“Query fever” or “Q fever” is a rare bacterial infection caused by Coxiella burnetii that generally causes flu-like symptoms (fever, cough, fatigue, headaches, etc.) but may cause serious damage to the heart and other organs. The pathogen resides in the body fluids (urine, milk, amniotic fluid, etc.) of animals like cattle, goats, sheep, etc. Humans acquire the disease when they inhale dust particles contaminated with the bacteria. The disease has acute and chronic manifestations.1Hartzell, J. D., Wood-Morris, R. N., Martinez, L. J., & Trotta, R. F. (2008, May). Q fever: epidemiology, diagnosis, and treatment. In Mayo Clinic Proceedings (Vol. 83, No. 5, pp. 574-579). Elsevier.
Most large outbreaks of the disease have occurred in urban communities.2Tan, T., Heller, J., Firestone, S., Stevenson, M., & Wiethoelter, A. (2024). A systematic review of global Q fever outbreaks. One Health, 18, 100667. The prevalence of C. burnetii in milk ranges from 0% to as high as 95%.3Pexara, A., Solomakos, N., & Govaris, A. (2018). Q fever and prevalence of Coxiella burnetii in milk. Trends in Food Science & Technology, 71, 65-72. Individuals with vascular and heart valve disorders have a higher risk of serious complications. Doctors treat it with antibiotics like doxycycline and hydroxychloroquine, etc.
Why Is It Called Q Fever?
“Query fever” or “Q fever” was named so because in the 1930s and 1940s patients came to doctors with symptoms but the healthcare professionals had no clue about it Therefore, there were many questions and queries regarding the fever cause. Thus, it came to be known as query fever.
Q Fever Symptoms
Coxiella burnetii infection does not necessarily cause disease and most patients do not have any symptoms. When present, symptoms appear 3 to 30 days after exposure to the pathogen. The disease can present as an acute disease or a chronic infection. The chronic form has a higher mortality rate than the acute form i.e., 12-25% and 0.5-1.5%, respectively.
A wide variety of presentations make Q fever’s diagnosis even more challenging.
Acute Q Fever:
Fever & Chills
Raised body temperature is an evident symptom of microbial infections and Query fever is no exception. Fever, chills, and fatigue are commonly seen in patients suffering from the disorder.
 Once inside, the infection can induce a process called hemophagocytosis in which the defense cells of the body (phagocytes) kill the blood cells. This contributes to raised temperatures of the body following C. burnetii infection.4Sağlam, B., Albayrak, M., Acar, A., Yıldız, A., Maral, S., Tığlıoğlu, M., … & Kuş, A. (2020). Q fever as a rare cause of hemophagocytic lymphohistiocytosis: case report. Transfusion and Apheresis Science, 59(4), 102747.
Once inside, the infection can induce a process called hemophagocytosis in which the defense cells of the body (phagocytes) kill the blood cells. This contributes to raised temperatures of the body following C. burnetii infection.4Sağlam, B., Albayrak, M., Acar, A., Yıldız, A., Maral, S., Tığlıoğlu, M., … & Kuş, A. (2020). Q fever as a rare cause of hemophagocytic lymphohistiocytosis: case report. Transfusion and Apheresis Science, 59(4), 102747.
Sweating
The under-diagnosed disorder has a wide variety of presentations. Night sweats can perplex patients. A 55-year-old male developed fever/chills and night sweats following a motor vehicle accident and was diagnosed with Coxiella burnetii infection.5Agostino, T., & Edwards, M. (2024). Q Fever, an Under-Recognized and Under-Diagnosed Disease: A Case Report. Cureus, 16(9), e70283.
Fatigue
Abnormal daily functioning and fatigue are known presentations. Acute Query fever can lead to long-term fatigue and have detrimental effects on your work productivity.6Morroy, G., Keijmel, S. P., Delsing, C. E., Bleijenberg, G., Langendam, M., Timen, A., & Bleeker-Rovers, C. P. (2016). Fatigue following acute Q-fever: a systematic literature review. PloS one, 11(5), e0155884.
Body Aches
Myalgias (muscle aches) and arthralgias (joint pains) by Q fever can hinder your day-to-day activities and reduce your quality of life.7Honarmand, H. (2012). Q Fever: an old but still poorly understood disease. Interdisciplinary perspectives on infectious diseases, 2012(1), 131932.
Headaches
Acute infection can cause severe headache. Several patients report pain in the retro-orbital area. Moreover, photophobia may also accompany headaches and myalgia.8Miller, H. K., Priestley, R. A., & Kersh, G. J. (2021). Q fever: a troubling disease and a challenging diagnosis. Clinical microbiology newsletter, 43(13), 109-118.
Skin Rash
Dermatological symptoms are not uncommon in C. burnetii infections. Many complain of having purple-colored skin rash. In a clinical study, a patient reported developing a nonpururitic (non-itchy) maculopapular reddish rash after infection.9Uribe Pulido, N., Escorcia García, C., Cabrera Orrego, R., Gutiérrez, L. A., & Agudelo, C. A. (2021, October). Acute Q fever with dermatologic manifestations, molecular diagnosis, and no seroconversion. In Open Forum Infectious Diseases (Vol. 8, No. 10, p. ofab458). US: Oxford University Press.
Respiratory Symptoms:
The bacterial infection can also have respiratory manifestations:
Cough
In addition to fever/chills, headache, and night sweats, patients also experience unexplained coughing.10Asamoah, J. K. K., Jin, Z., & Sun, G. Q. (2021). Non-seasonal and seasonal relapse model for Q fever disease with comprehensive cost-effectiveness analysis. Results in Physics, 22, 103889.
Chest Pain & Shortness of Breath
The development of serious symptoms like chest pain and shortness of breath can confuse doctors. Despite its contribution to heart muscle inflammation, Coxiella burnetii infection can mimic myocarditis as seen in a case with acute chest pain and extensive ST elevation.11Hammami, R., Bahloul, A., Charfeddine, S., Feki, W., Ayed, N. B., Abid, L., & Kammoun, S. (2021). Q fever presenting as myocarditis. IDCases, 23, e01056. Chest pain worsens with breathing. Many times the symptoms are indicative of pneumonia.
Gastric Disturbances:
GIT problems also make it to the list of the common Q fever symptoms.
Nausea & Vomiting
Studies of Q fever outbreaks reveal that nausea, vomiting, and diarrhea are associated with flu symptoms in numerous cases.12Tapia, T., Stenos, J., Flores, R., Duery, O., Iglesias, R., Olivares, M. F., … & Hormazabal, J. C. (2020). Evidence of Q fever and rickettsial disease in Chile. Tropical Medicine and Infectious Disease, 5(2), 99.
Diarrhea
The bacterial infection can also upset your stomach and induce watery diarrhea.
Stomach Pain
There can also be abdominal pain along with symptoms of nausea, vomiting, and diarrhea. The abdominal pain is sometimes the result of underlying Q fever-induced hepatitis.13Mekonnen, G. (2020). Review on Q fever: epidemiology, public health importance, and preventive measures. Op Acc J Bio Sci Res, 6(4).
Q Fever Fatigue Syndrome
In some cases, patients experience extreme fatigue for months (or even years) after exposure to the bacterial pathogen.
 The condition is seen in around 20% of the cases and resembles chronic fatigue syndrome and is thus, called Q fever fatigue syndrome.14Raijmakers, R. P., Roerink, M. E., Jansen, A. F., Keijmel, S. P., Gacesa, R., Li, Y., … & Xu, C. J. (2020). Multi-omics examination of Q fever fatigue syndrome identifies similarities with chronic fatigue syndrome. Journal of translational medicine, 18, 1-13. Sufferers experience prolonged joint/muscle aches, night sweats, and headaches as well.
The condition is seen in around 20% of the cases and resembles chronic fatigue syndrome and is thus, called Q fever fatigue syndrome.14Raijmakers, R. P., Roerink, M. E., Jansen, A. F., Keijmel, S. P., Gacesa, R., Li, Y., … & Xu, C. J. (2020). Multi-omics examination of Q fever fatigue syndrome identifies similarities with chronic fatigue syndrome. Journal of translational medicine, 18, 1-13. Sufferers experience prolonged joint/muscle aches, night sweats, and headaches as well.
Chronic Q Fever:
The chronic type of the disease can have grave consequences as it usually affects the heart muscle, heart valves, and blood vessels. Here again, patients experience a wide array of symptoms, depending on the organs involved.
Fever
Unlike the acute form, the chronic type causes persistent low-grade fever.
Night Sweats
Sweating at night continues for a long period.
Weight Loss
Multiple complications caused by chronic Query fever lead to weight loss. Patients suffering from Q fever endocarditis report weight loss and anorexia.15Lago‐Rodriguez, A. E., Fraile‐Ribot, P. A., Amengual‐Antich, I., Gual‐Capllonch, F., & Garcia‐Gasalla, M. (2024). Q Fever Endocarditis: A Challenging Diagnosis in a Patient Referring Weight Loss and Anorexia, and With Granulomas in Gastric Biopsy Specimens. Clinical Case Reports, 12(12), e9635. Moreover, patients with Q fever-related kidney disorders (glomerulonephritis) can also present with severe fatigue, decreased appetite, and weight loss.16Li, Y., Shen, Y., Yang, H., Li, M., Jiang, L., Ma, W., … & Su, T. Q Fever-Related Glomerulonephritis unveiled by Metagenomic Next-Generation.
Fatigue
Reports suggest there is a high incidence of chronic fatigue in patients with chronic Q fever. According to a 6-year follow-up study, more than 60% of individuals were diagnosed with chronic fatigue syndrome after the European Q fever outbreak. Thus, persistent fatigue is an evident feature.17Ankert, J., Frosinski, J., Weis, S., Boden, K., & Pletz, M. W. (2022). Incidence of chronic Q fever and chronic fatigue syndrome: A 6 year follow‐up of a large Q fever outbreak. Transboundary and emerging diseases, 69(4), 2219-2226.
Swelling Of Legs
As chronic Q fever tends to damage the kidneys and the heart, leg swelling can be seen in some long-term patients. A patient with rapidly deteriorating kidney function and leg swelling was diagnosed with Q fever.18Peng, M., Tang, B., Li, F., Deng, Y., Dai, Y., Chen, L., & Liu, W. (2023). A retrospective analysis of Q fever osteomyelitis in children, with recommendations. Microbes and Infection, 25(8), 105189.
Breathing Difficulties
Chronic fever can lead to long-term trouble in breathing. Pleural pain and shortness of breath make life difficult.
Complications Of Q Fever
Serious complications are uncommon, and only 1 to 5% of people (who acquire C. burnetii infection) suffer from life-threatening ailments. Most of the patients have weak immunity or underlying serious health issues.
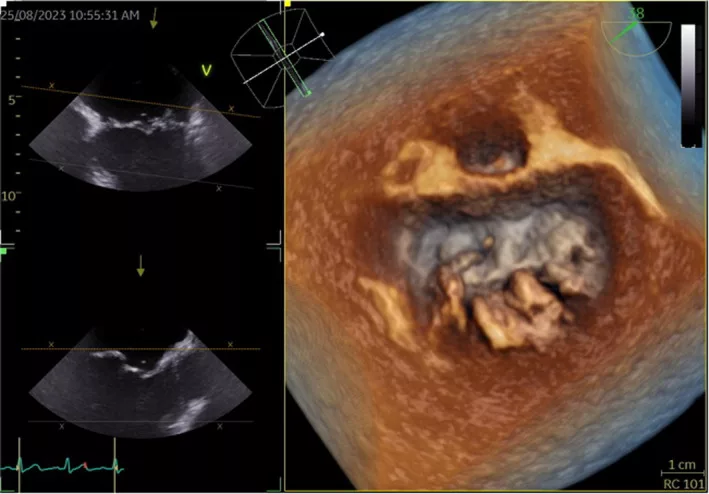
Heart Issues:
Query fever-induced endocarditis is a major complication of the infection. It is mostly seen in patients suffering from heart valve issues or who have a history of endocarditis. Several heart conditions arise due to Coxiella infection.
Endocarditis
Q fever endocarditis refers to inflammation of the inner lining of the heart muscle. It is the most common cardiac manifestation of the disease and can prove to be fatal if left untreated.19Million, M., Thuny, F., Richet, H., & Raoult, D. (2010). Long-term outcome of Q fever endocarditis: a 26-year personal survey. The Lancet Infectious Diseases, 10(8), 527-535.
Myocarditis
Query fever myocarditis (inflammation of the heart muscle) is a rare yet severe manifestation of the disorder. However, it is usually associated with other comorbidities (like kidney failure). It has a poor prognosis if left untreated.20Goyal, A., Dalia, T., Bhyan, P., Farhoud, H., Shah, Z., & Vidic, A. (2022). A rare case of chronic Q fever myocarditis in end-stage heart failure patient: A case report. World Journal of Cardiology, 14(9), 508.
Other heart problems may include pericarditis, arotitis, etc.
Kidneys:
Query fever can harm the kidneys in several ways, which are discussed below:
Q Fever Glomerulonephritis
Inflammation of the kidney structures under bacteria action can lead to severe anemia and impaired renal function. Glomerulonephritis can lead to further complications and prove to be a life-threatening disease. Therefore, timely diagnosis and prompt treatment are crucial for the complete recovery of the patient.21Loyen, M., Wiech, T., Reuter, S., & Thölking, G. (2024). Case report: membranoproliferative glomerulonephritis associated with Q fever causing chronic endocarditis. BMC nephrology, 25(1), 291.
Acute Kidney Injury
Severe acute kidney injury can occur secondary to Coxiella burnetii infection. This can be life-threatening if left untreated.22Stewart, A. G., Broom, J., Sowden, D., & Hollett, P. (2019). Acute kidney injury in acute Q fever. Internal Medicine Journal, 49(10), 1326-1329.
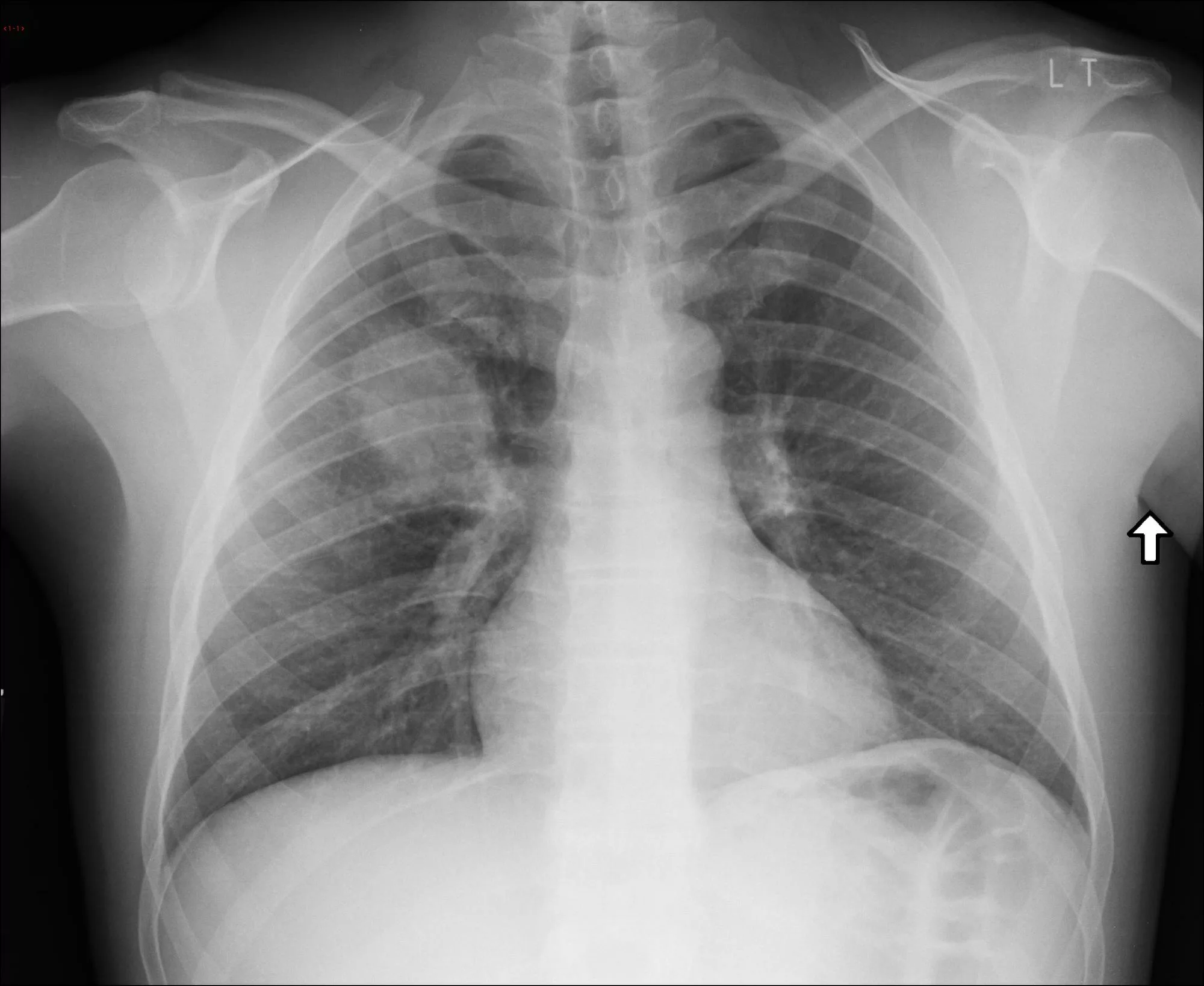
Lungs:
Reports suggest that pulmonary involvement can be seen in both acute and chronic forms. Pulmonary complications may include pneumonia, lung consolidations, pleural effusions, and lymphadenopathy. Radiographic findings of such patients also suggest pulmonary edema.23Kelm, D. J., White, D. B., Fadel, H. J., Ryu, J. H., Maldonado, F., & Baqir, M. (2017). Pulmonary manifestations of Q fever: analysis of 38 patients. Journal of Thoracic Disease, 9(10), 3973.
Brain:
Inflammation from C. burnetii infection can spread to the brain and cause havoc. In rare instances, Query fever can cause the protective lining of the brain (meninges) to swell up and turn into a life-threatening disease.
Neurological conditions like aseptic meningitis and encephalitis are rare complications. However, these conditions demand immediate medical attention, and thus, quick diagnosis is the key to good treatment.24Gu, M., Mo, X., Tang, Z., Tang, J., & Wang, W. (2022). Case report: diagnosis of acute q fever with aseptic meningitis in a patient by using metagenomic next-generation sequencing. Frontiers in Medicine, 9, 855020.
The atypical presentations of the fever (like meningitis and encephalitis) call for better diagnostic procedures like next-generation metagenomic sequencing.25Xing, F., Ye, H., Deng, C., Sun, L., Yuan, Y., Lu, Q., … & Woo, P. C. (2022). Diverse and atypical manifestations of Q fever in a metropolitan city hospital: Emerging role of next-generation sequencing for laboratory diagnosis of Coxiella burnetii. PLoS Neglected Tropical Diseases, 16(4), e0010364.
Bones:
Rarely, it can lay the foundation for bone conditions like osteomyelitis. There have been some cases of Query fever-induced vertebral osteomyelitis that had been diagnosed very late.26Ghanem-Zoubi, N., Karram, T., Kagna, O., Merhav, G., Keidar, Z., & Paul, M. (2021). Q fever vertebral osteomyelitis among adults: a case series and literature review. Infectious Diseases, 53(4), 231-240.
Pregnancy:
C. burnetii infection in pregnant women can lead to complications like pregnancy failures27Wheelhouse, N., Kemp, S., Halliday, J. E., Tingas, E. A., Duncan, W. C., & Horne, A. W. (2022). Q fever and early pregnancy failure: a Scottish case-control study. Reproduction and Fertility, 3(1), L1-L2. and miscarriages.
Q Fever Causes
What Causes Q Fever?
The bacterium Coxiella burnetii is the causative agent for the mysterious Query fever. The animal lives asymptotically in animals like cattle, sheep, and goats that carry the pathogen around. It is present in the following body fluids of the infected animals:
- Urine
- Stool
- Milk
- Amniotic fluid
Contact between the animal and the ground can transfer the bacteria into the soil. Humans become sick if they inhale the infected dust and mist particles.
Transmission & Spread
As already mentioned, the most common type of transfer to humans is via inhalation of contaminated dust/mist particles. Thus, most patients are individuals involved in dealing with livestock farming. Domesticated animals serve as the greatest source of infection for humans.28Espí, A., Del Cerro, A., Oleaga, A., Rodríguez-Pérez, M., López, C. M., Hurtado, A., … & García-Pérez, A. L. (2021). One health approach: An overview of q fever in livestock, wildlife and humans in Asturias (northwestern Spain). Animals, 11(5), 1395.
However, the stubborn pathogen of C. burnetii is capable of traveling some distance and infecting you without coming in contact with animals. Other ways of transmission include:
- Tick bites
- Blood transfusion
- Mother-to-child transmission during pregnancy or childbirth
- Consumption of unpasteurized dairy products like milk and cheese, et
Is Query Fever Contagious?
In most cases, the disease is not contagious. The pathogen may spread via the exchange of body fluids or physical contact. The only means of human-to-human transmission are mother-to-child (during pregnancy) and receiving blood from an infected person.
High Risk Groups
Certain groups of people are at a greater risk of developing severe forms of Q fever. The following people are at a higher risk of chronic Q fever (which is more severe than the acute form):
- Pregnant women
- Individuals with a history of valve disease or endocarditis29Kampschreur, L. M., Oosterheert, J. J., Hoepelman, A. I., Lestrade, P. J., Renders, N. H., Elsman, P., & Wever, P. C. (2012). Prevalence of chronic Q fever in patients with a history of cardiac valve surgery in an area where Coxiella burnetii is epidemic. Clinical and Vaccine Immunology, 19(8), 1165-1169.
- Kidney patients suffering from renal insufficiency
- People who have vascular prostheses (prosthetic devices placed in vessels to keep them open)
- Adults with weak immunity (transplant patients, HIV/Hepatitis patients, people taking immunosuppressant drugs)
Q Fever Diagnosis
Due to the diversity of symptoms and resemblance to other conditions, diagnosing Q fever is very tricky and may take a lot of time (with lots of trials and errors). However, the sequence of diagnosis will be as follows:
History & Physical Examination:
Your healthcare provider will ask about contact or working around animals. He will also inquire about medical history (history of heart valve disease, etc.) and the onset of symptoms. A question regarding a recent visit to a livestock farm may also help solve some questions.
Blood Samples:
If C. burnetii infection is suspected, a small sample of blood is taken and sent to the lab. Multiple tests can be performed at the lab:
Antigen Test
Lab experts use indirect fluorescent antibody (IFA) testing to check C. burnetii antigen in the blood. Multiple samples are taken (1st sample in the first week and 2nd sample 3-6 weeks later).
Antibody Test
Lab technicians detect antibodies (IgG) in the blood (which the body produces as a response to the pathogen). It also uses the IFA method.
PCR Test
Your healthcare provider may also order a Polymerase Chain Reaction (PCR) test to diagnose Q fever within the initial weeks of symptoms onset.
Bacterial Culture
The bacteria from the sample are grown in the lab and seen under a microscope for identification.
Differential Diagnosis:
Brucellosis Vs. Q Fever
Both brucellosis and Q fever are bacterial infections that share some similarities. Brucellosis is caused by Brucella, while Q fever arises due to Coxiella burnetii infection. While you may find fever, fatigue, and sweating in both conditions, the onset of Query fever is abrupt, while that of brucellosis is more gradual. One symptom that sets apart Q fever from brucellosis is headache.
Q Fever Treatment
The first line of treatment for Q fever is antibiotic therapy. Once diagnosed with it, your healthcare provider will prescribe a combination of antibiotics to treat the infection. Doxycycline is the most prevalent drug used to treat infection in adults and children. It is mostly combined with hydroxychloroquine.30España, P. P., Uranga, A., Cillóniz, C., & Torres, A. (2020, August). Q fever (Coxiella burnetii). In Seminars in respiratory and critical care medicine (Vol. 41, No. 04, pp. 509-521). Thieme Medical Publishers. Animal trials show the high efficacy of doxycycline and find levofloxacin as a potent alternative to doxycycline.31Clay, K. A., Hartley, M. G., Armstrong, S., Bewley, K. R., Godwin, K., Rayner, E., … & Norville, I. H. (2021). Evaluation of the efficacy of doxycycline, ciprofloxacin, levofloxacin, and co-trimoxazole using in vitro and in vivo models of Q fever. Antimicrobial Agents and Chemotherapy, 65(11), 10-1128.
Other efficacious drugs for Query fever include fluoroquinolones (like finafloxacin, ofloxacin, etc.),32Hartley, M. G., Norville, I. H., Richards, M. I., Barnes, K. B., Bewley, K. R., Vipond, J., … & Harding, S. V. (2021). Finafloxacin, a novel fluoroquinolone, reduces the clinical signs of infection and pathology in a mouse model of Q fever. Frontiers in Microbiology, 12, 760698. rifampin, clarithromycin, and Trimethoprim-sulfamethoxazole.
Your health professional may also prescribe anti-inflammatory and pain-killer drugs for symptomatic management of the disease.
Most patients respond well to antibiotics. However, only a small amount develops chronic unresolved symptoms that may last for months to years and are hard to cure.
Q Fever Prevention
You can adopt the following steps to keep the infirmity at bay:

- Ask your healthcare provider for a Q fever vaccine if you are in a high-risk area. Currently, the vaccine is only available in Australia. However, it can be managed for other regions.
- Wear protective gear (gloves and mask) when dealing with animal fluids.
- Avoid consuming unpasteurized drinks/food items.
- Get screened for heart valve problems to reduce the risk of infection.
Final Word
Q fever is a rare bacterial infection that has perplexed physicians. Coxiella burnetii is the causative agent that spreads to humans via inhalation of dust particles contaminated with it. In most cases, it has a milder acute form, but it may take a more serious chronic form. The infectious disease causes a wide variety of symptoms, including fever, headache, night sweats, skin rash, extreme fatigue, GIT, and respiratory symptoms. Weight loss and swelling of the legs are seen in chronic Q fever cases.
Farm animals like sheep and goats carry the pathogen in your body fluids (urine, amniotic fluid, milk, etc.). When the fluids mix in soil, they can get inhaled into the human body and cause infection. Diagnosis is difficult due to diverse symptoms but doctors treat the infection well with a combination of antibiotics like doxycycline and hydroxychloroquine, etc. You can prevent the disease by getting a vaccine, avoiding unpasteurized products, and wearing protective gear when dealing with livestock animals.
Refrences
- 1Hartzell, J. D., Wood-Morris, R. N., Martinez, L. J., & Trotta, R. F. (2008, May). Q fever: epidemiology, diagnosis, and treatment. In Mayo Clinic Proceedings (Vol. 83, No. 5, pp. 574-579). Elsevier.
- 2Tan, T., Heller, J., Firestone, S., Stevenson, M., & Wiethoelter, A. (2024). A systematic review of global Q fever outbreaks. One Health, 18, 100667.
- 3Pexara, A., Solomakos, N., & Govaris, A. (2018). Q fever and prevalence of Coxiella burnetii in milk. Trends in Food Science & Technology, 71, 65-72.
- 4Sağlam, B., Albayrak, M., Acar, A., Yıldız, A., Maral, S., Tığlıoğlu, M., … & Kuş, A. (2020). Q fever as a rare cause of hemophagocytic lymphohistiocytosis: case report. Transfusion and Apheresis Science, 59(4), 102747.
- 5Agostino, T., & Edwards, M. (2024). Q Fever, an Under-Recognized and Under-Diagnosed Disease: A Case Report. Cureus, 16(9), e70283.
- 6Morroy, G., Keijmel, S. P., Delsing, C. E., Bleijenberg, G., Langendam, M., Timen, A., & Bleeker-Rovers, C. P. (2016). Fatigue following acute Q-fever: a systematic literature review. PloS one, 11(5), e0155884.
- 7Honarmand, H. (2012). Q Fever: an old but still poorly understood disease. Interdisciplinary perspectives on infectious diseases, 2012(1), 131932.
- 8Miller, H. K., Priestley, R. A., & Kersh, G. J. (2021). Q fever: a troubling disease and a challenging diagnosis. Clinical microbiology newsletter, 43(13), 109-118.
- 9Uribe Pulido, N., Escorcia García, C., Cabrera Orrego, R., Gutiérrez, L. A., & Agudelo, C. A. (2021, October). Acute Q fever with dermatologic manifestations, molecular diagnosis, and no seroconversion. In Open Forum Infectious Diseases (Vol. 8, No. 10, p. ofab458). US: Oxford University Press.
- 10Asamoah, J. K. K., Jin, Z., & Sun, G. Q. (2021). Non-seasonal and seasonal relapse model for Q fever disease with comprehensive cost-effectiveness analysis. Results in Physics, 22, 103889.
- 11Hammami, R., Bahloul, A., Charfeddine, S., Feki, W., Ayed, N. B., Abid, L., & Kammoun, S. (2021). Q fever presenting as myocarditis. IDCases, 23, e01056.
- 12Tapia, T., Stenos, J., Flores, R., Duery, O., Iglesias, R., Olivares, M. F., … & Hormazabal, J. C. (2020). Evidence of Q fever and rickettsial disease in Chile. Tropical Medicine and Infectious Disease, 5(2), 99.
- 13Mekonnen, G. (2020). Review on Q fever: epidemiology, public health importance, and preventive measures. Op Acc J Bio Sci Res, 6(4).
- 14Raijmakers, R. P., Roerink, M. E., Jansen, A. F., Keijmel, S. P., Gacesa, R., Li, Y., … & Xu, C. J. (2020). Multi-omics examination of Q fever fatigue syndrome identifies similarities with chronic fatigue syndrome. Journal of translational medicine, 18, 1-13.
- 15Lago‐Rodriguez, A. E., Fraile‐Ribot, P. A., Amengual‐Antich, I., Gual‐Capllonch, F., & Garcia‐Gasalla, M. (2024). Q Fever Endocarditis: A Challenging Diagnosis in a Patient Referring Weight Loss and Anorexia, and With Granulomas in Gastric Biopsy Specimens. Clinical Case Reports, 12(12), e9635.
- 16Li, Y., Shen, Y., Yang, H., Li, M., Jiang, L., Ma, W., … & Su, T. Q Fever-Related Glomerulonephritis unveiled by Metagenomic Next-Generation.
- 17Ankert, J., Frosinski, J., Weis, S., Boden, K., & Pletz, M. W. (2022). Incidence of chronic Q fever and chronic fatigue syndrome: A 6 year follow‐up of a large Q fever outbreak. Transboundary and emerging diseases, 69(4), 2219-2226.
- 18Peng, M., Tang, B., Li, F., Deng, Y., Dai, Y., Chen, L., & Liu, W. (2023). A retrospective analysis of Q fever osteomyelitis in children, with recommendations. Microbes and Infection, 25(8), 105189.
- 19Million, M., Thuny, F., Richet, H., & Raoult, D. (2010). Long-term outcome of Q fever endocarditis: a 26-year personal survey. The Lancet Infectious Diseases, 10(8), 527-535.
- 20Goyal, A., Dalia, T., Bhyan, P., Farhoud, H., Shah, Z., & Vidic, A. (2022). A rare case of chronic Q fever myocarditis in end-stage heart failure patient: A case report. World Journal of Cardiology, 14(9), 508.
- 21Loyen, M., Wiech, T., Reuter, S., & Thölking, G. (2024). Case report: membranoproliferative glomerulonephritis associated with Q fever causing chronic endocarditis. BMC nephrology, 25(1), 291.
- 22Stewart, A. G., Broom, J., Sowden, D., & Hollett, P. (2019). Acute kidney injury in acute Q fever. Internal Medicine Journal, 49(10), 1326-1329.
- 23Kelm, D. J., White, D. B., Fadel, H. J., Ryu, J. H., Maldonado, F., & Baqir, M. (2017). Pulmonary manifestations of Q fever: analysis of 38 patients. Journal of Thoracic Disease, 9(10), 3973.
- 24Gu, M., Mo, X., Tang, Z., Tang, J., & Wang, W. (2022). Case report: diagnosis of acute q fever with aseptic meningitis in a patient by using metagenomic next-generation sequencing. Frontiers in Medicine, 9, 855020.
- 25Xing, F., Ye, H., Deng, C., Sun, L., Yuan, Y., Lu, Q., … & Woo, P. C. (2022). Diverse and atypical manifestations of Q fever in a metropolitan city hospital: Emerging role of next-generation sequencing for laboratory diagnosis of Coxiella burnetii. PLoS Neglected Tropical Diseases, 16(4), e0010364.
- 26Ghanem-Zoubi, N., Karram, T., Kagna, O., Merhav, G., Keidar, Z., & Paul, M. (2021). Q fever vertebral osteomyelitis among adults: a case series and literature review. Infectious Diseases, 53(4), 231-240.
- 27Wheelhouse, N., Kemp, S., Halliday, J. E., Tingas, E. A., Duncan, W. C., & Horne, A. W. (2022). Q fever and early pregnancy failure: a Scottish case-control study. Reproduction and Fertility, 3(1), L1-L2.
- 28Espí, A., Del Cerro, A., Oleaga, A., Rodríguez-Pérez, M., López, C. M., Hurtado, A., … & García-Pérez, A. L. (2021). One health approach: An overview of q fever in livestock, wildlife and humans in Asturias (northwestern Spain). Animals, 11(5), 1395.
- 29Kampschreur, L. M., Oosterheert, J. J., Hoepelman, A. I., Lestrade, P. J., Renders, N. H., Elsman, P., & Wever, P. C. (2012). Prevalence of chronic Q fever in patients with a history of cardiac valve surgery in an area where Coxiella burnetii is epidemic. Clinical and Vaccine Immunology, 19(8), 1165-1169.
- 30España, P. P., Uranga, A., Cillóniz, C., & Torres, A. (2020, August). Q fever (Coxiella burnetii). In Seminars in respiratory and critical care medicine (Vol. 41, No. 04, pp. 509-521). Thieme Medical Publishers.
- 31Clay, K. A., Hartley, M. G., Armstrong, S., Bewley, K. R., Godwin, K., Rayner, E., … & Norville, I. H. (2021). Evaluation of the efficacy of doxycycline, ciprofloxacin, levofloxacin, and co-trimoxazole using in vitro and in vivo models of Q fever. Antimicrobial Agents and Chemotherapy, 65(11), 10-1128.
- 32Hartley, M. G., Norville, I. H., Richards, M. I., Barnes, K. B., Bewley, K. R., Vipond, J., … & Harding, S. V. (2021). Finafloxacin, a novel fluoroquinolone, reduces the clinical signs of infection and pathology in a mouse model of Q fever. Frontiers in Microbiology, 12, 760698.