What is Vulvitis?
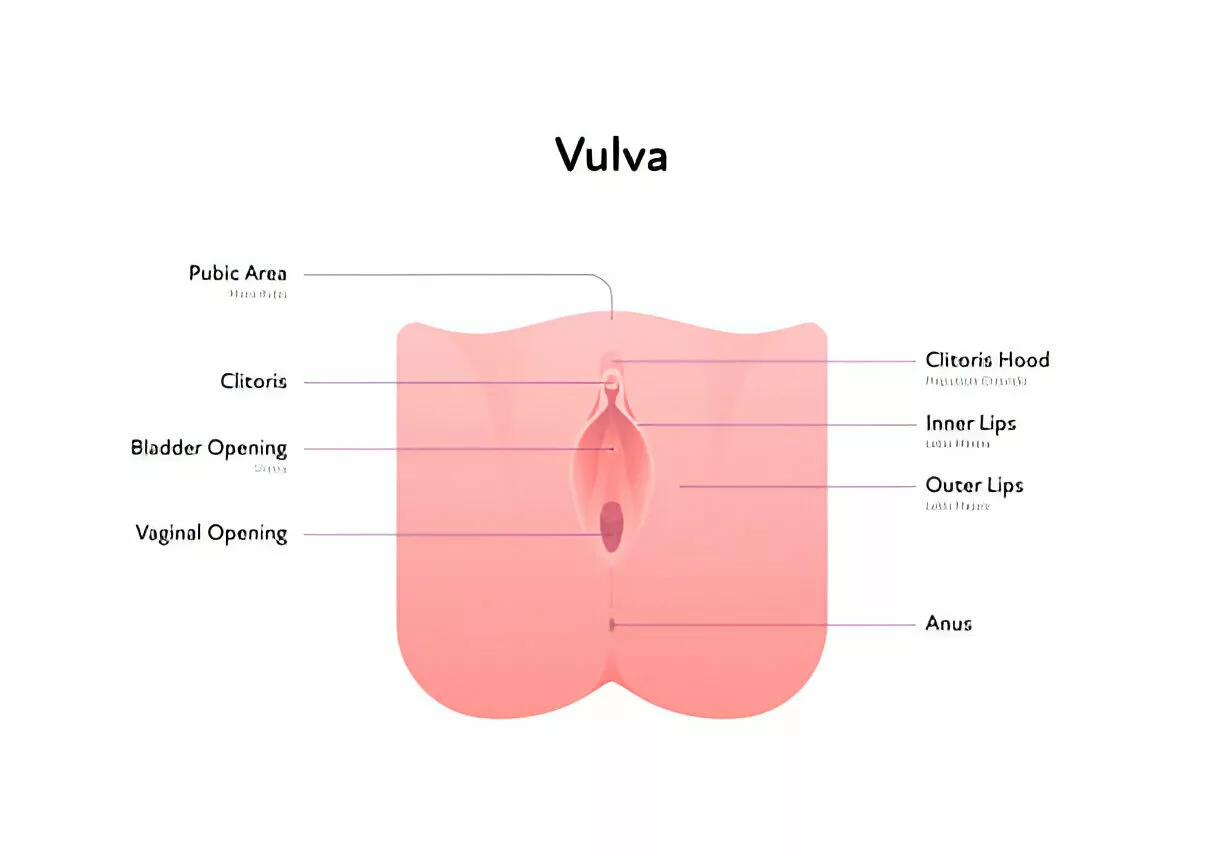
Vulvitis is an inflammation of the vulva caused by an infection, allergy, or injury. The vulva is the external part of the skin of the female genital organ. It is susceptible to inflammation or irritation because of its warm and moist nature. Irritants such as vaginal sprays or fungal infections, dermatitis, stress, poor nutrition, and poor hygiene are causative agents for vulvitis.
Women of any age can be affected by vulvitis, particularly those who have not yet reached puberty (under 13) or are post-menopausal (over 50). This increased susceptibility is primarily due to lower estrogen levels in these age groups. Before puberty and after menopause, estrogen levels drop, leading to thinner, drier vulvar tissues that are more prone to irritation and inflammation.
Symptoms include severe itching, sores, blisters, a burning sensation, thick white patches, redness, and swelling. It can lead to serious impairment of quality of life, impacting sexual function, relationships, sleep, and self-esteem.1Burcham LR, Burcham ZM, Akbari MS, Metcalf JL, Doran KS. Interrelated Effects of Zinc Deficiency and the Microbiome on Group B Streptococcal Vaginal Colonization. mSphere. 2022 Aug 31;7(4):e0026422. doi: 10.1128/msphere.00264-22. Epub 2022, Aug. 9. PMID: 35943198; PMCID: PMC9429885Anti-fungal creams, or topical estrogen creams, are used to relieve vulvitis.
Types of Vulvitis
Vulvitis can be acute or chronic, depending on the duration.
Acute Vulvitis
Acute vulvitis involves sudden inflammation of the vulva, characterized by discomfort and symptoms like itching, burning, redness, swelling, and pain. It can occur due to various factors such as allergic reactions, irritants, hormonal changes, or infections caused by bacteria, viruses, or parasites. Tight clothing, feminine hygiene products, and prolonged moisture exposure can also contribute to acute vulvitis. Treatment usually includes medications like antibacterials, antivirals, or antifungals, along with preventive measures like wearing loose clothing and maintaining good genital hygiene.
Chronic Vulvitis
Chronic vulvitis refers to persistent or long-term inflammation of the vulva, often resulting from untreated acute vulvitis. It leads to increased pain and discomfort over an extended period, ranging from weeks to months or even years. Several factors can contribute to chronic vulvitis, including recurrent bacterial, viral, or fungal infections, hormonal changes (especially postmenopausal estrogen decline), pregnancy, autoimmune conditions like mucous membrane pemphigoid, and zinc deficiency.2Burcham LR, Burcham ZM, Akbari MS, Metcalf JL, Doran KS. Interrelated Effects of Zinc Deficiency and the Microbiome on Group B Streptococcal Vaginal Colonization. mSphere. 2022 Aug 31;7(4):e0026422. doi: 10.1128/msphere.00264-22. Epub 2022, Aug. 9. PMID: 35943198; PMCID: PMC9429885.Managing chronic vulvitis may involve addressing underlying causes and symptoms through appropriate medical intervention and lifestyle adjustments.
Vulvitis Causes
Vulvitis can occur due to several causes, divided into two categories.
Non-Infectious Causes
The non-infectious causes include:
- Dermatitis: It presents with a red, scaly rash and a crack in the skin involving the vulva.
- An allergic reaction to rubber, Condoms, and perfumed oils can cause vulvitis. The vulvitis can be very severe and ulcerative, so pain and burning are the main symptoms.
- Overuse of soap and bubble baths
- Skin Conditions: Dermatological conditions such as eczema, psoriasis, or lichen sclerosus can affect the vulva.
- Atrophic vaginitis: It occurs with the loss of estrogen that occurs before puberty or after the age of 50 and causes physiologic and structural changes within the genital organ that lead to vulvitis.3Raef HS, Elmariah SB. Vulvar Pruritus: A Review of Clinical Associations, Pathophysiology, and Therapeutic Management. Front Med (Lausanne). 2021 Apr 7;8:649402. doi: 10.3389/fmed.2021.649402. PMID: 33898486; PMCID: PMC8058221.
- Frequent horseback or bike riding
- Synthetic underwear or pantyhose without a breathable crotch
- Wearing a wet bathing suit for too long
Infectious Causes
The infectious causes include:
- Fungal infections such as Candida albicans can cause short- or long-term symptoms that always involve the vagina and may also spread to the vulva.
- Parasitic infections such as Trichomonas can cause itching and an offensive discharge, resulting in vulvitis.
- Viral infections, such as Herpes simplex, cause vulvovaginitis, which presents with pain, discrete ulcers, and blisters on the vulva.
- Bacterial infections such as streptococcus may occasionally cause vulvitis with a persistent, non-offensive discharge, which may cause maceration and irritation of the vulval skin. This infection may co-exist with C. albicans.
Risk Factors For Vulvitis
Certain factors increase the risk of vulvitis.
- Women with sensitive skin have a higher response to irritants.
- Women with weak immune systems, i.e., aging or taking certain medications,
- Low level of estrogen as it maintains the integrity of the vulva skin.
- Unprotected sexual intercourse increases the chances of getting vulvitis.
Vulvitis Symptoms
Symptoms are often not a reliable clue to diagnosis, and patients with a variety of different conditions may experience similar symptoms,4Nappi RE, Martini E, Cucinella L, Martella S, Tiranini L, Inzoli A, Brambilla E, Bosoni D, Cassani C, and Gardella B. Addressing Vulvovaginal Atrophy (VVA) and Genitourinary Syndrome of Menopause (GSM) for Healthy Aging in Women. Front Endocrinol (Lausanne). 2019 Aug 21;10:561. doi: 10.3389/fendo.2019.00561. PMID: 31496993; PMCID: PMC6712495. so a physical examination or any diagnostic test should also be done. But commonly, vulvitis presents with the following symptoms:
- Severe itching
- Burning sensation during urination
- Thick white patches on the skin of the vulva.
- Swelling Blisters
- Vaginal discharge
- Dyspareunia (Painful Intercourse)
- Soreness
- Dysuria (A painful, stinging, or burning sensation during urination)
- Softening and breaking down of skin resulting from prolonged exposure to moisture
Diagnosis of Vulvitis
As the treatment will be based on the etiology of the patient’s condition, the first step is to make a correct diagnosis. Initially, a thorough assessment is conducted, including a detailed medical and pregnancy history. A physical examination of the vulva is performed to identify any rash, blisters, or discharge. Additionally, pH testing of vaginal secretions using color-pH indicator strips may be carried out.5Fischer G. Treatment of vaginitis and vulvitis. Australian Prescriber [Internet]. 2001 Jun 1;24(3):59–61. Available from: https://doi.org/10.18773/austprescr.2001.067 Esim Buyukbayrak E, Kars B, Karsidag AY, Karadeniz BI, Kaymaz O, Gencer S, Pirimoglu ZM, Unal O, and Turan MC. Diagnosis of vulvovaginitis: comparison of clinical and microbiological diagnosis. Arch Gynecol Obstet. 2010 Nov;282(5):515–9. doi: 10.1007/s00404-010-1498-x. Epub 2010 May 12. PMID: 20461391
A cotton swab is utilized to collect a discharge sample for laboratory analysis. The diagnosis of vulvitis can then be established based on the characteristic symptoms observed during the examination or the findings from laboratory tests.6Centers for Disease Control and Prevention. (2017). Self-study module: Vaginitis. Retrieved April 9, 2018, from https://www.std.uw.edu/go/syndrome-based/vaginal-discharge/core-concept/all
Treatment
Treatment of vulvitis depends on symptoms, age, and general health. It also depends on the severity of the vulvitis.7Poordast T, Ghaedian L, Najib FS, Alipour S, Hosseinzadeh M, Vardanjani HM, Salehi A, and Hosseinimehr SJ. Aloe Vera: A new treatment for atrophic vaginitis, a randomized, double-blinded controlled trial. J Ethnopharmacol. 2021 Apr 24;270:113760. doi: 10.1016/j.jep.2020.113760. Epub 2020 Dec 28. PMID: 33383112
- Non-infectious vulvitis can be treated by removing the causative agents.
- Anti-allergic medications can be used for allergic vulvitis.
- Estrogen to overcome hormonal imbalances.
- For infectious vulvitis, antibiotics, antiviral, or anti-fungal drugs are prescribed.
Apart from these, you can opt for the following measures to relieve discomfort:
- Cold compression with the ice pack on a clean cloth can reduce discomfort.
- Wear loose cloth or breathable undergarments to reduce friction in the valvular area.
- Some studies claim that the application of apple cider vinegar can manage vulvitis and cure vaginal candida infection. However, there isn’t yet enough human research to recommend it as a safe and effective treatment for a yeast infection.8Ozen B., Baser M. Vaginal Candidiasis Infection Treated Using Apple Cider Vinegar: A Case Report. Altern Ther Health Med. 2017 Dec;23(7): AT5751. Epub 2017 Nov 7. PMID: 29112940.
Avoid any self-treatment before your doctor prescribes a treatment plan. In some cases, anti-fungal or anti-itch ointments or creams can worsen vulvitis. Creams containing anti-fungal ingredients are what a yeast infection needs for treatment, but they’re not needed to treat a different cause of vulvitis. Some ingredients in creams will irritate your skin even more.
Prevention of Vulvitis
The following actions can be taken to protect yourself from vulvitis:
- General measures such as avoiding soap and bubble baths.
- Toileting and wiping advice: Avoid delaying urination and bowel movements, use the bathroom regularly, and wipe carefully and gently without excessive rubbing.
- For drying, pat it rather than rub the vulva with a towel.
- Soothing creams, such as paraffin and emollients.
Complications of Vulvitis
If left neglected, this condition can become more infected, and symptoms can aggravate. The vulva has a favorable environment for bacterial and fungal growth, which is why early treatment is important.
Further complications include:
- Persistent Pain and Discomfort: This can significantly impact daily activities and quality of life.
- Scarring and Skin Changes: Prolonged vulvitis can lead to scarring or alterations in the appearance of the vulvar skin.
- Painful Sexual Intercourse: This condition can cause dyspareunia, potentially leading to relationship issues.
- Increased Risk of STDs: Chronic vulvitis can raise the likelihood of contracting sexually transmitted diseases (STDs).
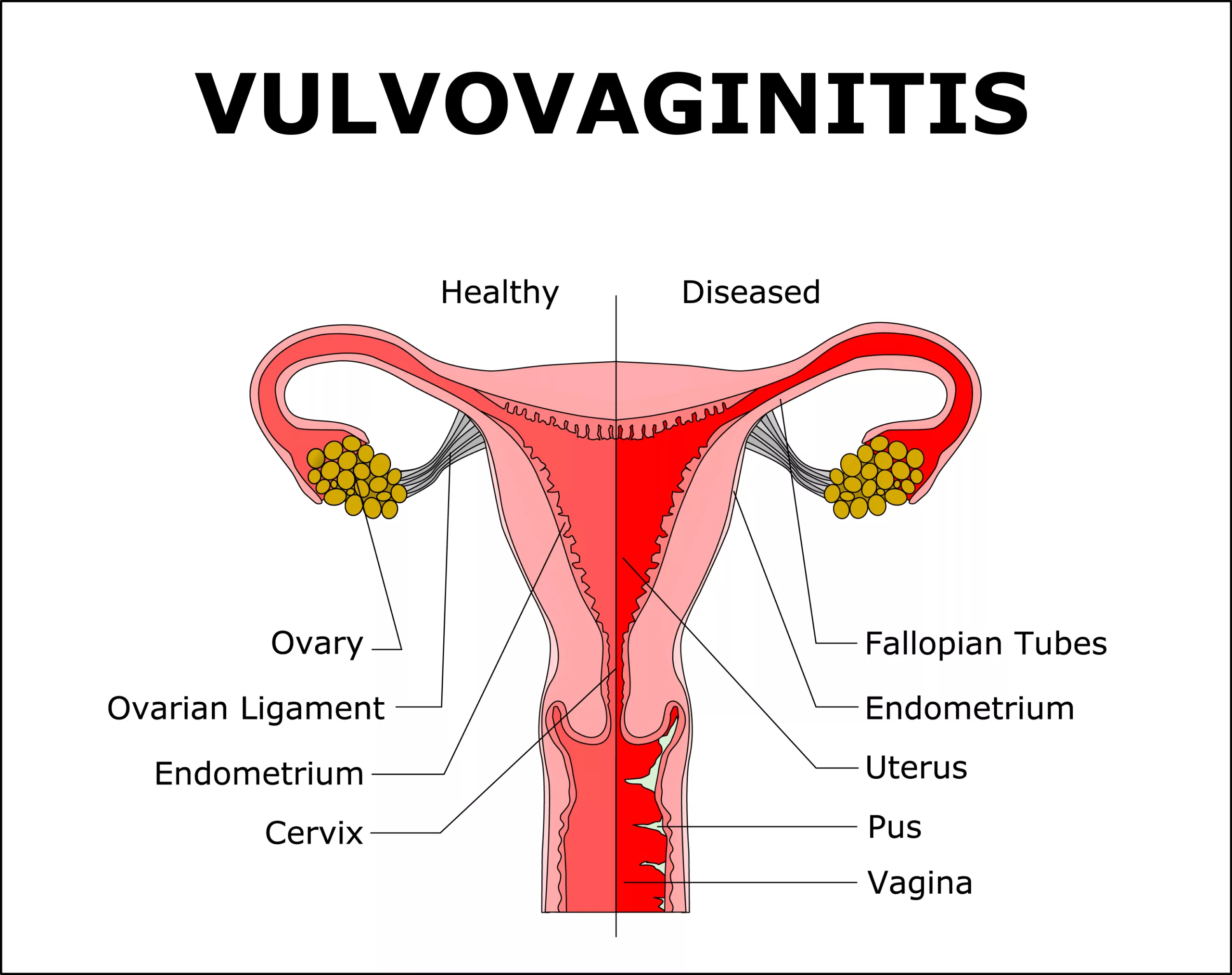
Vaginitis Vs. Vulvitis
Vulvitis and vaginitis are both conditions that present with inflammation of the female genital area, but they affect different parts of the genital area. Vulvitis refers to the inflammation of the vulva, which is the external part of the female genital organ, the vagina. The vulva includes two flaps, major and minor. In contrast, vaginitis refers to the inflammation of the internal surfaces of the female genital organ. These conditions mostly occur simultaneously and are termed as Vulvovaginitis.
Conclusion
It is a discomfort or painful condition caused by unhealthy genital hygiene, tight clothing, or other irritants. A proper diagnosis is necessary for adequate treatment. If this condition is left untreated, it can cause severe discomfort and pain, as well as affect self-esteem and cause infertility in young women.
Refrences
- 1Burcham LR, Burcham ZM, Akbari MS, Metcalf JL, Doran KS. Interrelated Effects of Zinc Deficiency and the Microbiome on Group B Streptococcal Vaginal Colonization. mSphere. 2022 Aug 31;7(4):e0026422. doi: 10.1128/msphere.00264-22. Epub 2022, Aug. 9. PMID: 35943198; PMCID: PMC9429885
- 2Burcham LR, Burcham ZM, Akbari MS, Metcalf JL, Doran KS. Interrelated Effects of Zinc Deficiency and the Microbiome on Group B Streptococcal Vaginal Colonization. mSphere. 2022 Aug 31;7(4):e0026422. doi: 10.1128/msphere.00264-22. Epub 2022, Aug. 9. PMID: 35943198; PMCID: PMC9429885.
- 3Raef HS, Elmariah SB. Vulvar Pruritus: A Review of Clinical Associations, Pathophysiology, and Therapeutic Management. Front Med (Lausanne). 2021 Apr 7;8:649402. doi: 10.3389/fmed.2021.649402. PMID: 33898486; PMCID: PMC8058221.
- 4Nappi RE, Martini E, Cucinella L, Martella S, Tiranini L, Inzoli A, Brambilla E, Bosoni D, Cassani C, and Gardella B. Addressing Vulvovaginal Atrophy (VVA) and Genitourinary Syndrome of Menopause (GSM) for Healthy Aging in Women. Front Endocrinol (Lausanne). 2019 Aug 21;10:561. doi: 10.3389/fendo.2019.00561. PMID: 31496993; PMCID: PMC6712495.
- 5Fischer G. Treatment of vaginitis and vulvitis. Australian Prescriber [Internet]. 2001 Jun 1;24(3):59–61. Available from: https://doi.org/10.18773/austprescr.2001.067 Esim Buyukbayrak E, Kars B, Karsidag AY, Karadeniz BI, Kaymaz O, Gencer S, Pirimoglu ZM, Unal O, and Turan MC. Diagnosis of vulvovaginitis: comparison of clinical and microbiological diagnosis. Arch Gynecol Obstet. 2010 Nov;282(5):515–9. doi: 10.1007/s00404-010-1498-x. Epub 2010 May 12. PMID: 20461391
- 6Centers for Disease Control and Prevention. (2017). Self-study module: Vaginitis. Retrieved April 9, 2018, from https://www.std.uw.edu/go/syndrome-based/vaginal-discharge/core-concept/all
- 7Poordast T, Ghaedian L, Najib FS, Alipour S, Hosseinzadeh M, Vardanjani HM, Salehi A, and Hosseinimehr SJ. Aloe Vera: A new treatment for atrophic vaginitis, a randomized, double-blinded controlled trial. J Ethnopharmacol. 2021 Apr 24;270:113760. doi: 10.1016/j.jep.2020.113760. Epub 2020 Dec 28. PMID: 33383112
- 8Ozen B., Baser M. Vaginal Candidiasis Infection Treated Using Apple Cider Vinegar: A Case Report. Altern Ther Health Med. 2017 Dec;23(7): AT5751. Epub 2017 Nov 7. PMID: 29112940.





