesions ultimately lead to osteochondritis dissecans of the ankle joint.
Osteochondritis dissecans in the elbow joint mostly occurs in baseball or racquet sports players. Repetitive forceful movement of your arm during sports produces microtrauma, which becomes a cause of osteochondritis dissecans. Sometimes, a single forceful trauma to your elbow is enough to cause osteochondritis dissecans. The pressure is produced between the radial head and capitellum (lateral part of humeral condyle ), causing osteochondral changes in the elbow joint.
Genetic causes:
Genetic factors don’t play a great role in causing osteochondritis dissecans. Some studies show the relation of osteochondritis dissecans in the knee with familial history as well as in twins.
Ischemia:
Ischemia or decreased blood supply is one of the important etiology behind osteochondritis dissecans. Compromise of the blood supply to a subchondral bone increases its vulnerability, making it prone to getting fractured by trauma. Ultimately, a fracture of the subchondral bone causes its detachment from the articular surface.2Bruns, J., Werner, M., & Habermann, C. (2018). Osteochondritis Dissecans: Etiology, Pathology, and Imaging with a Special Focus on the Knee Joint. Cartilage, 9(4), 346–362. https://doi.org/10.1177/1947603517715736
Epidemiology of Osteochondritis Dissecans
Out of 10000 cases in the US, almost six men and three women get osteochondritis dissecans in their femoral condyles. The incidence of osteochondritis dissecans is higher in men than women and 75% of cases develop in the knee joint. The elbow and ankle joint have less incidence than the knee joint. While looking closely at the knee joint, studies show that 75% of the cases of osteochondritis dissecans occur in the femoral condyle.3Kessler, J. I., Jacobs, J. C., Jr, Cannamela, P. C., Weiss, J. M., & Shea, K. G. (2018). Demographics and Epidemiology of Osteochondritis Dissecans of the Elbow Among Children and Adolescents. Orthopedic journal of sports medicine, 6(12), 2325967118815846. https://doi.org/10.1177/2325967118815846
Stages of Osteochondritis Dissecans
Osteochondritis dissecans progress from four stages if it is not treated properly and well on time. These stages are:4Takahara, M., Uno, T., Maruyama, M., Harada, M., Satake, H., Takahara, D., & Takagi, M. (2022). Staging of osteochondritis dissecans of the elbow based on pathologic progression in the partially detached articular fragment. Journal of shoulder and elbow surgery, 31(2), 391–401. https://doi.org/10.1016/j.jse.2021.08.006
Stage l:
Stage I is the stage in which the affected subchondral bone only undergoes compression in a small area after a trauma. If the pain associated with compression is taken seriously, this stage doesn’t progress further.
Stage ll:
Stage II develops when the compressed subchondral bone partially separates from its original epiphyseal line. Radiographs demonstrate this stage by a radiolucent line between the detached part and the original surface of the bone.
Stage III:
Osteochondritis dissecans cases are mostly diagnosed at this stage. At stage III, the subchondral bone completely detaches from its surface, but it remains in the compression of bone.
Stage lV:
In stage IV, the separated part of the bone becomes a loose body by being detached from its original site.5Andriolo, L., Solaro, L., Altamura, S. A., Carey, J. L., Zaffagnini, S., & Filardo, G. (2022). Classification Systems for Knee Osteochondritis Dissecans: A Systematic Review. Cartilage, 13(3), 19476035221121789. https://doi.org/10.1177/19476035221121789
Symptoms of Osteochondritis Dissecans
Symptoms of osteochondritis dissecans entirely depend upon its stage. In the early stages of osteochondritis dissecans, you experience nonspecific and vague symptoms as well as mild pain and swelling of the joint being involved. With the progression of the stage, symptoms also progress toward severity. Mild pain changes into severe pain, and swelling might increase, too. Pain that does not decrease in intensity with time favors the presence of a loose body in the joint, and the patient can even palpate it. In addition to this, later stages of osteochondritis dissecans present with the following intermittent symptoms and are associated with strenuous activity:
Locking:
It is when you can’t move the joint from one position to another, such as by straightening or bending. Sometimes, pain makes it impossible to move the joint, causing a locked joint. Locking mostly involves the knee joint, as it is a weight-bearing joint of your body.
Catching:
This condition also causes joint catching, in which you feel something getting caught in the joint when you try to bend it from a straight position. X-ray and MRI of the joint help diagnose it.
Giving away:
The joint instability causes a sudden loss of support during heavy exercises.6Konarski, W., Poboży, T., Konarska, K., Derczyński, M., & Kotela, I. (2024). Understanding Osteochondritis Dissecans: A Narrative Review of the Disease Commonly Affecting Children and Adolescents. Children (Basel, Switzerland), 11(4), 498. https://doi.org/10.3390/children11040498
How to diagnose Osteochondritis Dissecans?
Physicians make the diagnosis of osteochondritis dissecans by the following protocol:
History & Examination:
The first step to diagnosing any disease is to ask the patient about his symptoms and the nature, intensity, and frequency of those symptoms. Physical examination of the joints is crucial in osteochondritis dissecans.
The first physical examination focuses on the patient’s gait. The gait is abnormal in patients with this condition, as they tend to rotate the affected leg externally. A change in gait helps them walk without pain, as it prevents the tibial spine from striking the condyle.
Checking the integrity of the quadriceps muscle is crucial as it may undergo atrophy or weakness in osteochondritis dissecans.
Wilson test for the medial femoral condyle is performed in patients with osteochondritis dissecans. Your physician asks you to flex the knee to 90 degrees and internally rotate the tibia while slowly extending the knee. When the knee is extended 30 degrees of flexion, you experience pain.
Osteochondritis dissecans in the ankle and elbow joints show physical signs of tenderness and swelling along with a clear history of trauma or repetitive movement. These joints also present with effusion and crepitus (grating sound).
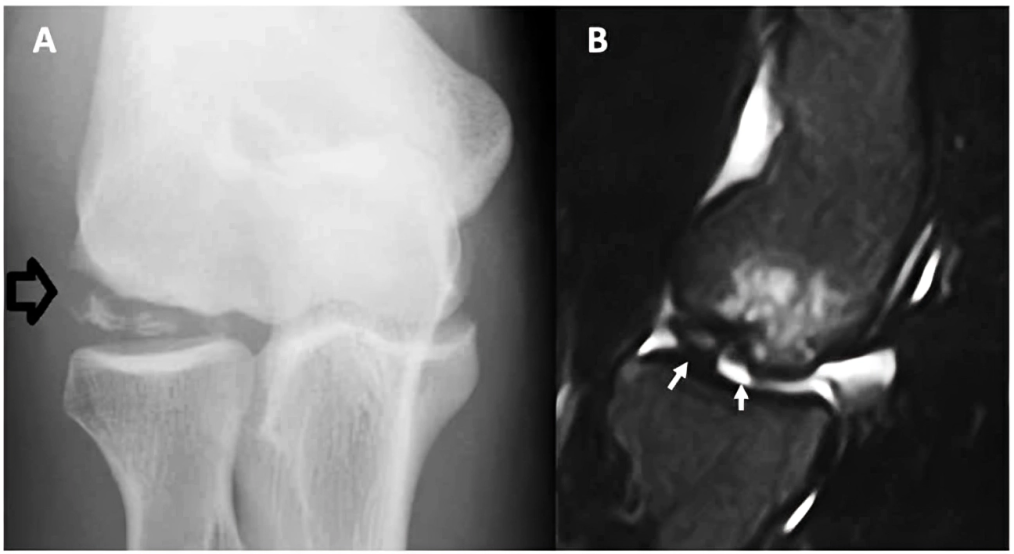
Plain Radiographs:
The first line of investigation is plain radiography. Early stages of OCD do not show any signs in a radiograph, but as the stage progresses, it shows lucency in the epiphyseal part of the bone. A posteroanterior view of a knee joint shows a notch or tunnel in osteochondritis dissecans.
Relationships between Iron Status and Selected Physical Fitness Components of South African Adolescents: The PAHL-Study” by authors from the Children journal, published by MDPI, licensed under CC BY 4.0
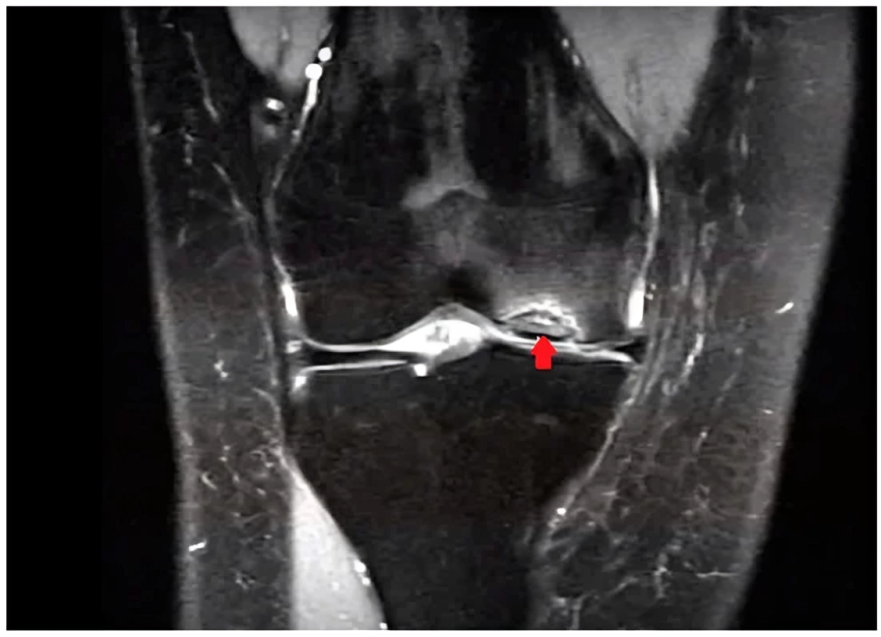
MRI:
MRI visualizes the lesions that are not easily detected by plain radiographs. It shows the displaced part of the bone and also the degree of its displacement. Radiologists use gadolinium injection into the articular surface of the joint before doing an MRI as it makes MRI more specific and sensitive.7Lehner, K., Heuck, A., Rodammer, G., Raff, W., & Haller, W. (1987). MRI bei der Osteochondrosis dissecans [MRI in osteochondrosis dissecans]. RoFo : Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin, 147(2), 191–195. https://doi.org/10.1055/s-2008-1048620
Relationships between Iron Status and Selected Physical Fitness Components of South African Adolescents: The PAHL-Study” by authors from the Children journal, published by MDPI, licensed under CC BY 4.0
Scintigraphy:
Scintigraphy helps in evaluating the prognosis of osteochondritis dissecans. The uptake of technetium by the bone determines the healing of a detached body—the more the uptake, the more the chances of a speedy recovery. Scintigraphy gives a guided treatment to the doctors as it clearly shows whether the lesion needs conservative or surgical management. 8McCullough, R. W., Gandsman, E. J., Litchman, H. E., & Schatz, S. L. (1988). Dynamic bone scintigraphy in osteochondritis dissecans. International orthopedics, 12(4), 317–322. https://doi.org/10.1007/BF00317831
Ultrasound:
Ultrasound is less valuable than MRI and plain radiographs in diagnosing osteochondritis dissecans. It is mostly used for the knee joint and humeral capitellum. It may show some signs of OCD in the capitellum of the humerus bone if performed by a qualified sonologist.
Arthroscopy:
Some doctors recommend arthroscopy for knee, elbow, and ankle joints in cases not easily diagnosed by any other investigation tool. An arthroscopy involves inserting a narrow tube with a video camera into the affected joint. The procedure visualizes the loose part and also aids in repairing damaged ligaments.
It is a minimally invasive procedure with only two incisions, which gives it an advantage over open surgery.9Gowd, A. K., Beck, E. C., Nabor, D., & Waterman, B. R. (2020). A Staged Arthroscopic Approach to Fixation of Unstable Osteochondritis Dissecans in the Medial Femoral Condyle of the Knee Using Nonabsorbable Fixation Screws. Arthroscopy techniques, 9(4), e477–e481. https://doi.org/10.1016/j.eats.2019.11.021
How to treat & manage Osteochondritis Dissecans?
Treatment depends upon the disease’s location and stage. Severe stages require surgical management, but conservative measures are enough to treat early stages.
Conservative Management:
Treatment of osteochondritis dissecans in joints depends upon the age of the patient and its location. Children and people with weak bones having a normal radiograph of the knee joint benefit from conservative management. It involves complete rest and avoidance of heavy exercises for at least three months. A knee immobilizer helps to avoid the progression of this condition in children. The doctor advises surgical intervention if the patient is still symptomatic after three months.10NOVOTNY H. (1951). Preventive and conservative treatment of osteochondrosis dissecans. Acta orthopaedica Scandinavica, 21(1-4), 40–54. https://doi.org/10.3109/17453675108991189

Treatment of OCD in the ankle is based on the radiographic findings and location. People with normal X-ray findings and having a minor detachment undergo conservative management for at least 12 weeks. The medial lesion is more severe than the lateral lesion of the knee joint. Therefore, people with medial lesions and completely detached fragments of bone can benefit only from conservative measures for almost six months. However, with lateral lesions and a severe form of detachment, surgical management becomes necessary. Osteochondritis dissecans in the elbow joint almost always requires avoidance of exercise. 11Tajika, T., Kuboi, T., Endo, F., Hatori, Y., Saida, R., Shitara, H., Nakajima, I., Kamata, M., & Chikuda, H. (2021). Successful Nonoperative Treatment of Osteochondritis Dissecans of the Humeral Capitellum in a Young Baseball Player with Advanced Skeletal Maturity. Progress in rehabilitation medicine, 6, 20210044. https://doi.org/10.2490/prm.20210044
Surgical Therapy:
Surgical therapy is suitable for those people who have symptomatic disease, and conservative treatment does not do any benefit. Moreover, people having the disease in weight-bearing joints, such as the knee joint, even without symptoms, should undergo surgical intervention as it may lead to serious degenerative problems.
Preoperatively, it is crucial to know that the patient is fulfilling all the indications of surgery. Surgical options for osteochondritis dissecans are:12Pascual-Garrido, C., McNickle, A. G., & Cole, B. J. (2009). Surgical treatment options for osteochondritis dissecans of the knee. Sports Health, 1(4), 326–334. https://doi.org/10.1177/1941738109334216
- Arthroscopic subchondral drilling
- Arthroscopic debridement and fragment stabilization
- Excision, curettage, and drilling
- Open removal of loose bodies
- Radical removal of sclerotic bone with grafting
- Chondrocyte transplantation
Osteochondrosis Vs. Osteochondritis Dissecans
Symptoms of both diseases almost correlate, such as swelling, tenderness, and limitation of movement, but they differ in many ways.
Osteochondrosis is an abnormal arrangement of bone growth that resolves on its own with time. At the same time, osteochondritis dissecans involve a detached bony part, and it needs surgical management in severe cases.
Osteochondrosis mostly involves the ossification center of your bones in the epiphyses (the end part of a long bone). Radiological evidence suggests that Osteochondrosis is due to ischemic changes in the center of ossification leading to necrosis. On the other hand, osteochondritis dissecans affect the knee, ankle, and elbow joints due to the lodgement of separated parts of bone.13Rothschild, B. M., & Wayne Lambert, H. (2021). Distinguishing between congenital phenomena and traumatic experiences: Osteochondrosis versus osteochondritis. Journal of Orthopaedics, 23, 185–190. https://doi.org/10.1016/j.jor.2021.01.006
Prognosis of Osteochondritis Dissecans
The prognosis of osteochondritis depends upon the patient’s age, the disease’s severity, and the surgical approach chosen. Adults and teenagers have a better prognosis of osteochondritis than elderly patients. Conservative measures, such as immobilization, easily manage the early stages of the disease, but the later stages require surgery, especially in weight-bearing areas.
Moreover, the surgical approach used to treat osteochondritis dissecans also impacts its prognosis, such as fixation with bone pegs, which has nearly 100 percent effectiveness in treating knee OCD. 14Bangert, Y., Zarembowicz, P., Engelleiter, K., Gkarilas, E., Schmitt, H., Renkawitz, T., & Jaber, A. (2023). Long-Term Outcome and Athletic Level Following Operative Treatment for Osteochondritis Dissecans of the Knee in Pediatric and Adolescent Patients. Journal of Clinical Medicine, 12(12), 4140. https://doi.org/10.3390/jcm12124140
Conclusion
In conclusion, this condition develops due to the separation of cartilage from bone and becoming a loose body. The loose body either remains in its bed or lodges to any other site, causing symptoms like pain, swelling, locking, giving away, and catching in the affected joint. Osteochondritis dissecans develop due to trauma, genetic factors, or decreased blood supply. Conservative measures such as avoiding triggering movement and immobilizing affected joints go a long way in treating this condition. If conservative measures fail, you can choose the surgical option to treat OCD. Proper care is necessary after surgery to avoid complications like infection, neurovascular injuries, and arthritis.
Refrences
- 1Chau, M. M., Klimstra, M. A., Wise, K. L., Ellermann, J. M., Tóth, F., Carlson, C. S., Nelson, B. J., & Tompkins, M. A. (2021). Osteochondritis Dissecans: Current Understanding of Epidemiology, Etiology, Management, and Outcomes. The Journal of bone and joint surgery. American volume, 103(12), 1132–1151. https://doi.org/10.2106/JBJS.20.01399
- 2Bruns, J., Werner, M., & Habermann, C. (2018). Osteochondritis Dissecans: Etiology, Pathology, and Imaging with a Special Focus on the Knee Joint. Cartilage, 9(4), 346–362. https://doi.org/10.1177/1947603517715736
- 3Kessler, J. I., Jacobs, J. C., Jr, Cannamela, P. C., Weiss, J. M., & Shea, K. G. (2018). Demographics and Epidemiology of Osteochondritis Dissecans of the Elbow Among Children and Adolescents. Orthopedic journal of sports medicine, 6(12), 2325967118815846. https://doi.org/10.1177/2325967118815846
- 4Takahara, M., Uno, T., Maruyama, M., Harada, M., Satake, H., Takahara, D., & Takagi, M. (2022). Staging of osteochondritis dissecans of the elbow based on pathologic progression in the partially detached articular fragment. Journal of shoulder and elbow surgery, 31(2), 391–401. https://doi.org/10.1016/j.jse.2021.08.006
- 5Andriolo, L., Solaro, L., Altamura, S. A., Carey, J. L., Zaffagnini, S., & Filardo, G. (2022). Classification Systems for Knee Osteochondritis Dissecans: A Systematic Review. Cartilage, 13(3), 19476035221121789. https://doi.org/10.1177/19476035221121789
- 6Konarski, W., Poboży, T., Konarska, K., Derczyński, M., & Kotela, I. (2024). Understanding Osteochondritis Dissecans: A Narrative Review of the Disease Commonly Affecting Children and Adolescents. Children (Basel, Switzerland), 11(4), 498. https://doi.org/10.3390/children11040498
- 7Lehner, K., Heuck, A., Rodammer, G., Raff, W., & Haller, W. (1987). MRI bei der Osteochondrosis dissecans [MRI in osteochondrosis dissecans]. RoFo : Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin, 147(2), 191–195. https://doi.org/10.1055/s-2008-1048620
- 8McCullough, R. W., Gandsman, E. J., Litchman, H. E., & Schatz, S. L. (1988). Dynamic bone scintigraphy in osteochondritis dissecans. International orthopedics, 12(4), 317–322. https://doi.org/10.1007/BF00317831
- 9Gowd, A. K., Beck, E. C., Nabor, D., & Waterman, B. R. (2020). A Staged Arthroscopic Approach to Fixation of Unstable Osteochondritis Dissecans in the Medial Femoral Condyle of the Knee Using Nonabsorbable Fixation Screws. Arthroscopy techniques, 9(4), e477–e481. https://doi.org/10.1016/j.eats.2019.11.021
- 10NOVOTNY H. (1951). Preventive and conservative treatment of osteochondrosis dissecans. Acta orthopaedica Scandinavica, 21(1-4), 40–54. https://doi.org/10.3109/17453675108991189
- 11Tajika, T., Kuboi, T., Endo, F., Hatori, Y., Saida, R., Shitara, H., Nakajima, I., Kamata, M., & Chikuda, H. (2021). Successful Nonoperative Treatment of Osteochondritis Dissecans of the Humeral Capitellum in a Young Baseball Player with Advanced Skeletal Maturity. Progress in rehabilitation medicine, 6, 20210044. https://doi.org/10.2490/prm.20210044
- 12Pascual-Garrido, C., McNickle, A. G., & Cole, B. J. (2009). Surgical treatment options for osteochondritis dissecans of the knee. Sports Health, 1(4), 326–334. https://doi.org/10.1177/1941738109334216
- 13Rothschild, B. M., & Wayne Lambert, H. (2021). Distinguishing between congenital phenomena and traumatic experiences: Osteochondrosis versus osteochondritis. Journal of Orthopaedics, 23, 185–190. https://doi.org/10.1016/j.jor.2021.01.006
- 14Bangert, Y., Zarembowicz, P., Engelleiter, K., Gkarilas, E., Schmitt, H., Renkawitz, T., & Jaber, A. (2023). Long-Term Outcome and Athletic Level Following Operative Treatment for Osteochondritis Dissecans of the Knee in Pediatric and Adolescent Patients. Journal of Clinical Medicine, 12(12), 4140. https://doi.org/10.3390/jcm12124140

