What is Xerophthalmia?
Xerophthalmia is a severe eye condition characterized by a range of ocular signs and symptoms resulting from Vitamin A deficiency. It manifests as dryness of the conjunctiva and cornea (conjunctival and corneal xerosis), Bitot’s spots, and, in advanced cases, softening and ulceration of the cornea (keratomalacia), which can lead to blindness. Other symptoms include night blindness (nyctalopia) and retinal damage. Xerophthalmia is a significant public health issue, particularly in developing countries, where it remains a leading cause of preventable blindness, especially in children. The condition can also contribute to increased morbidity, mortality, and impaired growth in affected children.1Feroze, K. B., & Kaufman, E. J. (2023). Xerophthalmia. In StatPearls. StatPearls Publishing.
Causes of Xerophthalmia
It can occur for two reasons. The first is the most common one: a Vitamin A deficiency. Deficiency develops when one’s diet lacks Vitamin A. Xerophthalmia due to Vitamin A deficiency mostly occurs in children of developing countries where people lack necessities like healthy food.
Besides dietary deficiency of Vitamin A, it can also occur sporadically or when Vitamin A metabolism and storage in the body are affected. Conditions that disturb the metabolism and storage of Vitamin A in the body are excessive alcohol intake, liver disease, pancreatitis, and upper GIT surgery.2Belete, G. T., Fenta, A. L., & Hussen, M. S. (2019). Xerophthalmia and Its Associated Factors among School-Age Children in Amba Giorgis Town, Northwest Ethiopia, 2018. Journal of Ophthalmology, 2019, 5130904. https://doi.org/10.1155/2019/5130904
Epidemiology
Vitamin A deficiency-related xerophthalmia has become a major concern in different countries. According to WHO records, out of 254 million children with Vitamin A deficiency, almost 2.8 children develop Xerophthalmia. Nearly three lacs children every year suffer from blindness due to Xerophthalmia. Due to the increasing number of cases, Xerophthalmia is becoming a serious issue worldwide, especially in countries with fewer resources. The most common cause of blindness in children is Xerophthalmia, which mostly develops in children with anemia due to poor dietary intake.3Dole K, Gilbert C, Deshpande M, Khandekar R. Prevalence and determinants of xerophthalmia in preschool children in urban slums, Pune, India–a preliminary assessment. Ophthalmic Epidemiol. 2009 Jan-Feb;16(1):8-14. 4Pal R, Sagar V. Antecedent risk factors of xerophthalmia among Indian rural preschool children. Eye Contact Lens. 2008 Mar;34(2):106-8.
Risk Factors of Xerophthalmia
Although the main factor that leads to Xerophthalmia is Vitamin A deficiency, the following are some of the potential factors that take part in causing Xerophthalmia in one way or another:
Young Age:
Xerophthalmia develops more at a young age and in children than in adults. Children are prone to certain infections, such as measles or upper respiratory infections, and the chance of having xerophthalmia increases with any underlying infection.
Poverty:
Poverty also plays a part in developing Xerophthalmia in children, as poor people lack healthy food containing Vitamin A. Deficiencies of vitamins and minerals lead to malnutrition and Xerophthalmia.
Underlying Diseases:
People with diseases that disrupt the normal metabolism of Vitamin A, such as pancreatitis, liver cirrhosis, or inflammatory bowel disease, are more prone to develop Xerophthalmia.
Alcoholism:
Alcoholism is a significant factor behind Xerophthalmia in developed countries, as alcohol hinders the normal absorption of Vitamin A and depletes it from your body.5Schaumberg, D. A., O’Connor, J., & Semba, R. D. (1996). Risk factors for xerophthalmia in the Republic of Kiribati. European journal of clinical nutrition, 50(11), 761–764.
Pathophysiology of Xerophthalmia
The functions that Vitamin A performs in your body depict the pathophysiology behind Xerophthalmia. Vitamin A plays an integral role in the normal development of your skin, epithelial surfaces, and retina. Your retina has rods and cone cells responsible for night and day vision, respectively, and Vitamin A deficiency mostly affects the rods. As a result, it deteriorates your night vision, making it difficult to see clearly in dim light. Vitamin A also has a role in maintaining the integrity and normal functioning of your conjunctiva and cornea. Thus, its deficiency causes severe dryness in your cornea and conjunctiva, corneal ulcers, and scarring.
Symptoms of Xerophthalmia
This condition presents with the following specific symptoms:
Night Blindness
The first symptom that you encounter in Vitamin A deficiency is vision loss at night. This is due to the defective functioning of rods, which need Vitamin A for normal function and development. Check your serum retinol levels if you have difficulty seeing in dim light.6Sommer, A., Hussaini, G., Muhilal, Tarwotjo, I., Susanto, D., & Saroso, J. S. (1980). History of night blindness: a simple tool for xerophthalmia screening. The American journal of clinical nutrition, 33(4), 887–891. https://doi.org/10.1093/ajcn/33.4.887
Conjunctival Xerosis
The conjunctiva is a thin mucous membrane in your eyes that contributes to the mucus layer of the tear film. In xerophthalmia, changes in epithelial proteins lead to reduced mucus production. This decrease in mucus output results in fewer tears from the lacrimal glands, causing the conjunctiva to become dull and dry.
Corneal Xerosis
The clear area in front of the eyes that refracts light is the cornea. In Xerophthalmia, the cornea becomes dry and hazy due to decreased tear production. If not treated at the right time, dryness of the cornea can lead to its thinning. Proper Vitamin A supplementation at this stage can reverse the symptoms of Xerophthalmia.
Bitot’s Spots
The formation of Bitot’s spots is a typical sign of Xerophthalmia. These spots have a whitish opaque appearance with a raised margin. Bitot spots typically form in your conjunctiva due to dead keratin cells.7Madan, S., & Beri, S. (2017). Bitot spot: an early marker for avoidable blindness. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 189(40), E1264. https://doi.org/10.1503/cmaj.170792
Keratomalacia
Keratomalacia is the thinning of the cornea due to untreated corneal dryness. As a result of thinning, the cornea develops a cloudy appearance, further deteriorating normal vision. Keratomalacia develops due to a severe Vitamin A deficiency, which can eventually lead to blindness.
Corneal Ulceration & Scar
Extreme dryness of the eyes due to Vitamin A deficiency increases the risk of developing corneal ulcers. These ulcers further increase the risk of developing secondary infections, such as respiratory infections. When these ulcers heal, they leave scarring in the eyes.
Xerophthalmic Fundus
The inside back surface of your eyes is the fundus, which changes due to severe Vitamin A deficiency. During the early stages of Xerophthalmia, your retina undergoes functional changes. With the increasing severity of Vitamin A deficiency, the retina also changes in its structure.8Aygun, B. T., Yildiz, B. K., Koc, D. O., & Yildirim, Y. (2020). Xerophthalmia: Findings from the Eye Lead to Diagnosis of a Fatal Intestinal Disease. Beyoglu Eye Journal, 5(2), 149–152. https://doi.org/10.14744/bej.2020.93063
Diagnosis of Xerophthalmia
Typical manifestations of Xerophthalmia are usually enough to diagnose the condition. Moreover, a detailed history of the symptoms is crucial. If you have symptoms of dry eyes, your physician may ask you for the proper medical history, dietary history, and history of taking alcohol or any other drug.
In addition to evaluating clinical signs and taking history, there are some tests to diagnose Xerophthalmia:
Serum Vitamin A Levels
Checking serum Vitamin A levels in the blood specifies the severity of vitamin A deficiency in your body. It is important to get them checked so that treatment can start as soon as possible. Normal serum Vitamin A levels range from 0.30 to 0.20 mg/L of blood.9Daga, S., Agarwal, K. N., & Bhatt, I. (1969). Serum vitamin A levels in childhood xerophthalmia. The Indian journal of medical research, 57(4), 755–757.
Serum Retinol Levels
Retinol in your body contains Vitamin A. Consequently, checking serum retinol levels helps to determine Vitamin A levels in your body. Laboratory tests to check serum retinol levels in your blood are high-performance liquid chromatography (HPLC) or spectrophotometry.
Dark Adaptometry
Dark adaptometry helps to see how the rods adapt from bright to dim light in patients with night blindness. The patient sits in a dark room with a light source in front of him. The physician changes the light intensity and then measures the rods’ sensitivity to different lights.10Yang, G. Q., Chen, T., Tao, Y., & Zhang, Z. M. (2015). Recent advances in the dark adaptation investigations. International journal of ophthalmology, 8(6), 1245–1252. https://doi.org/10.3980/j.issn.2222-3959.2015.06.31
Night Vision Threshold Tests
This test helps to determine rods’ ability to adapt in a dark room. Dim light spots are used in the dark room, and the patient’s vision is assessed by determining the minimum amount of light he can see.
Ophthalmic Imaging and Tests:
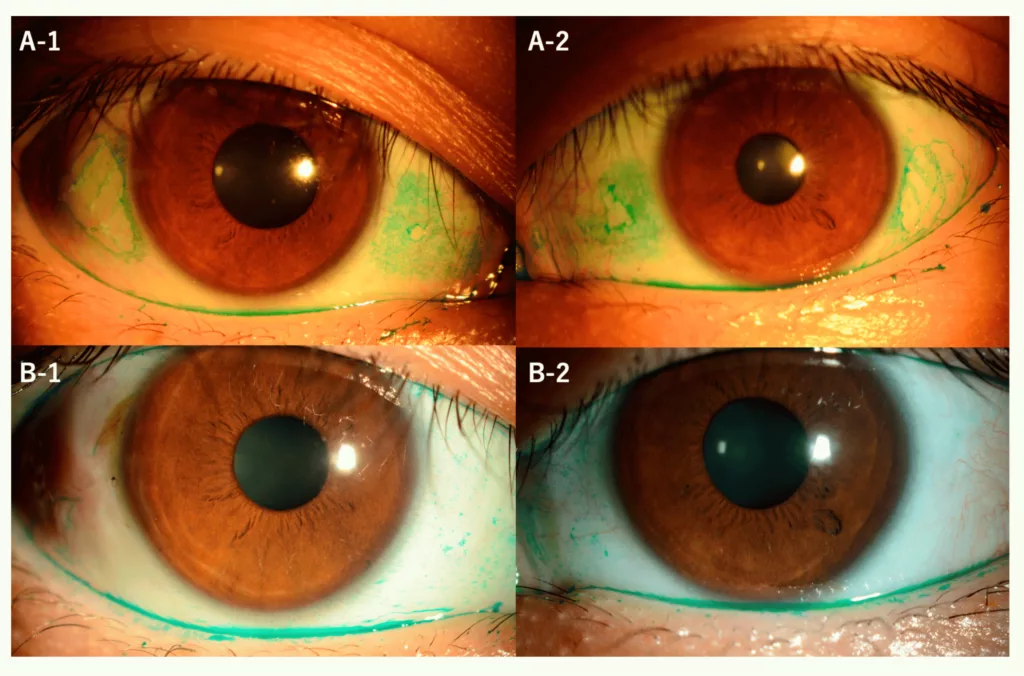
Slit-Lamp Examination:
This test allows the doctor to thoroughly examine the eye’s surface to identify any dryness or damage to the conjunctiva and cornea.
Ocular Surface Staining:
Special dyes such as fluorescein or Lissamine Green can be used to highlight areas of dryness or damage on the eye’s surface, aiding in the diagnosis of xerophthalmia.
Electroretinogram
An electroretinogram detects the response of your retina when light is put into it. An ophthalmologist puts an electrode on your cornea and measures the electrical activity that your retinal neurons produce. ERG also aids in diagnosing retinal disorders and assessing the importance of retinal surgery.

Treatment of Xerophthalmia
Most people with Xerophthalmia recover entirely by taking sufficient amounts of Vitamin A through diet or supplements.
Some strategies to cope with Xerophthalmia are the following:
Oral Vitamin A
Oral vitamin A is an effective way to treat Xerophthalmia. WHO recommends 200,000 IU of oral Vitamin A. The same dose is taken the next day and then some weeks later.
Topical Treatment
In addition to oral Vitamin A, doctors also recommend artificial tears to avoid frequent dryness in your eyes.

Antibiotics
There are cases in which patients get secondary bacterial infections due to severe dryness of the eyes. To avoid this, antibiotics are prescribed.
Treatment of Underlying Condition
When the cause of Xerophthalmia is a defect in the absorption and storage of Vitamin A rather than its deficiency, the treatment of the cause is the main focus to treat Xerophthalmia. Conditions like liver disease or pancreatitis are treated by a gastroenterologist. If the cause is alcoholism, it is crucial to treat it by withdrawal methods or psychological counseling.
Nutritional Support
Nutritional support is the best way to cope with early Vitamin A deficiency. Beef, eggs, carrots, chicken, and milk are rich sources of Vitamin A.11Hatchell, D. L., Faculjak, M., & Kubicek, D. (1984). Treatment of xerophthalmia with retinol, tretinoin, and etretinate. Archives of ophthalmology (Chicago, Ill. : 1960), 102(6), 926–927. https://doi.org/10.1001/archopht.1984.01040030746036

Surgical Intervention:
In severe cases with corneal damage, surgical procedures such as corneal transplantation or amniotic membrane transplantation may be necessary to restore vision and eye health.
Difference between Xerostomia & Xerophthalmia
Xerostomia and Xerophthalmia both refer to dryness but in different parts of the body.
Xerostomia is dryness in the mouth, which occurs due to any salivary gland defect or decreased saliva production. It occurs in patients undergoing radiation therapy of the head and neck or taking certain medications, for instance, anticholinergic, antidepressants, or diuretics. Xerostomia is also a part of Sjogren syndrome along with Xerophthalmia. In xerostomia, you experience oral dryness, taste changes, loss of appetite, and fissures in your mouth or lips. Your physician advises you to drink plenty of water, avoid caffeine and alcohol, and use sialogogue drugs like pilocarpine.
On the other hand, Xerophthalmia develops when you have a Vitamin A deficiency. This leads to dryness in your eyes, which may cause scarring and ulcers in your corneas. Physicians prescribe Vitamin A supplements, artificial tears, and antibiotics to treat Xerophthalmia.
Differential Diagnoses of Xerophthalmia
Some of the differentials of Xerophthalmia show almost the same symptoms of dryness and irritation in the eye and vision loss in uncured cases. These are:
- Hypothyroidism
- Parasitic eye disease
- Trachoma
Prevention & Prognosis of Xerophthalmia
The best approach to treating Xerophthalmia is to eat a proper diet and food that contains Vitamin A. You must consume leafy green vegetables, eggs, carrots, yams, citrus, and beef to overcome vitamin A deficiency.12The prevention of xerophthalmia. (1973). WHO Chronicle, 27(1), 28–30.
Eating vitamin A-containing food and supplements can help with the early stages of Vitamin A deficiency. Properly treating the cause in the early stages can prevent blindness caused by Xerophthalmia, hence the good prognosis.
However, people who acquire corneal ulcers due to severe Xerophthalmia need surgery to treat it, but it still doesn’t promise satisfactory results.13McLaughlin, S., Welch, J., MacDonald, E., Mantry, S., & Ramaesh, K. (2014). Xerophthalmia–a potential epidemic on our doorstep? Eye (London, England), 28(5), 621–623. https://doi.org/10.1038/eye.2014.17
Conclusion
In conclusion, Vitamin A deficiency or any defect with its absorption in your body causes Xerophthalmia. It causes dryness of your eyes, formation of bitot spots, and night blindness, and if it is not treated at the right time, it leads to scarring, thinning of the cornea, and permanent blindness. Although clinical signs of Xerophthalmia are enough to diagnose it, some tests such as dark adaptometry, serum Vitamin A and retinol levels, and impression cytology further confirm the diagnosis. A diet rich in eggs, vegetables, carrots, and beef is appropriate to treat Vitamin A deficiency. You can also go for oral Vitamin A and Vitamin A supplements. Xerophthalmia should be taken seriously as its untreated cases lead to permanent blindness, which isn’t possible to cure completely.
Refrences
- 1Feroze, K. B., & Kaufman, E. J. (2023). Xerophthalmia. In StatPearls. StatPearls Publishing.
- 2Belete, G. T., Fenta, A. L., & Hussen, M. S. (2019). Xerophthalmia and Its Associated Factors among School-Age Children in Amba Giorgis Town, Northwest Ethiopia, 2018. Journal of Ophthalmology, 2019, 5130904. https://doi.org/10.1155/2019/5130904
- 3Dole K, Gilbert C, Deshpande M, Khandekar R. Prevalence and determinants of xerophthalmia in preschool children in urban slums, Pune, India–a preliminary assessment. Ophthalmic Epidemiol. 2009 Jan-Feb;16(1):8-14.
- 4Pal R, Sagar V. Antecedent risk factors of xerophthalmia among Indian rural preschool children. Eye Contact Lens. 2008 Mar;34(2):106-8.
- 5Schaumberg, D. A., O’Connor, J., & Semba, R. D. (1996). Risk factors for xerophthalmia in the Republic of Kiribati. European journal of clinical nutrition, 50(11), 761–764.
- 6Sommer, A., Hussaini, G., Muhilal, Tarwotjo, I., Susanto, D., & Saroso, J. S. (1980). History of night blindness: a simple tool for xerophthalmia screening. The American journal of clinical nutrition, 33(4), 887–891. https://doi.org/10.1093/ajcn/33.4.887
- 7Madan, S., & Beri, S. (2017). Bitot spot: an early marker for avoidable blindness. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 189(40), E1264. https://doi.org/10.1503/cmaj.170792
- 8Aygun, B. T., Yildiz, B. K., Koc, D. O., & Yildirim, Y. (2020). Xerophthalmia: Findings from the Eye Lead to Diagnosis of a Fatal Intestinal Disease. Beyoglu Eye Journal, 5(2), 149–152. https://doi.org/10.14744/bej.2020.93063
- 9Daga, S., Agarwal, K. N., & Bhatt, I. (1969). Serum vitamin A levels in childhood xerophthalmia. The Indian journal of medical research, 57(4), 755–757.
- 10Yang, G. Q., Chen, T., Tao, Y., & Zhang, Z. M. (2015). Recent advances in the dark adaptation investigations. International journal of ophthalmology, 8(6), 1245–1252. https://doi.org/10.3980/j.issn.2222-3959.2015.06.31
- 11Hatchell, D. L., Faculjak, M., & Kubicek, D. (1984). Treatment of xerophthalmia with retinol, tretinoin, and etretinate. Archives of ophthalmology (Chicago, Ill. : 1960), 102(6), 926–927. https://doi.org/10.1001/archopht.1984.01040030746036
- 12The prevention of xerophthalmia. (1973). WHO Chronicle, 27(1), 28–30.
- 13McLaughlin, S., Welch, J., MacDonald, E., Mantry, S., & Ramaesh, K. (2014). Xerophthalmia–a potential epidemic on our doorstep? Eye (London, England), 28(5), 621–623. https://doi.org/10.1038/eye.2014.17