Rotator cuff tendinitis or tendinopathy is the inflammation of the rotator cuff tendon. It is also known as “Impingement,” “Bursitis,” or “Biceps Tendinitis.”
It occurs due to inflammation of the rotator cuff tendons and bursa, which causes pain and swelling of these tendons. If injury to the shoulder joint is recurrent and persisting, it leads to rotator cuff tendinosis.
What Is Rotator Cuff Tendinitis?
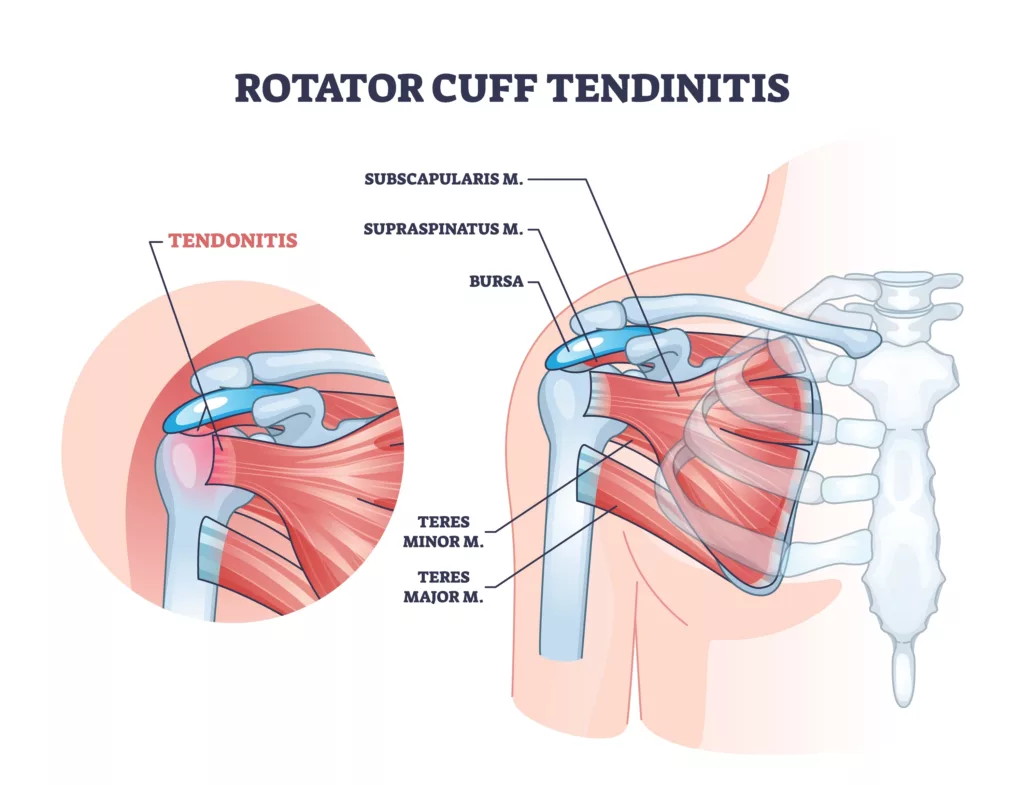
The upper arm is connected to the shoulder by muscles and tendons. Four tendons form the rotator cuff: the Supraspinatus, Infraspinatus, teres minor, and Subscapularis tendon. Rotator cuff tendinitis is the inflammation of these tendons. Its major causes include repetitive injury and long-term irritation. Rotator cuff injuries commonly cause pain and an inability to perform well in athletes.1Weiss, L. J., Wang, D., Hendel, M., Buzzerio, P., & Rodeo, S. A. (2018). Management of Rotator Cuff Injuries in the Elite Athlete. Current reviews in musculoskeletal medicine, 11(1), 102–112. https://doi.org/10.1007/s12178-018-9464-5
Causes Of Rotator Cuff Tendinitis
The following are the causes of rotator cuff tendinitis:
Rotator Cuff Impingement Syndrome
Rotator cuff tendinitis is most commonly seen with rotator cuff impingement syndrome. It is also called rotator cuff impingement syndrome, which manifests as bursitis and tendinopathy and results in tears of full thickness in your rotator cuff. In impingement, your bones rub against your rotator cuff tendon repeatedly, which leads to rotator cuff tendinitis. Compression and degeneration of the tendons are common causes.2Harrison, A. K., & Flatow, E. L. (2011). Subacromial impingement syndrome. The Journal of the American Academy of Orthopaedic Surgeons, 19(11), 701–708. https://doi.org/10.5435/00124635-201111000-00006
Rotator cuff impingement syndrome and rotator cuff tendinitis are common in young adults.
Overuse of the Joint
Overuse of your joint is a common cause of rotator cuff tendinitis. When you perform a certain action on your shoulder joint repeatedly, it causes stress on the joint, and tendinitis occurs.
Overhead Movement of the Shoulders
When you perform overhead shoulder movements, like turning or twisting your shoulders with your arms raised, it causes rotator cuff tendinitis. Athletes perform such movements repeatedly during their practice, which results in tendinitis.
Trauma
Traumas like high-energy falls on arms, accidents, and sports injuries are common causes of rotator cuff tendinitis.
Idiopathic
Rotator cuff tendinitis occurs in some patients without any obvious or known cause.
Sports
People who participate in sports such as swimming, tennis, volleyball, badminton, and baseball are more likely to develop rotator cuff tendinitis.
Professions
People in certain professions, such as construction, weight lifting, painting, and hanging dry walls, are more prone to developing rotator cuff tendinitis.
Sleeping Position
Sleeping in the same position on your shoulder every night can lead to rotator cuff tendinitis.
Symptoms Of Rotator Cuff Tendinitis
You may notice the following symptoms if you have rotator cuff tendinitis:
- Pain and swelling in your arms
- Stiffness
- Severe pain in the night that wakes you from sleep even
- Pain in your arm and shoulder when you raise it above the head
- Decrease in movement of your affected arm
- Clicking sounds
- Athletes may feel pain when playing
- Pain that radiates from your shoulder to one side of your arm
- Problems in fine activities like closing the buttons or zips
Types Of Rotator Cuff Tendinitis
There are two types of rotator cuff tendinitis.
Acute Rotator Cuff Tendinitis
Acute rotator cuff occurs suddenly due to a sudden trauma to your shoulder. It is common in athletes who play games like tennis, javelin throw, badminton, and baseball. There is severe pain in acute rotator cuff tendinitis; immediate treatment is essential.
Chronic Rotator Cuff Tendinitis
Chronic rotator cuff tendinitis occurs due to continuous underlying stress on the joints, such as repeated trauma, damage, rub, or degeneration of the tendon.
Extrinsic Compression
Extrinsic compression results in spurring or degeneration that causes impingement and rotator tendinitis.3Neer C. S., 2nd (1983). Impingement lesions. Clinical orthopedics and related research, (173), 70–77.
Degeneration Of Tendons
Intrinsic degeneration of the tendons due to aging is one of the causes of rotator cuff tendinitis. It reduces the stability of glenohumeral joints and results in tendonitis.4Sambandam, S. N., Khanna, V., Gul, A., & Mounasamy, V. (2015). Rotator cuff tears: An evidence-based approach. World journal of orthopedics, 6(11), 902–918. https://doi.org/10.5312/wjo.v6.i11.902
Vascular Changes
Vascular changes occur with age, and the areas of your rotator cuff tendon become thin and lesser in number. Tears and vascular changes occur in the tendons and cause vascular degeneration.5Feeney, M. S., O’dowd, J., Kay, E. W., & Colville, J. (2003). Glenohumeral articular cartilage changes in rotator cuff disease. Journal of shoulder and elbow surgery, 12(1), 20–23. https://doi.org/10.1067/mse.2003.128565
Changes in Joints & Tendons with Age
Changes in your rotator cuff tendon occur with aging, including fiber and myxoid degeneration.6Longo, U. G., Franceschi, F., Ruzzini, L., Rabitti, C., Morini, S., Maffulli, N., Forriol, F., & Denaro, V. (2007). Light microscopic histology of supraspinatus tendon ruptures. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA, 15(11), 1390–1394. https://doi.org/10.1007/s00167-007-0395-8
The frequency of rotator cuff tendinitis increases 5-10 percent during the first twenty years of your age. It increases 30-35 percent in your fifties or sixties and 65 percent in your eighties.
Enormous intrinsic, tensile forces affect your joint chronically and cause rotator cuff tendinitis.
How Is Rotator Cuff Tendinitis Diagnosed?
Rotator cuff tendonitis is diagnosed with the help of a thorough history, examination, and a few investigations. The following steps help diagnose shoulder tendonitis:
History:
If your doctor suspects that you have rotator cuff tendinitis, he will ask the following questions:
- History of trauma to the shoulder, any severe pain, or sudden increase in shoulder pain.
- Does the pain increase when you perform overhead movement of your shoulder joint?
- Does the pain increase at night?
- Stiffness, swelling, or any clicking sounds in the joint?
Examination:
Your doctor will perform a complete general physical examination and examine your rheumatic system to diagnose rotator cuff tendinitis.
Shoulder Examination
Your doctor inspects your shoulder region for scars, redness, visible deformities, or asymmetry. Then, he will check the movements, muscle bulk, symmetry of movements, tenderness, and rupture of membranes.7Bakhsh, W., & Nicandri, G. (2018). Anatomy and Physical Examination of the Shoulder. Sports medicine and arthroscopy review, 26(3), e10–e22. https://doi.org/10.1097/JSA.0000000000000202
Cervical Spine & Neck Examination
Your doctor assesses nerve tests from C5 to T1 dermatome and rotator cuff muscle strength tests.

Supraspinatus Tests:
Jobe’s Tests
In Jobe’s test, when your doctor flexes your arm at 90 degrees, abducts it with your thumb pointing downwards, and applies a downward pressure against resistance, it causes pain or weakness.
Drop Arm Test
The doctor abducts your arm; he initially supports it, but later, he removes the support and checks your ability to maintain the abducted position of your shoulder. A positive test means an inability to maintain an abducted position.8Doxey, R., Thiese, M. S., & Hegmann, K. T. (2018). Reliability of Common Provocative Tests for Shoulder Tendinitis. Journal of occupational and environmental medicine, 60(12), 1063–1066. https://doi.org/10.1097/JOM.0000000000001430
Infraspinatus Tests:
Infraspinatus tests include:
Strength Testing
Your doctor places your shoulder at 90 degrees of abduction, flexes it, and asks you to rotate your elbow externally.
Horn Blower’s Sign
The doctor places your shoulder at 90 degrees of abduction, flexes it, slightly rotates it externally, and asks you to maintain this position.
Subscapularis Tests:
Subscapularis tests include:
Internal Rotator Lag Test
Your doctor flexes your elbow at 90 degrees against your back and externally rotates it by lifting the dorsum of your hands. The test is positive when the patient cannot maintain this position of your joint.
Lift Off Test
In the lift-off test, the doctor flexes your elbow at 90 degrees against your back and resists your ability to lift the dorsum of your hands away from your lower back.
Belly Press
The doctor places your arm at 90 degrees of flexion and performs the internal rotator lag test by asking you to place your thumb against your belly. Initially, the doctor supports the elbow; later, he doesn’t support it and checks your arm’s ability to maintain this position.
External Impingement Tests:
These tests include:
Neer Impingement Test
Your doctor asks you to flex your arm; if it causes pain in your arm beyond 90 degrees, it is a positive Neer Impingement Test.
Hawkins Test
In the Hawkins test, your doctor positions your elbow at 90 degrees. If the internal rotation of the shoulder in this position causes pain, it is a positive Hawkins test.
Radiographs:
Your doctor advises you to get an anteroposterior view (The Grashey view) radiograph of your glenohumeral joint. The doctor checks the acromiohumeral interval.
You can also get a 30-degree caudal tilt view to visualize the acromial spurring.
X-ray Findings
- Acromiohumeral interval less than 7 millimetres
- Calcification of your coracoacromial ligament or coracohumeral ligaments.
- Osteophytes on acromion, humerus, or glenoid
- Acromial spurring
- Cystic degeneration of your greater tuberosity
- Degenerative changes
- Hooked acromion
Ultrasound:
Your doctor may use ultrasound modality to detect rotator cuff tendinitis by visualizing rotator cuff tendon and muscle integrity.
Magnetic Resonance Imaging (MRI):
Magnetic resonance imaging (MRI) gives partial versus full-thickness tear details, as well as the extent, location, degree, and severity of your rotator cuff tendon tears. Your doctor assesses the tears and subacromial impingement by performing magnetic resonance imaging (MRI).9Harrison, A. K., & Flatow, E. L. (2011). Subacromial impingement syndrome. The Journal of the American Academy of Orthopaedic Surgeons, 19(11), 701–708. https://doi.org/10.5435/00124635-201111000-00006
Management Of Rotator Cuff Tendinitis
The treatment options for rotator cuff tendinitis include the following:
Non-Operative Treatment:
Non-operative treatment includes:
Anti Inflammatory Medicines
Non-steroidal anti-inflammatory drugs (NSAIDs) are the first-line treatment for rotator cuff tendinitis. They work by reducing pain, inflammation, and swelling in the joints. They also reduce prostaglandins and other inflammatory mediators.
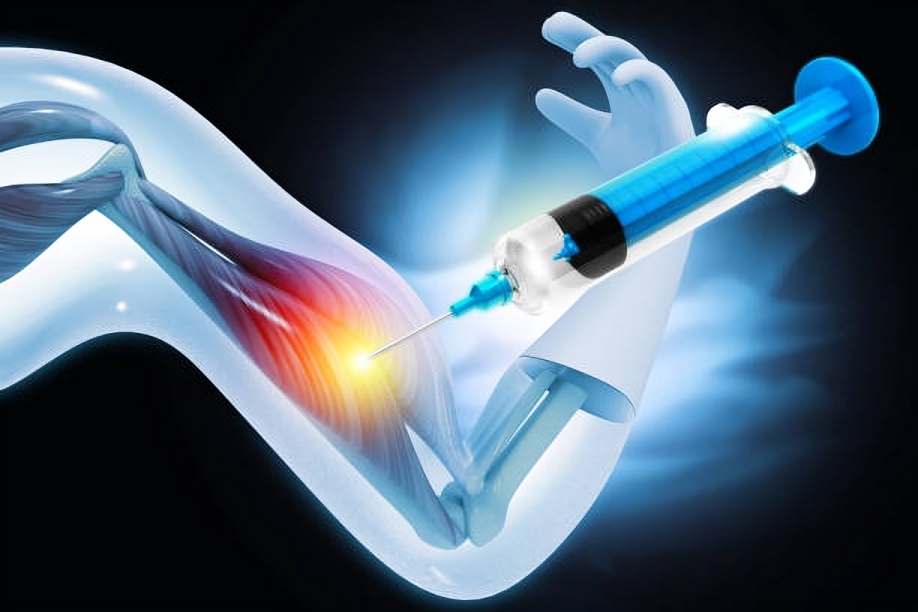
Cortisone Injections
Your doctor may give you a cortisone injection in your subacromial joint space. It provides you with instant pain relief. They work by reducing inflammation, relieving pressure, and suppressing your immunity.

Other Drugs
Muscle relaxants (Cyclobenzaprine), acetaminophen, topical painkillers (Capsaicin), narcotic pain relievers (morphine, codeine) and transcutaneous nerve stimulation are also useful for rotator cuff tendinitis.
Rest
Your doctor will advise you to rest and avoid strenuous exercises, particularly heavy weight lifting, overhead movement, and sports like tennis, badminton, and swimming.
Surgical Management:
Surgical options for treatment of the rotator cuff tendinitis are:
Subacromial Decompression
In subacromial decompression, your doctor debrides your subacromial space. Moreover, they also perform bursectomy and coracoacromial ligament decompression to reduce calcification and fraying.
Acromioplasty
In acromioplasty, the surgeon shaves the undersurface of your acromion to reduce spurring and improve impingement.
Treatment of Os Acromiale
In the case of os acromiale (a developmental defect that occurs due to a lack of osseous union formation between the ossification centers of the acromion), your surgeon will fuse the os Acromiale first, then perform acromioplasty.
Exercises For Rotator Cuff Tendonitis
Your doctor may advise you on some exercises for your thoracic spine, cervical spine, glenohumeral joint, or scapulothoracic joint. Some exercises are:
Pendulum Stretching
Pendulum stretching is also a useful exercise in which you keep your arm straight and close to your body and swing it forward, backward, upward, downward, and side to side.
Pulley Exercise
In this exercise, a pulley system weighing 1 to 1.5 kilograms moves your arm upward slightly for two minutes.
- Hold a rod in the arm that has rotator cuff tendinitis.
- Use your other hand to hold the middle of the rod. This hand will guide the rod and help extend the affected arm.
- Slowly lift the affected arm using the pulley system.
Your doctor advises performing this exercise fifteen to twenty times daily with rest intervals between each set.
Scapular Squeeze
In a scapular squeeze, lie flat on the ground and squeeze your shoulders towards each other, towards the spine, and downwards.
Other exercises include inward rotation, outward rotation, abduction, quadruped, reverse pull, door stretch, and lawn mower exercises.
Rotator Cuff Tendinitis Vs. Rotator Cuff Tears
The following are the main differences between these two conditions:
| Rotator Cuff Tendinitis | Rotator Cuff Tear | |
| Pain | There is chronic pain that increases gradually and worsens with time. | The rotator cuff tear has acute, sudden, sharp, and severe pain. |
| Etiology | There are micro tears and degenerations in your rotator cuff tendon that are beyond repair and cause severe pain and inflammation.
Rotator cuff tendinitis occurs due to repeated, severe trauma that causes impingement and tendinitis. |
In a rotator cuff tear, your tendon is torn and detached from the head of the humerus.
Rotator cuff tear is caused by isolated, severe trauma. |
| Lidocaine Injection test | A local anesthetic is injected into the inflamed bursa. If the strength of the shoulder joint returns to normal after the pain is resolved, it indicates rotator cuff tendonitis. | If the strength of the shoulder joint does not return to normal after blocking pain, it indicates a rotator cuff tear. |
Difference between Rotator Cuff Tendonitis and Calcific Tendonitis
The main difference between calcific tendonitis and rotator cuff tendonitis lies in their causes and effects on the shoulder. Rotator cuff tendonitis, also known as tendinosis, is characterized by inflammation of the shoulder tendons and bursae, which are membrane-lined sacs that facilitate smooth tendon movement across other structures. This condition often results from overuse or injury.
In contrast, calcific tendonitis is caused by the buildup of calcium deposits in the shoulder tendons, leading to severe pain, but it doesn’t directly affect the bursae. However, inflammation of the bursae can occur as a secondary response to calcific tendonitis. It is also called Rotator Cuff Calcific Tendinopathy (RCCT).10Chianca, V., Albano, D., Messina, C., Midiri, F., Mauri, G., Aliprandi, A., Catapano, M., Pescatori, L. C., Monaco, C. G., Gitto, S., Pisani Mainini, A., Corazza, A., Rapisarda, S., Pozzi, G., Barile, A., Masciocchi, C., & Sconfienza, L. M. (2018). Rotator cuff calcific tendinopathy: from diagnosis to treatment. Acta bio-medica : Atenei Parmensis, 89(1-S), 186–196. https://doi.org/10.23750/abm.v89i1-S.7022
Conclusion
Rotator cuff tendinitis is inflammation of the rotator cuff tendon. It occurs due to repeated trauma, sports, overhead movements, and degeneration of the shoulder joints. It is treatable with nonsteroidal anti-inflammatory drugs (NSAIDs), steroids, exercises, and corrective surgery.
Refrences
- 1Weiss, L. J., Wang, D., Hendel, M., Buzzerio, P., & Rodeo, S. A. (2018). Management of Rotator Cuff Injuries in the Elite Athlete. Current reviews in musculoskeletal medicine, 11(1), 102–112. https://doi.org/10.1007/s12178-018-9464-5
- 2Harrison, A. K., & Flatow, E. L. (2011). Subacromial impingement syndrome. The Journal of the American Academy of Orthopaedic Surgeons, 19(11), 701–708. https://doi.org/10.5435/00124635-201111000-00006
- 3Neer C. S., 2nd (1983). Impingement lesions. Clinical orthopedics and related research, (173), 70–77.
- 4Sambandam, S. N., Khanna, V., Gul, A., & Mounasamy, V. (2015). Rotator cuff tears: An evidence-based approach. World journal of orthopedics, 6(11), 902–918. https://doi.org/10.5312/wjo.v6.i11.902
- 5Feeney, M. S., O’dowd, J., Kay, E. W., & Colville, J. (2003). Glenohumeral articular cartilage changes in rotator cuff disease. Journal of shoulder and elbow surgery, 12(1), 20–23. https://doi.org/10.1067/mse.2003.128565
- 6Longo, U. G., Franceschi, F., Ruzzini, L., Rabitti, C., Morini, S., Maffulli, N., Forriol, F., & Denaro, V. (2007). Light microscopic histology of supraspinatus tendon ruptures. Knee surgery, sports traumatology, arthroscopy: official journal of the ESSKA, 15(11), 1390–1394. https://doi.org/10.1007/s00167-007-0395-8
- 7Bakhsh, W., & Nicandri, G. (2018). Anatomy and Physical Examination of the Shoulder. Sports medicine and arthroscopy review, 26(3), e10–e22. https://doi.org/10.1097/JSA.0000000000000202
- 8Doxey, R., Thiese, M. S., & Hegmann, K. T. (2018). Reliability of Common Provocative Tests for Shoulder Tendinitis. Journal of occupational and environmental medicine, 60(12), 1063–1066. https://doi.org/10.1097/JOM.0000000000001430
- 9Harrison, A. K., & Flatow, E. L. (2011). Subacromial impingement syndrome. The Journal of the American Academy of Orthopaedic Surgeons, 19(11), 701–708. https://doi.org/10.5435/00124635-201111000-00006
- 10Chianca, V., Albano, D., Messina, C., Midiri, F., Mauri, G., Aliprandi, A., Catapano, M., Pescatori, L. C., Monaco, C. G., Gitto, S., Pisani Mainini, A., Corazza, A., Rapisarda, S., Pozzi, G., Barile, A., Masciocchi, C., & Sconfienza, L. M. (2018). Rotator cuff calcific tendinopathy: from diagnosis to treatment. Acta bio-medica : Atenei Parmensis, 89(1-S), 186–196. https://doi.org/10.23750/abm.v89i1-S.7022