Bardet-Biedl Syndrome (BBS) is a rare genetic disorder that affects multiple body systems, usually starting in early childhood. It is inherited in an autosomal recessive pattern, leading to physical and developmental symptoms. Common features include progressive vision loss, obesity, intellectual disability, extra fingers or toes (polydactyly), and abnormalities in sexual development.1Forsythe E, Beales PL. Bardet-Biedl Syndrome. In: GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993–2024.
What is Bardet-Biedl Syndrome?
BBS is classified as a ciliopathy—meaning it results from defects in the structure or function of primary cilia, which are hair-like extensions on the surface of cells responsible for critical signaling pathways. When these cilia do not function properly, it can disrupt the development and function of several organs and systems, including the nervous, renal, skeletal, and reproductive systems. Early diagnosis plays a key role in managing complications and preventing long-term damage.2Nachury MV, Mick DU. Establishing and regulating the composition of cilia for signal transduction. Nat Rev Mol Cell Biol. 2019;20(7):389–405.
Georges Bardet first identified this syndrome in 1920, followed by Arthur Biedl in 1922. It was then recognized as a distinct genetic disorder. This rare disorder affects 1 in 100,000 to 1 in 160,000 people worldwide. BBS affects people more frequently in communities that practice consanguineous marriages, like Newfoundland, Canada, and the Middle East.3Green JS, Parfrey PS, Harnett JD, et al. The cardinal manifestations of Bardet-Biedl syndrome, a form of Laurence-Moon-Biedl syndrome. N Engl J Med. 1989;321(15):1002–1009.
Bardet-Biedl Syndrome Causes
Bardet-Biedl Syndrome arises from genetic changes that affect the structure and function of cellular cilia, particularly the basal body, a key component involved in cilia assembly and signaling. Research has identified mutations in at least 24 different genes (BBS1 through BBS24) that disrupt normal ciliary function, ultimately contributing to the development of BBS.4Khan SA, Muhammad N, Khan MA, Kamal A, Rehman ZU, Khan S. Genetics of human Bardet-Biedl syndrome, an updates. Clin Genet. 2016;90(1):3–15.
These BBS genes play important roles in a process known as intraflagellar transport (IFT)—a bidirectional system that allows molecular cargo to move along the ciliary axoneme. This system is essential for proper cilia function and signaling. The BBS1, BBS2, BBS4, BBS6, BBS7, BBS8, BBS9, BBS10, and BBS12 genes represent the primary genetic mutations found in affected patients.5Huber C, Delezoide AL, Guimiot F, et al. A large-scale mutation search in Bardet-Biedl syndrome loci. J Med Genet. 2010;47(11):705–712.
| Gene | Function | Mutation Frequency |
| BBS1 | Cilia formation & signaling | High |
| BBS2 | Ciliary transport | Moderate |
| BBS10 | Protein folding | Moderate |
Inheritance Pattern of BBS
The inheritance pattern of Bardet-Biedl Syndrome follows an autosomal recessive transmission. This means a child must inherit two mutated copies of a BBS gene—one from each parent—to develop the syndrome. Individuals who inherit only one mutated copy are considered carriers. They typically show no symptoms but can pass the mutation on to their offspring.
People who have Bardet-Biedl Syndrome should seek genetic counseling to understand their family risks. In this way, families gain knowledge about potential risks along with the implications for their offspring.
Bardet-Biedl Syndrome Symptoms & Features
There is no specific age for signs and symptoms to appear. They can appear at any age. Similarly, types and intensity also vary in different patients.
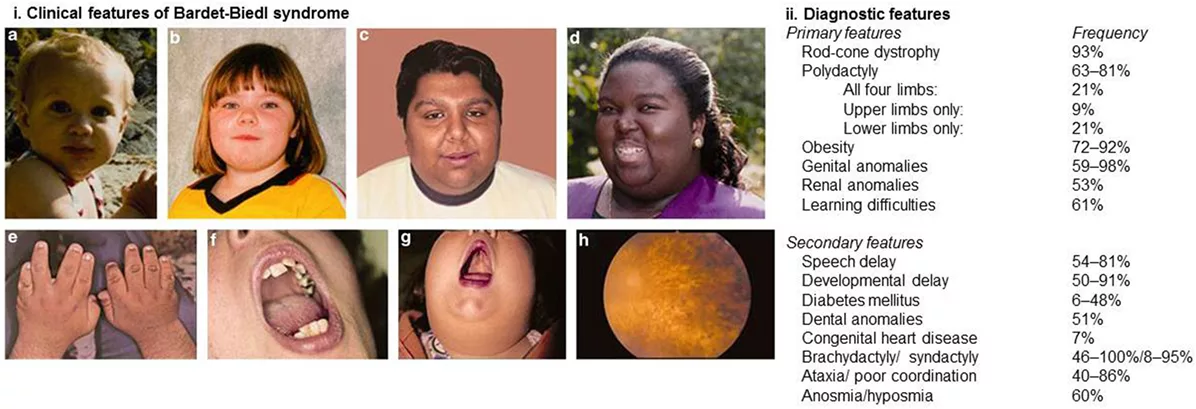
Image credit: Adapted from Forsythe E, Beales PL. 2018. Managing Bardet–Biedl Syndrome—Now and in the Future. Front Pediatr. 6:23. © Authors, under CC BY 4.0.
Major Clinical Features:
1. Progressive Vision Loss (Cone-Rod Dystrophy)
The first noticeable signs of BBS appear as visual impairment, with or without night blindness. As the condition progresses, patients experience reduced side vision, color blindness, and reduced vision clarity. BBS diagnosis becomes possible early if you notice these problems before your kid reaches the tenth birthday, consult health professionals soon.6Iannaccone A, Mykytyn K, Persico AM, et al. Clinical and functional aspects of Bardet-Biedl syndrome: insights from a multidisciplinary perspective. Retina. 2009;29(4):453–463.
An abnormal electroretinography test (ERG ) often reveals impaired retinal function in affected individuals. Eye specialists have observed retinal disorders (strabismus, astigmatism, cataracts) in many patients.
2. Obesity
BBS children have a normal birth weight when born, yet they start developing central obesity during their early infancy. Research indicates that the average Body Mass Index (BMI) reaches 35.7, which marks severe obesity in early childhood.7Feuillan PP, Ng D, Han JC, et al. Patients with Bardet-Biedl syndrome have hyperleptinemia suggestive of leptin resistance. J Clin Endocrinol Metab. 2011;96(3):E528–E535
3. Extra Fingers or Toes (Polydactyly)
Polydactyly means additional fingers or toes. These extra digits are usually made up of soft tissues, but sometimes they also contain bones and joints. The more common presentation is an extra little finger on the ulnar side (postaxial) or a thumb on the fibular side (preaxial), and rarely a finger in the middle (central).8Katsanis N. The oligogenic properties of Bardet-Biedl syndrome. Hum Mol Genet. 2004;13 Spec No 1:R65–R71.
4. Cognitive & Behavioral Challenges
BBS patients have reduced cognitive abilities, resulting in multiple kinds of mental disabilities. The condition affects only a limited number of children. Individuals with BBS commonly experience problems with critical thinking and word communication, as well as attention deficiencies. Autistic features have also been documented.9Beales PL, Elcioglu N, Woolf AS, Parker D, Flinter FA. New criteria for improved diagnosis of Bardet-Biedl syndrome: results of a population survey. J Med Genet. 1999;36(6):437–446.
5. Underdeveloped Reproductive Organs & Infertility
BBS leads to delayed puberty in its patients. The typical symptoms in males consist of:
- Tiny genitals
- Small testes that do not descend properly
- Low testosterone levels
The abnormalities seen in females are:
- Hypoplastic or duplex uterus
- Hypoplastic fallopian tubes and/or ovaries
- Partial or complete vaginal atresia
- Absent vaginal orifice
- Persistent urogenital sinus
- Vesico-vaginal fistula.
The majority of these cases lead to infertility, but a few manage to conceive.10Dattani MT, Guffanti A, Taylor D, et al. Endocrine abnormalities in Bardet-Biedl syndrome. Clin Endocrinol (Oxf). 2013;78(3):364–370.
6. Kidney Involvement
BBS also leads to kidney-related complications, including cysts or ectopic kidneys. Advanced stages of chronic kidney disease (CKD) can also occur in BBS. Medical professionals diagnose most cases within the first year of life or before children reach five.
People with advanced kidney disease at any age require either dialysis or kidney transplantation. Older adults with hypertension, along with type 2 diabetes, develop more rapid kidney damage.11Imhoff O, Marion V, Stoetzel C, et al. Bardet-Biedl syndrome: a study of the renal and cardiovascular phenotypes in a French cohort. Clin J Am Soc Nephrol. 2011;6(1):22–29.
Minor Clinical Features:
- Neurodevelopmental Delays: A delay in speech, motor skills, and overall physical growth has been reported in BBS patients. Doctors may observe ataxia, poor coordination, and stiff muscles. However, most children eventually become able to walk and talk.
- Speech and Language Issues: Children with speech delay tend to speak through their noses, their voices sound breathy, and their words become difficult to understand. The conditions develop from hearing issues, oral structure problems, and neurological aspects.
- Behavioral and Emotional Concerns: Changes in behavior and emotional difficulties are observed in these patients, such as anxiety and mood disorders, and obsessive-compulsive traits.
- Facial and Cranial Differences: People with BBS present with a flat face structure, a deep nasal indentation, and a thin chin. Some individuals may exhibit hypertelorism, characterized by widely spaced eyes. These signs do not appear in every case.
- Reduced Sense of Smell (Anosmia/Hyposmia): Hypo or anosmia may or may not be present. The olfactory system shows changes in brain images in most cases.
- Dental and Oral Abnormalities: The common dental defects include tooth absence or small tooth size, teeth crowding, undeveloped roots, enamel problems, and a high-arched palate. Poor dental care, together with existing medical conditions, tends to produce more severe complications.
- Heart and Thoraco-abdominal Defect: Rare congenital heart defects and situs inversus (abnormal organ positioning) have been reported, though infrequently.
- Gastrointestinal and Liver Issues: Diseases like Hirschsprung disease, together with obstructions, affect the digestive tract. Obesity leads to higher risks of developing inflammatory bowel disease, together with specific liver conditions such as non-alcoholic fatty liver disease (NAFLD).12Tobin JL, Beales PL. Bardet-Biedl syndrome: beyond the cilium. Pediatr Nephrol. 2007;22(7):926–936.
- Endocrine and Metabolic Disorders: These patients have obesity as a major feature. The complications of obesity lead to high triglyceride levels, insulin resistance, and type 2 diabetes. Women who have this condition might also experience polycystic ovarian syndrome (PCOS).
Rare Features:
- Skin Conditions: BBS patients can rarely experience some skin problems, such as keratosis pilaris alongside seborrheic dermatitis and obesity-related skin issues such as acanthosis nigricans and stretch marks.
- Hearing Loss: Hearing loss, in adults, is caused by sensorineural factors. Whereas children usually experience conductive hearing problems because of frequent ear infections.
- Skeletal Anomalies: The condition may result in increased scoliosis and unequal leg size with flexible joints and foot issues.
Differential Diagnosis:
BBS is the second most common cause of retinal degeneration, after Usher syndrome, which is the first one. Usher syndrome is also associated with sensorineural hearing loss. The genetic similarities with other ciliopathic conditions make it difficult to diagnose.
Bardet-Biedl Syndrome Diagnosis
The diagnosis requires medical and family history, along with physical assessment, laboratory tests, and genetic testing.
Clinical Diagnostic Criteria:
Medical professionals diagnose Bardet-Biedl Syndrome through its four core symptoms, which consist of retinal dystrophy and extra fingers or toes and obesity, and kidney disorders. A diagnosis is made when patients present these features along with or without some minor features.
Additional symptoms are developmental delays and speech difficulties, together with other health problems mentioned above. A doctor begins by taking your medical history before performing a physical checkup and conducting tests for your eyesight and kidney function. Regular eye exams should be performed to help detect retinal dystrophy.
Genetic Testing & Prenatal Diagnosis:
The diagnosis requires genetic testing for confirmation. There are more than 20 BBS genes that can be mutated. Genetic tests detect these mutations in people who have the syndrome. These tests assist families in making future decisions.
The tests for Bardet-Biedl Syndrome families are also available when there is a known history of the condition. Medical tests that extract cells from amniocentesis or chorionic villus sampling enable doctors to diagnose genetic disorders. Early detection of problems enables families to prepare for their plans.
Bardet-Biedl Syndrome Treatment & Management
Currently, there is no definitive cure for Bardet-Biedl Syndrome, yet patients can still learn to manage its symptoms. A treatment plan with effective approaches must be established to address this complicated disease.
The most important step in managing Bardet-Biedl syndrome is regular medical evaluations. Due to its multisystem involvement, routine check-ups are recommended to manage complications and support a better quality of life.
- Growth & Nutrition: Monitor height, weight, waist circumference, diet, and physical activity at every visit. Focus on following a balanced diet with regular physical activity. A professional nutritionist’s advice becomes helpful during specific situations.
- Vision: Regular annual ophthalmologic evaluations are recommended to assess progressive vision loss. Patients who suffer from vision loss can use low vision aids together with mobility training as part of their treatment.
- Dental Health: Routine dental checkups starting at age one, every 6 months.
- Heart & Abdomen: Echocardiogram and abdominal ultrasound as needed or if symptoms arise.
- Respiratory: Annual screening for sleep apnea and frequent respiratory infections.
- Gastrointestinal: Check for signs of inflammatory bowel disease, celiac disease, or structural issues yearly.
- Liver & Metabolic: Annual liver function tests and metabolic screening (lipids, glucose, HbA1c) from early childhood.
- Kidney Health: Renal ultrasound, blood pressure, and lab tests annually to monitor their kidney function. Patients who have advanced kidney disease might need dialysis or a kidney transplant as a treatment option.
- Thyroid Function: Test annually to detect any dysfunction.
- Reproductive Health: Hormone evaluation and pelvic imaging in adolescents, if needed.
- Musculoskeletal: Imaging only if abnormalities are suspected.
- Developmental & Psychiatric: Early neurodevelopmental screening and regular behavioral assessments during school years.
- Genetic Counseling: Offered every 1–2 years to support family planning and education.
- Support Services: Ongoing assessment for social, educational, and community support needs.
Multidisciplinary Care Approach:
Bardet-Biedl Syndrome requires medical management from multiple specialists. A team of healthcare professionals who specialize in genetics along with ophthalmology and endocrinology, and nephrology collaborate to provide treatment. The medical team creates a customized care strategy that reflects the specific requirements of each patient.
When the medical team works together using a targeted strategy, patients with Bardet-Biedl Syndrome will achieve a better quality of life.
Bardet-Biedl Syndrome Prognosis
Life Expectancy & Prognosis:
Patients with Bardet-Biedl Syndrome (BBS) face health challenges mainly due to medical issues and lifestyle limitations. Each patient’s outcome depends on kidney involvement, obesity control, diabetes, and hypertension.
Renal disease is the main risk factor for BBS patients. It greatly affects life expectancy. Early chronic kidney disease can lead to kidney failure, requiring dialysis or a transplant. However, with early diagnosis and proper medical care, patients can have a better chance of surviving into adulthood.
Educational & Vocational Challenges:
BBS patients face educational and job challenges. These problems come from learning difficulties, concentration issues, and eye health conditions. The level of cognitive impairment stays mild to moderate, so early infant teaching support, together with individualized education plans, leads to positive educational results.
Vocational training, together with assistive technologies, provides these patients with the opportunity to become more independent.
Support Resources & Community Connections:
The availability of resources and organizations strongly influences the outcome of BBS. These organizations offer support, educational programs, and emotional help to families. In this way, people develop connections to increase confidence while uniting individuals.
The Bardet-Biedl Syndrome Foundation supports families and arranges community meetings for its members. Joining these organizations can improve life quality. Members also learn ways to handle challenges from rare genetic disorders.13Forsythe E, Beales PL. Bardet-Biedl Syndrome. In: Adam MP, Mirzaa GM, Pagon RA, et al., editors. GeneReviews®. Seattle (WA): University of Washington, Seattle; 1993–2024.
Conclusion
Bardet-Biedl syndrome is a genetic disorder that affects many body systems simultaneously. The main symptoms of this disease are retinal dystrophy, obesity, and polydactyly. Renal abnormalities are also common. Proper management of Bardet-Biedl syndrome requires collaboration between doctors and other healthcare workers. The disease requires immediate diagnosis and treatment for patients to lead better lives.
There is no permanent cure for this disease, but combining teaching support with education plans plays a big role. People should be made aware of Bardet-Biedl syndrome. Community support and organizations enable better support for those who have been impacted. The scientists are constantly searching for improved therapeutic solutions.
Refrences
- 1Forsythe E, Beales PL. Bardet-Biedl Syndrome. In: GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993–2024.
- 2Nachury MV, Mick DU. Establishing and regulating the composition of cilia for signal transduction. Nat Rev Mol Cell Biol. 2019;20(7):389–405.
- 3Green JS, Parfrey PS, Harnett JD, et al. The cardinal manifestations of Bardet-Biedl syndrome, a form of Laurence-Moon-Biedl syndrome. N Engl J Med. 1989;321(15):1002–1009.
- 4Khan SA, Muhammad N, Khan MA, Kamal A, Rehman ZU, Khan S. Genetics of human Bardet-Biedl syndrome, an updates. Clin Genet. 2016;90(1):3–15.
- 5Huber C, Delezoide AL, Guimiot F, et al. A large-scale mutation search in Bardet-Biedl syndrome loci. J Med Genet. 2010;47(11):705–712.
- 6Iannaccone A, Mykytyn K, Persico AM, et al. Clinical and functional aspects of Bardet-Biedl syndrome: insights from a multidisciplinary perspective. Retina. 2009;29(4):453–463.
- 7Feuillan PP, Ng D, Han JC, et al. Patients with Bardet-Biedl syndrome have hyperleptinemia suggestive of leptin resistance. J Clin Endocrinol Metab. 2011;96(3):E528–E535
- 8Katsanis N. The oligogenic properties of Bardet-Biedl syndrome. Hum Mol Genet. 2004;13 Spec No 1:R65–R71.
- 9Beales PL, Elcioglu N, Woolf AS, Parker D, Flinter FA. New criteria for improved diagnosis of Bardet-Biedl syndrome: results of a population survey. J Med Genet. 1999;36(6):437–446.
- 10Dattani MT, Guffanti A, Taylor D, et al. Endocrine abnormalities in Bardet-Biedl syndrome. Clin Endocrinol (Oxf). 2013;78(3):364–370.
- 11Imhoff O, Marion V, Stoetzel C, et al. Bardet-Biedl syndrome: a study of the renal and cardiovascular phenotypes in a French cohort. Clin J Am Soc Nephrol. 2011;6(1):22–29.
- 12Tobin JL, Beales PL. Bardet-Biedl syndrome: beyond the cilium. Pediatr Nephrol. 2007;22(7):926–936.
- 13Forsythe E, Beales PL. Bardet-Biedl Syndrome. In: Adam MP, Mirzaa GM, Pagon RA, et al., editors. GeneReviews®. Seattle (WA): University of Washington, Seattle; 1993–2024.