What is Acute Hepatic Porohria?
Acute hepatic porphyria (AHP) is a group of metabolic disorders characterized by the buildup of specific molecules known as porphyrins in the body. This buildup primarily impacts the liver, but it can also affect the nervous system and, eventually, the entire body. Common symptoms include abdominal pain, nausea, vomiting, diarrhea, muscle pain, back pain, chest pain, skin blisters, and anxiety. It results from the deficiency of any of the eight enzymes involved in heme biosynthesis in your body, which causes the accumulation of molecules called Porphyrins. Heme is a crucial component in our body’s metabolism, playing a central role in various processes, including oxygen transport.
Acute hepatic porphyria is a genetic disorder with autosomal dominant, recessive, or X-linked inheritance patterns. According to research, one in twenty-five thousand individuals in The United States is affected by acute hepatic porphyria.1Ramanujam, V. S., & Anderson, K. E. (2015). Porphyria Diagnostics-Part 1: A Brief Overview of the Porphyrias. Current protocols in human genetics, 86, 17.20.1–17.20.26. https://doi.org/10.1002/0471142905.hg1720s86
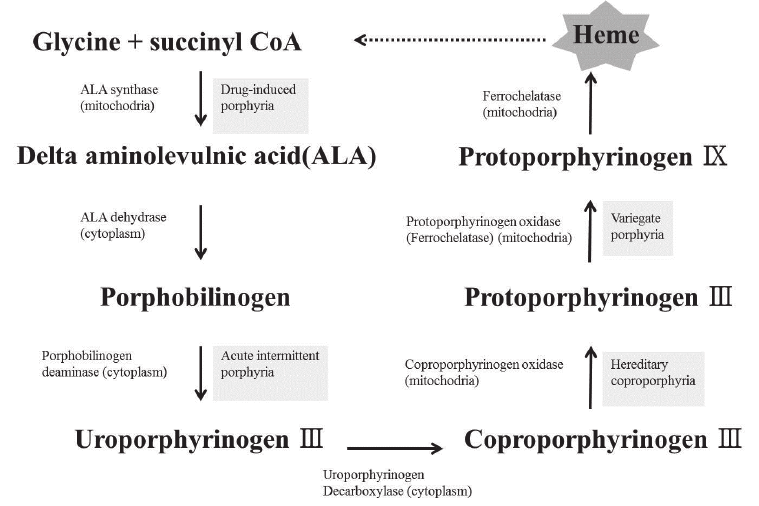
Pathophysiology Of Acute Hepatic Porphyria:
Acute hepatic porphyria is caused by mutations in genes responsible for the enzymes involved in heme biosynthesis. One common mutation occurs in the HMBS (Hydroxymethylbilane Synthase) gene located on chromosome 11q24.1-q24.2.2Bonkovsky HL, Dixon N, Rudnick S. Pathogenesis and clinical features of the acute hepatic porphyrias (AHPs). Mol Genet Metab. 2019 Nov;128(3):213-218. Doi: 10.1016/j.ymgme.2019.03.002. Epub 2019 Mar 6. PMID: 30987916; PMCID: PMC6754303.Heme is a vital component of hemoglobin and other proteins involved in oxygen transport and energy production. This mutation causes a deficiency of any of the eight enzymes in your body involved in heme metabolism, leading to the accumulation of heme intermediates, such as Porphobilinogen and Aminolevulinic acid. They accumulate in your liver; besides this, they circulate throughout your body, and ultimately they produce symptoms of Porphyria.
Symptoms of Acute Hepatic Porphyria:
Symptoms Of Acute Hepatic Porphyria start with abdominal pain; however, generalized body aches, back pain, muscle pain, and fatigue also occur later.
Gastrointestinal Symptoms
Gastrointestinal problems occur in acute hepatic porphyria that include:
- Diarrhea
- Constipation
- Indigestion
- Vomiting

Neurological Symptoms
Neurological symptoms of acute hepatic porphyria include neuropathy symptoms that include:
- Tingling
- Numbness
- Weakness
- Sensory loss
- Fatigue
Moreover, anxiety, depression, seizures, hallucinations, and delirium also occur in acute hepatic porphyria.
Dermatological Symptoms
Skin reactions like rashes, blisters, and pigmentation occur in acute hepatic porphyria, and scarring can also occur.
Urine Color Changes
Acute Hepatic Porphyria changes the color of your urine from yellow to reddish-purple due to the accumulation of molecules called porphyrin products in urine. Basically, the word Porphyria originates from the word Porphura, which means purple. However, It’s essential to note that this symptom is not always present in all cases of AHP. The color change in urine occurs when porphyrins are excreted in the urine and can be influenced by factors such as the type of AHP, the severity of the condition, and individual variations.
Types Of Acute Hepatic Porphyria:
Acute hepatic porphyria has four types that include:
Acute Intermittent Porphyria
It occurs due to a mutation in the HMBS (HydroxyMethylbilane Synthase) gene that results in the deficiency of the HydroxymethylBilane synthase enzyme. This causes an accumulation of Porphobilinogen and acute intermittent porphyria. It has autosomal dominant patterns of inheritance, meaning that a single copy of the mutated gene from one parent is sufficient to cause the condition. In addition to this, it is the most common type of acute hepatic porphyria.
Variegate Porphyria
Variegate Porphyria (VP) is a type of porphyria resulting from a PPOX gene mutation. This genetic mutation leads to a deficiency of the Protoporphyrin oxidase enzyme. Like Acute Intermittent Porphyria (AIP), Variegate Porphyria follows an autosomal dominant inheritance pattern.
VP is relatively rare, and its severity and symptom presentation can vary among affected individuals.
Hereditary Coproporphyria
Hereditary Coproporphyria (HCP) is a rare type of porphyria resulting from a mutation in the CPOX gene, leading to a deficiency of the Coproporphyrinogen oxidase enzyme.3National Institutes of Health. (n.d.). Hereditary Coproporphyria. Retrieved from https://rarediseases.info.nih.gov/diseases/6619/hereditary-coproporphyria This disrupts heme metabolism and causes an accumulation of Coproporphyrinogen, leading to symptoms like abdominal pain, skin photosensitivity, and neurological issues. Proper management, including trigger avoidance and supportive care, is essential for individuals with HCP. Genetic counseling is important for understanding inheritance patterns, and collaborative efforts between patients and healthcare providers are crucial for optimal management of this condition.
ALAD (Delta Aminolevulinic Acid Dehydratase) Deficiency Porphyria
ALAD deficiency Porphyria is a rare inherited genetic disorder characterized by the deficiency of an enzyme called Delta Aminolevulinic acid dehydratase (ALAD). This condition follows an autosomal recessive pattern of inheritance, which means that both copies of the ALAD gene must be defective for the disorder to manifest. It results from a mutation in the ALAD gene on your chromosome.
Prevalence Of Acute Hepatic Porphyria:
The estimated prevalence of acute hepatic porphyrias is one per five years individuals. However, the most common one is porphyria cutanea tarda, which has prominent clinical symptoms, and its estimated prevalence is one per ten thousand individuals. Acute intermittent porphyria has a prevalence of one in two thousand individuals. Moreover, acute intermittent porphyria is also common in certain ethnic groups like Spain and Argentina.4Cerbino, G. N., Gerez, E. N., Varela, L. S., Melito, V. A., Parera, V. E., Batlle, A., & Rossetti, M. V. (2015). Acute intermittent porphyria in Argentina: an update. BioMed research international, 2015, 946387. https://doi.org/10.1155/2015/946387
Triggers & Precipitating Factors:
The major risk factors for acute hepatic porphyria include infections, low-calorie intake, fasting, alcohol consumption, certain drugs, and reproductive changes. Additionally, females are at a higher risk of developing acute hepatic porphyria compared to males.
Low-calorie intake and fasting can lead to a shortage of nutrients needed for heme synthesis, potentially exacerbating porphyria symptoms. Alcohol consumption induces enzymes that interfere with heme synthesis, making it a significant trigger for acute attacks.
Drugs You Should Avoid In Acute Hepatic Porphyria:
Certain medications, such as barbiturates, antiepileptic drugs, and sulfonamides, can worsen porphyria symptoms, increasing the risk of acute episodes. According to the Norwegian Porphyria Centre and Europe Porphyria Network, clinicians should avoid prescribing drugs like Ketamine, Thiopental, Rifampicin, Spironolactone, Carbamazepine, Phenytoin, Risperidone, and Phenobarbital to the porphyria patients.5 Roveri G, Nascimbeni F, Rocchi E, Ventura P. Drugs and acute porphyrias: reasons for a hazardous relationship. Postgrad Med. 2014 Nov;126(7):108-20. doi: 10.3810/pgm.2014.11.2839. PMID: 25387219.
Acute Hepatic Porphyria vs. Acute Intermittent Porphyria:
Acute Intermittent Porphyria is a subtype of acute hepatic porphyria that results from a partial deficiency of the HydroxymethylBilane Synthase enzyme. As a result of this, Aminolevulinic acid and Porphobilinogen accumulate. Its symptoms include gastrointestinal problems like nausea, vomiting, diarrhea, rapid heart rate, increased blood pressure, behavioral changes, and seizures. Treatment of acute intermittent porphyria includes avoiding triggering factors and Heme injections. Besides this, hospitalization and treatment of gastrointestinal and neurological symptoms should be
Potential Complications from Acute Hepatic Porphyria
During an acute attack, symptoms affecting the central nervous system, like anxiety, hallucinations, and seizures, are typically temporary. Conversely, symptoms linked to the peripheral nervous system, such as muscle weakness and paralysis, can occur more frequently, with the potential for enduring harm during severe episodes. Moreover, the accumulation of porphyrin precursors has the capacity to gradually harm specific organs, potentially giving rise to conditions such as6Gonzalez-Mosquera LF, Sonthalia S. Acute Intermittent Porphyria. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547665/
- Chronic hypertension
- Chronic liver disease
- Chronic kidney disease
- Hepatocellular cancer7Stewart MF. Review of hepatocellular cancer, hypertension, and renal impairment as late complications of acute porphyria and recommendations for patient follow-up. J Clin Pathol. 2012 Nov;65(11):976-80.
- Depression and anxiety.
Diagnosis of Acute Hepatic Porphyria:
Symptoms of acute hepatic porphyria are diverse; as a result, acute hepatic porphyria is not diagnosed easily. However, severe chronic gastrointestinal pain and porphyria symptoms in your body lead to the diagnosis of acute hepatic porphyria.
Acute Hepatic Porphyria (AHP) is diagnosed8Anderson KE. Acute hepatic porphyrias: Current diagnosis & management. Mol Genet Metab. 2019 Nov;128(3):219-227. doi 10.1016/j.ymgme.2019.07.002. Epub 2019 Jul 5. PMID: 31311713; PMCID: PMC6911835. by measuring the levels of Aminolevulinic acid (ALA) and Porphobilinogen (PBG) molecules in the blood, urine, or sometimes in the stool.
The primary screening test for diagnosing acute porphyria is the measurement of urinary porphobilinogen (PBG). During acute porphyria attacks, PBG levels are significantly elevated in all affected patients, making this test highly sensitive and specific for detecting acute porphyria. It helps distinguish acute porphyria from other medical conditions that may have similar symptoms but do not exhibit marked elevation of PBG.
However, one rare exception is ALAD-Deficient Porphyria (ADP), where urinary PBG levels may not be notably increased during an attack. Instead, another compound called aminolevulinic acid (ALA) is elevated in ADP. Nevertheless, ADP is an extremely rare condition and is typically not the first consideration during porphyria evaluations due to its uncommon occurrence.
Genetic Testing
Genetic testing9Balwani M, Wang B, Anderson KE, Bloomer JR, Bissell DM, Bonkovsky HL, Phillips JD, Desnick RJ; Porphyrias Consortium of the Rare Diseases Clinical Research Network. Acute hepatic porphyrias: Recommendations for evaluation and long-term management. Hepatology. 2017 Oct;66(4):1314-1322. doi: 10.1002/hep.29313. Epub 2017 Sep 4. PMID: 28605040; PMCID: PMC5605422. is also an essential component of diagnosing porphyria. It involves analyzing a sample of DNA from saliva, blood, or other body fluids to identify specific genetic mutations associated with different types of porphyria. Genetic testing helps determine the condition’s underlying cause and confirms the type of porphyria the individual has.
Treatment Of Acute Hepatic Porphyria:
The first remedy for treating acute hepatic porphyria is avoiding triggering factors like drugs, alcohol, infection, smoking, alcohol, fasting, and sun exposure. Moreover, treating infections is the main step in preventing attacks of acute hepatic porphyria. Besides this, avoid emotional stress and infection triggers. Some of the treatment options are:
IV Hemin:
Medical treatment of acute hepatic porphyria focuses on treating symptoms and preventing complications. It consists of an IV injection of Hemin (Panhematin) that limits the production of Porphyrins.10Pischik E, Kauppinen R. An update of clinical management of acute intermittent porphyria. Appl Clin Genet. 2015;8:201.
Givosiran:
In 2019, the U.S. Food and Drug Administration approved a medication named Givosiran, designed to address the needs of adults grappling with Acute Hepatic Porphyria (AHP). Administered via subcutaneous injection once per month, Givosiran offers a therapeutic solution. Notably, clinical trials revealed that individuals undergoing Givosiran treatment experienced a reduction in the frequency of acute AHP attacks, in contrast to those who received a placebo—a treatment void of active components.11Kuter, D. J., Bonkovsky, H. L., Monroy, S., Sweetser, M. T., Thapar, M., & ENVISION Investigators. (2023). Efficacy and safety of givosiran for acute hepatic porphyria: Final results of the randomized phase III ENVISION trial. Journal of Hepatology, Open Access, Published: July 18, 2023. https://doi.org/10.1016/j.jhep.2023.06.013 It is imperative for patients taking Givosiran to maintain regular liver and kidney assessments overseen by their healthcare providers.
For individuals suffering from recurrent severe AHP attacks, with limited response to IV hemin or Givosiran, or a notably compromised quality of life, the possibility of liver transplantation arises as a last-resort option.
Pain Management:
Effective pain relief measures, including potent pain relievers like opioids, might be necessary to alleviate the intensity of discomfort during an acute episode.
Phenothiazines Utilization:
In cases of pronounced nausea and vomiting, phenothiazines can be employed to manage these symptoms and provide relief effectively.
Intravenous (IV) Fluids and Nutritional Support:
Acute attacks can trigger symptoms such as abdominal pain, nausea, vomiting, diarrhea, and constipation. These symptoms can lead to caloric and hydration deficits. Additionally, AHP might contribute to sodium and magnesium deficiencies. To address these issues, IV fluids containing carbohydrates and electrolytes can be administered to restore the body’s balance.
Seizure Medications:
During an attack, a portion of individuals, up to 20%, might require treatment for seizures. Appropriate seizure medications can be employed to manage this aspect of the condition effectively.
Liver Transplantation:
People who experience frequent, life-threatening attacks that don’t respond to other treatment options may be eligible for a liver transplant. This can cure them.
Conclusion:
Acute Hepatic Porphyria stands as a complex and multifaceted disorder characterized by its episodic and often debilitating nature. Its intricate interplay of genetic factors and enzymatic deficiencies underscores the importance of a comprehensive and multidisciplinary approach to both management and research. While recent advancements in understanding the underlying mechanisms and the emergence of targeted therapies have offered new hope, challenges persist in effectively addressing acute attacks, preventing complications, and enhancing the quality of life for those affected.
Refrences
- 1Ramanujam, V. S., & Anderson, K. E. (2015). Porphyria Diagnostics-Part 1: A Brief Overview of the Porphyrias. Current protocols in human genetics, 86, 17.20.1–17.20.26. https://doi.org/10.1002/0471142905.hg1720s86
- 2Bonkovsky HL, Dixon N, Rudnick S. Pathogenesis and clinical features of the acute hepatic porphyrias (AHPs). Mol Genet Metab. 2019 Nov;128(3):213-218. Doi: 10.1016/j.ymgme.2019.03.002. Epub 2019 Mar 6. PMID: 30987916; PMCID: PMC6754303.
- 3National Institutes of Health. (n.d.). Hereditary Coproporphyria. Retrieved from https://rarediseases.info.nih.gov/diseases/6619/hereditary-coproporphyria
- 4Cerbino, G. N., Gerez, E. N., Varela, L. S., Melito, V. A., Parera, V. E., Batlle, A., & Rossetti, M. V. (2015). Acute intermittent porphyria in Argentina: an update. BioMed research international, 2015, 946387. https://doi.org/10.1155/2015/946387
- 5Roveri G, Nascimbeni F, Rocchi E, Ventura P. Drugs and acute porphyrias: reasons for a hazardous relationship. Postgrad Med. 2014 Nov;126(7):108-20. doi: 10.3810/pgm.2014.11.2839. PMID: 25387219.
- 6Gonzalez-Mosquera LF, Sonthalia S. Acute Intermittent Porphyria. [Updated 2023 May 1]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK547665/
- 7Stewart MF. Review of hepatocellular cancer, hypertension, and renal impairment as late complications of acute porphyria and recommendations for patient follow-up. J Clin Pathol. 2012 Nov;65(11):976-80.
- 8Anderson KE. Acute hepatic porphyrias: Current diagnosis & management. Mol Genet Metab. 2019 Nov;128(3):219-227. doi 10.1016/j.ymgme.2019.07.002. Epub 2019 Jul 5. PMID: 31311713; PMCID: PMC6911835.
- 9Balwani M, Wang B, Anderson KE, Bloomer JR, Bissell DM, Bonkovsky HL, Phillips JD, Desnick RJ; Porphyrias Consortium of the Rare Diseases Clinical Research Network. Acute hepatic porphyrias: Recommendations for evaluation and long-term management. Hepatology. 2017 Oct;66(4):1314-1322. doi: 10.1002/hep.29313. Epub 2017 Sep 4. PMID: 28605040; PMCID: PMC5605422.
- 10Pischik E, Kauppinen R. An update of clinical management of acute intermittent porphyria. Appl Clin Genet. 2015;8:201.
- 11Kuter, D. J., Bonkovsky, H. L., Monroy, S., Sweetser, M. T., Thapar, M., & ENVISION Investigators. (2023). Efficacy and safety of givosiran for acute hepatic porphyria: Final results of the randomized phase III ENVISION trial. Journal of Hepatology, Open Access, Published: July 18, 2023. https://doi.org/10.1016/j.jhep.2023.06.013