What is Lumber Scoliosis?
Lumbar spine scoliosis is an abnormal sideways curvature of the spine at the lower back. Scoliosis can affect any spine region, i.e., thoracic, lumbar, or thoracolumbar (vertebrae of both thoracic and lumbar sections are involved). The degree of deflection can be mild, moderate, or severe (in rare cases). In a study, the prevalence of scoliosis in children was found to be 3.1%.1Li, M., Nie, Q., Liu, J., & Jiang, Z. (2024). Prevalence of scoliosis in children and adolescents: a systematic review and meta-analysis. *Frontiers in Pediatrics*, 12. https://doi.org/10.3389/fped.2024.1399049 Women are more likely to develop scoliosis. The exact cause of lumbar scoliosis is unknown, but the spine deformity is linked to multiple musculoskeletal disorders.
Most patients experience a mild type of the disorder, and there are no evident symptoms. However, the abnormal position of the backbone can stress the musculature, leading to back pain and nerve symptoms. Doctors usually diagnose the condition in adolescence and use the letters “S” and “C” to describe the curvature. Treatment involves scoliosis braces, physical therapy/exercises, and surgery.
Structure Of The Spine
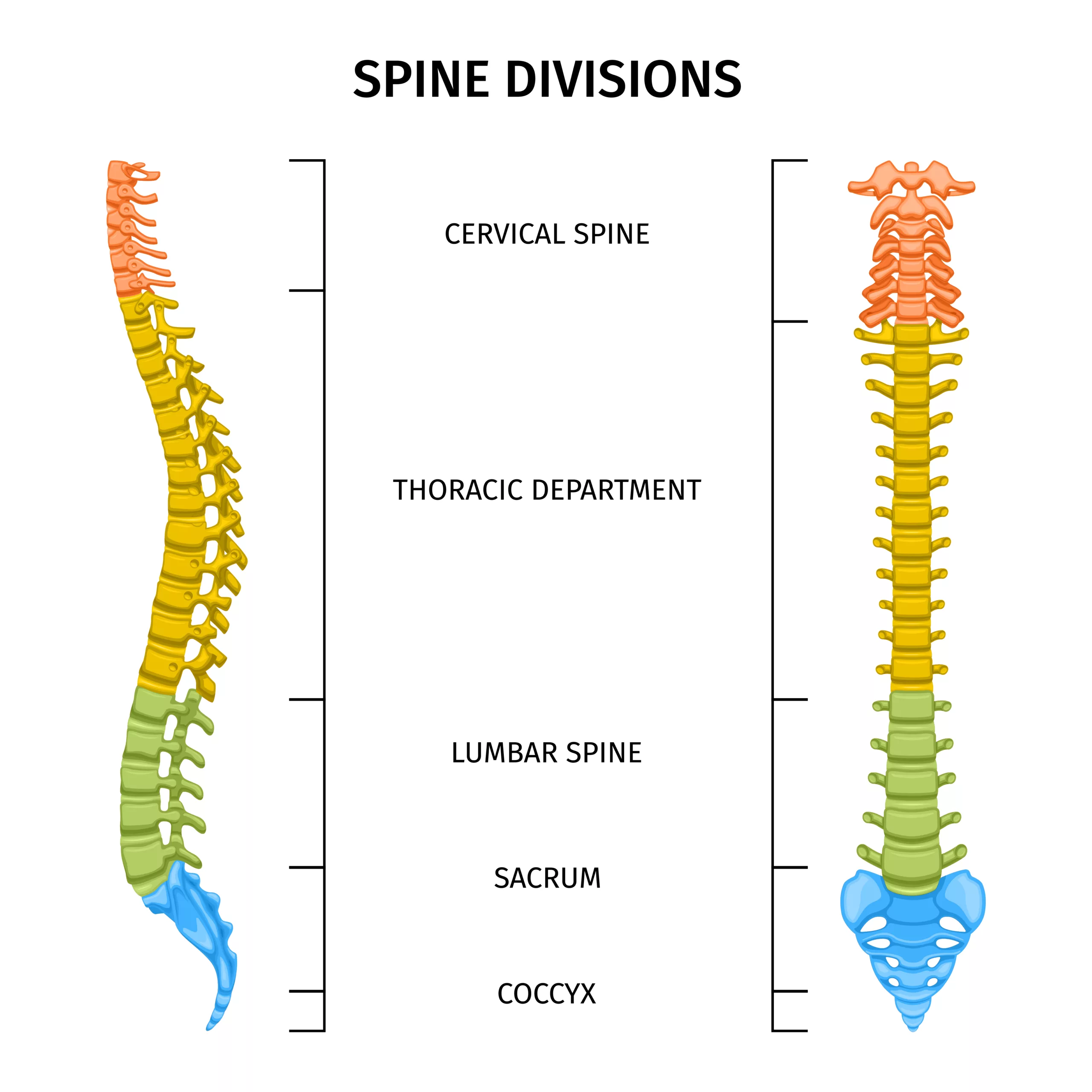
Doctors divide the spine into three main regions:
- Cervical (neck region)
- Thoracic (Upper back region)
- Lumbar (Lower back region)
Scoliosis that develops in the lumbar region is called lumbar spine scoliosis or simply lumbar scoliosis.
Types Of Lumbar Scoliosis
Based on the underlying cause, doctors divide lumbar scoliosis into different types:
Congenital Scoliosis
This type of scoliosis affects the patients within the womb. Congenital scoliosis has an incidence of 0.5-1/1000 births and accounts for 10% of all scoliotic deformities.2Sebaaly, A., Daher, M., Salameh, B., Ghoul, A., George, S., & Roukoz, S. (2022). Congenital scoliosis: a narrative review and proposal of a treatment algorithm. EFORT Open Reviews, 7(5), 318-327. This disorder is commonly seen in patients born with muscular dystrophy and other neuromuscular disorders. Early diagnostic imaging (X-rays, MRIs, and CT scans) plays an important role in timely treatment.
Idiopathic Scoliosis
Any disease that arises spontaneously (without any known cause) is called idiopathic. This type of scoliosis has the highest prevalence among all forms. Based on the age of development, there are different types of idiopathic scoliosis:
Infantile Scoliosis
The earliest to develop is the infantile idiopathic scoliosis (IIS). The disease may resolve without intervention but can potentially worsen over time. If left untreated, IIS can progress to permanent disfigurement.3Janicki, J. A., & Alman, B. (2007). Scoliosis: Review of diagnosis and treatment. Pediatrics & Child Health, 12(9), 771-776.
Juveline/Early Onset Scoliosis
The condition is termed juvenile scoliosis if the symptoms appear before ten years of age. Patients start developing abnormal curvature of the spine at a young age. Early diagnosis is crucial because idiopathic scoliosis tends to progress during growth.4Di Felice, F., Zaina, F., Donzelli, S., & Negrini, S. (2018). The natural history of idiopathic scoliosis during growth: a meta-analysis. American journal of physical medicine & rehabilitation, 97(5), 346-356.
Adolescent Idiopathic Scoliosis (AIS)
The adolescent type affects 2-3% of the population, with only a fraction of patients suffering from severe curvature.5Weinstein, S. L. (2019). The natural history of adolescent idiopathic scoliosis. Journal of Pediatric Orthopaedics, 39, S44-S46. The age of diagnosis for AIS is 10-18. There is a tendency for the disease to aggravate during the growth spurt. For diagnosis of this peripubertal stage, there should be a minimum of 10° curvature in the spine.6Kikanloo, S. R., Tarpada, S. P., & Cho, W. (2019). Etiology of adolescent idiopathic scoliosis: a literature review. Asian Spine Journal, 13(3), 519.
Adult Idiopathic Scoliosis (Degenerative Scoliosis)
Adult or late-onset idiopathic scoliosis is called degenerative scoliosis. As people age, the vertebral bones and joints wear and tear. Uneven bone loss and wear contribute to the curving of the spine. Degenerative lumbar scoliosis is seen in elderly patients (above 18 years) and can be symptomatic.
Neuromuscular Scoliosis
As the name indicates, this type of scoliosis arises due to an underlying neuromuscular disorder. The spine gets an unusual curvature due to brain-muscle incoordination. It is seen in patients with cerebral palsy, Duchenne muscular dystrophy, spinal muscular atrophy, etc. The most commonly involved spine regions are thoracic and lumbar.7Loughenbury, P. R., & Tsirikos, A. I. (2022). Current concepts in the treatment of neuromuscular scoliosis: clinical assessment, treatment options, and surgical outcomes. Bone & joint open, 3(1), 85-92.
Lumbar Scoliosis Symptoms
Some patients do not experience any symptoms if the degree of deflection is low. However, depending on your condition, you may experience mild or severe symptoms. When symptomatic, the most commonly encountered symptoms include:
Low Back Pain
The unusual curvature of the spine puts pressure on the back muscles, which can, in turn, impinge the nerves innervating the lower back and legs. Even mild scoliosis patients report low back pain as a major issue. Degenerative scoliosis patients experience low back pain as a result of disc degeneration and consequent ligament damage.
Adolescent idiopathic scoliosis patients frequently report back pain. As per a study, 90% of AIS patients suffered from some low back pain (over the last six months). Mild symptoms were seen in 37.5% of patients, while 6.5% reported severe pain. The study concluded that AIS-induced back pain is multifactorial and is associated with psychological and morphological factors.8Teles, A. R., St-Georges, M., Abduljabbar, F., Simões, L., Jiang, F., Saran, N., … & Ferland, C. E. (2020). Back pain in adolescents with idiopathic scoliosis: the contribution of morphological and psychological factors. European Spine Journal, 29(8), 1959-1971.
A 2024 study revealed that nearly half of all newly diagnosed AIS patients experience back pain. For most patients, the lumbar curvature was the most painful point.9Sarkovich, S., Leonardi, C., Darlow, M., Martin, D., Issa, P., Soria, T., … & Clement, C. (2024). Back pain in adolescent idiopathic scoliosis: frequency and risk factors. Spine Deformity, 1-9. In addition to radiating back pain, patients may experience nerve symptoms, including numbness, burning and tingling, etc.
Postural Abnormalities
The spine tries to compensate for the deflections, and therefore, there are changes in the posture. The degree of deflection increases rapidly during the growth spurt. Thus, the greatest postural abnormality is seen during this phase. Clinical research reveals that large postural changes can also contribute to low back pain.10Makino, T., Kaito, T., Sakai, Y., Takenaka, S., & Yoshikawa, H. (2019). Health-related quality of life and postural spinal alignment changes in female adolescents associated with back pain in adolescent idiopathic scoliosis: a prospective cross-sectional study. Spine, 44(14), E833-E840.
Changes In Gait &Balance Issues
Patients also notice changes in walking. Balance issues often accompany these negative changes. Kinematics and electromyographic analysis of lumbar scoliosis patients revealed that even mild changes in gait had significant effects on generalized health. Gait analysis showed there was a reduced pelvic frontal motion.11Mahaudens, P., Banse, X., Mousny, M., & Detrembleur, C. (2009). Gait in adolescent idiopathic scoliosis: kinematics and electromyographic analysis. European Spine Journal, 18, 512-521. Walking becomes difficult because most individuals have difficulty balancing the body.
Disfigurement
There is a noticeable twist in the back when scoliosis is moderate to severe. Moreover, uneven hips contribute to walking and balance issues.
Lumbar Scoliosis Causes
The exact cause of lumbar scoliosis is unknown. This is why 80% of the cases fall under idiopathic scoliosis.
Genetics
Idiopathic lumbar scoliosis is a multifactorial disease. Genetic and epigenetic factors (changes in genetics) contribute to the development of AIS. As per a modern study, epigenetics and genetic variants contribute directly to the increase in AIS risk.12Pérez-Machado, G., Berenguer-Pascual, E., Bovea-Marco, M., Rubio-Belmar, P. A., García-López, E., Garzón, M. J., … & García-Giménez, J. L. (2020). From genetics to epigenetics to unravel the etiology of adolescent idiopathic scoliosis. Bone, 140, 115563. Another study revealed a genetic predisposition in degenerative lumbar scoliosis cases.13Shin, J. H., Ha, K. Y., Jung, S. H., & Chung, Y. J. (2011). Genetic predisposition in degenerative lumbar scoliosis due to the copy number variation. Spine, 36(21), 1782-1793. Thus, genetics seem to play a significant role in lumbar scoliosis.
Injury
Spinal injuries can lead to twisting of the spine, which can then turn into scoliosis. These injuries lay the foundation for changes in posture.
Tumor
Though rare, very large tumors tend to shift the spinal alignment, leading to spinal curvature defects like scoliosis and kyphosis, etc. Ganglioneuromas are rare and benign spinal tumors that can deflect the spine, leading to marked scoliosis.14Gaddipati, R., Ma, J., Dayawansa, S., Shan, Y., Huang, J. H., Garrett, D., & Qaiser, R. (2021). Lumbar ganglioneuroma presenting with scoliosis. Cureus, 13(7).
Risk Factors
The following are the most common risk factors for lumbar scoliosis:
- Family history of scoliosis (degenerative scoliosis)
- Underlying neuromuscular condition (cerebral dystrophy, muscular dystrophy, etc.)
- Osteoporosis
- Spinal injuries
- Spinal tumors
How To Diagnose Lumbar Scoliosis?
History (Medical & Family)
A healthcare professional takes a complete history of the patient. He may ask when the patient first noticed the curvature. In the case of adolescent patients, parents are informed about the changes. A history of spinal injury and the presence of scoliosis in family members is important. After taking the history, the doctor may perform a scoliosis screening.
Scoliosis Screening
In screening, a healthcare professional asks the patient to expose his back (take off the clothes) and stand straight. Next, he performs the Adam’s bend test, which requires the patient to bend forward while the doctor analyzes abnormal curvatures in the lumbar spine. Some doctors use a modified Adam’s forward bending test (that correlates axial rotation with sideways-bending movement).15Senkoylu, A., Ilhan, M. N., Altun, N., Samartzis, D., & Luk, K. D. (2021). A simple method for assessing rotational flexibility in adolescent idiopathic scoliosis: modified Adam’s forward bending test. Spine deformity, 9, 333-339.
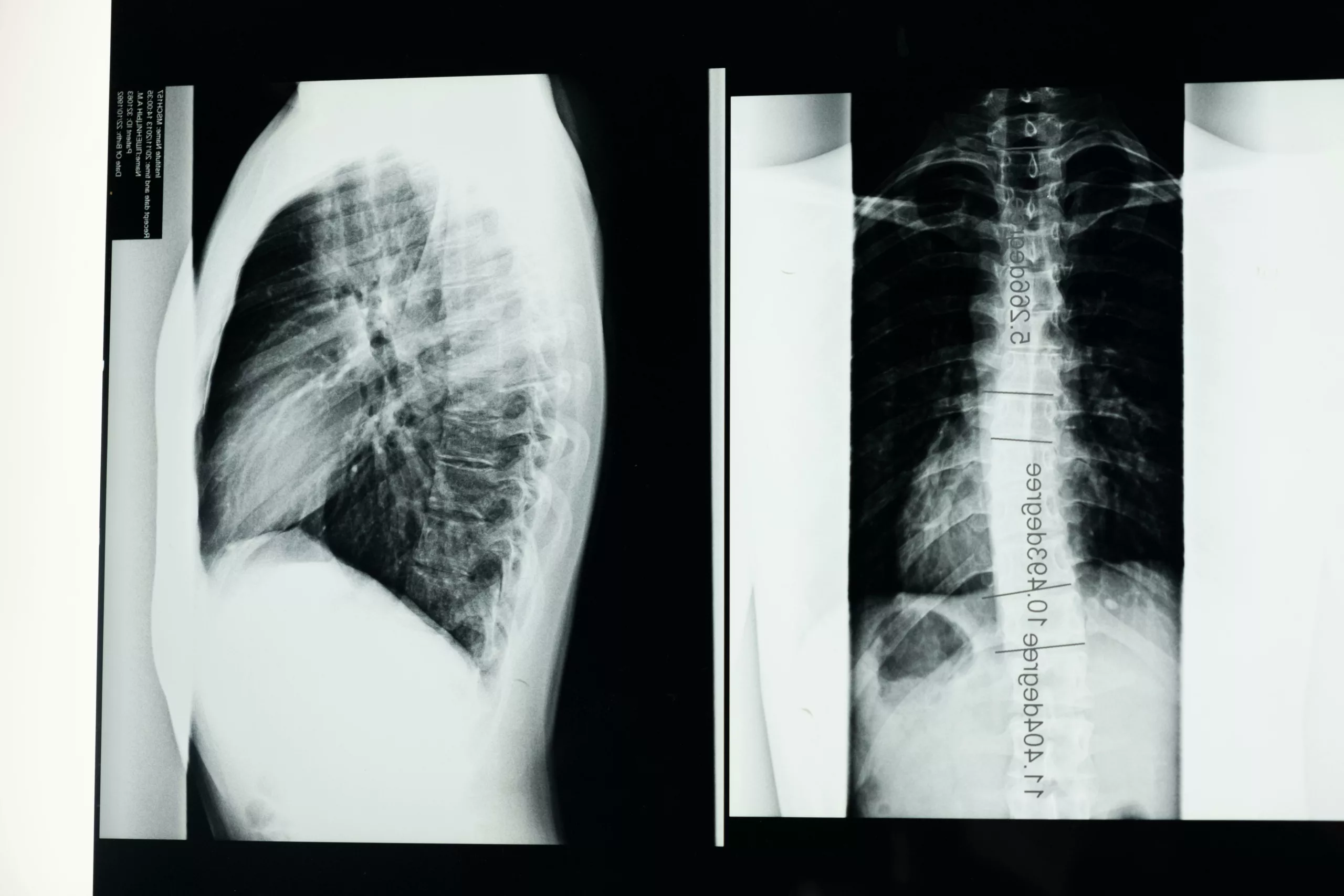
Diagnostic Imaging
Doctors usually order various diagnostic images to get a better picture of the spine.
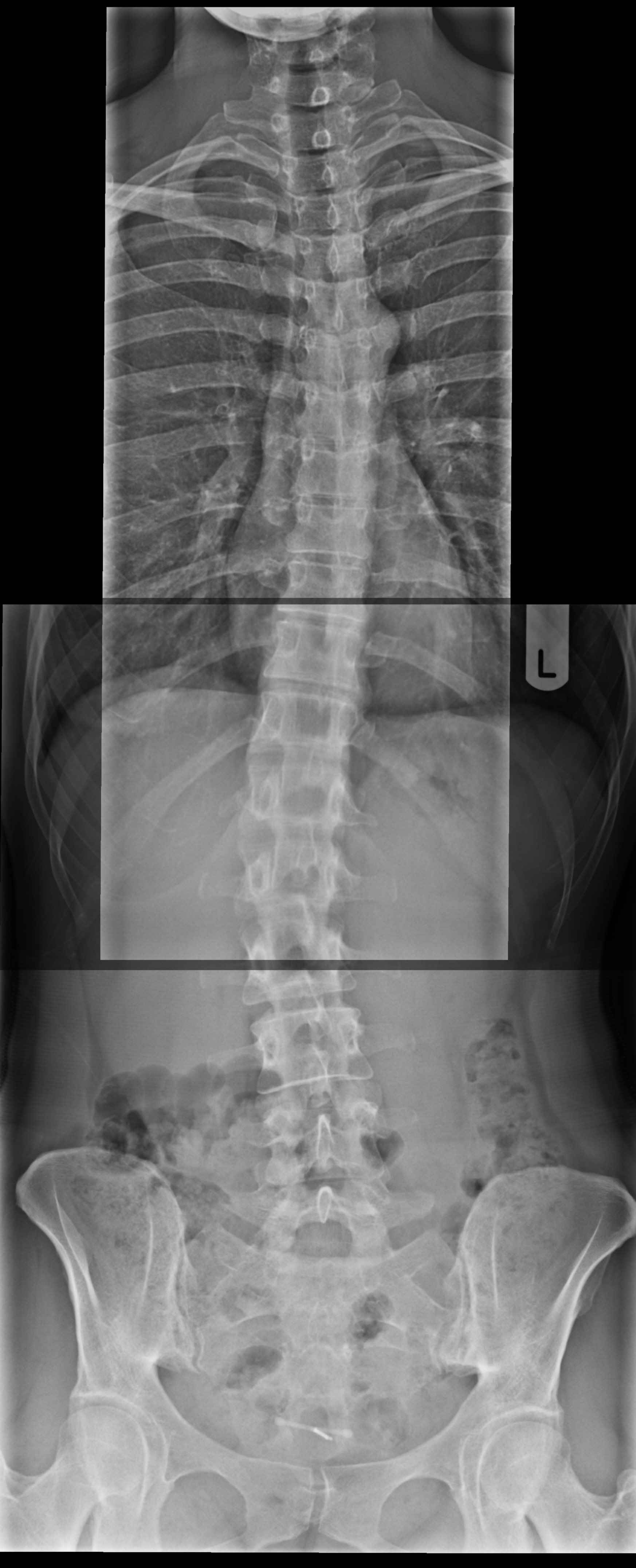
The most common radiographic images include:
- X-rays
- CT scans
- MRI scans
Advanced cases are referred to orthopedic specialists.
Classification Of Lumbar Scoliosis (Cobb Angle)
Minor sideways deflections of the spine are considered normal. However, your doctor will identify the condition as scoliosis if the deflection is 10° or more. Most doctors use a special protractor called a scoliometer to measure the curve on the body. The angle
Based on the Cobb angle, forms of lumbar scoliosis are:
- Mild scoliosis: When the deflection is 10 to 24°.
- Moderate scoliosis: When the deflection is 25 to 39°
- Severe scoliosis: When the deflection is 40°or more.
- Very severe scoliosis: When the deflection is greater than 80°.
Lumbar Scoliosis Treatment
The ideal treatment type varies with the extent and location of the disorder. The most prevalent types of lumbar scoliosis treatment include:
Observation
In most mild scoliosis cases, doctors merely observe the patient. The patient is advised to get regular spine scans to check the progression of the disease. If there are no symptoms or signs of disease progression, most professionals take a typical approach.
Medications And Injections
Doctors prescribe over-the-counter painkillers (like ibuprofen, naproxen, etc.) to control AIS-induced pain. Nerve-blocking may be prescribed in cases of severe nerve impingement where medicines do not respond.
Scoliosis Bracing
Bracing is the most common non-invasive treatment modality for adolescent idiopathic lumbar scoliosis. A brace holds the spine in place. Different types of braces are available, including soft, semi-rigid, and rigid. Young patients have to wear braces during periods of growth.
According to studies, bracing positively controls scoliosis progression (increase of Cobb angle).16Babaee, T., Moradi, V., Hashemi, H., Shariat, A., Anastasio, A. T., Khosposterior percutaneous instrumentation withravi, M., & Bagheripour, B. (2023). Does bracing control the progression of adolescent idiopathic scoliosis in curves higher than 40? A systematic review and meta-analysis. Asian Spine Journal, 17(1), 203. Researchers have noted the effectiveness and general patient acceptance of braces.17Grivas, T. B., Negrini, S., Aubin, C. E., Aulisa, A. G., De Mauroy, J. C., Donzelli, S., … & Zaina, F. (2022). Nonoperative management of adolescent idiopathic scoliosis (AIS) using braces. Prosthetics and Orthotics International, 46(4), 383-391.
Physical Therapy
Physiotherapy sessions can aid in alleviating symptoms. The mobilization of the spinal joints (by a physiotherapist) regulates blood flow and helps improve muscular control. Several patients report significant improvements in balance and stability while walking.
Surgery
Surgeons opt for the type of surgery depending on the degree of deflection (Cobb angle), symptoms, and patient age. For mild to moderate acute spinal deformity, there are minimally invasive techniques that combine posterior percutaneous instrumentation with lateral interbody fusion cages. In posterior percutaneous instrumentation, small incisions are made in the back to insert screws, combined with lateral interbody fusion cages. These cages, placed between the vertebrae, help stabilize the spine, restore proper alignment, and relieve pressure on the compressed nerves. This procedure aligns the vertebral column and decompresses the nerves.
For severe cases (large deformities), surgeons perform a spinal fusion surgery. There are different techniques of fusion, but the most effective one is lumbosacral fusion with double rods.18Charles, Y. P., & Ntilikina, Y. (2020). Scoliosis surgery in adulthood: what challenges for what outcome? Annals of Translational Medicine, 8(2). Surgery has pitfalls. Therefore, it is reserved only for patients who don’t respond to non-invasive therapies.
Lumbar Scoliosis Exercises
Stretching and keeping the lumbar/pelvic region mobile can slow down the progression of the disease and keep symptoms at bay. You can adopt the following exercises to keep your spine healthy:
- Pelvic tilts
- Cat-cow pose
- Abdominal press
- Leg raises
Final Word
Lumbar scoliosis is an abnormal side-to-side deflection of the lumbar spine. The condition is rare and is mostly of idiopathic origin (unknown causes). Young individuals (infants to adolescents) are common targets. The spinal deformity disorder is usually present in patients with muscular dystrophy and other neuromuscular disorders.
Mild lumbar scoliosis is mostly asymptomatic. However, symptoms are seen in mild-to-moderate scoliosis. When present, patients report low back pain, gait and postural abnormalities, and balance issues (especially when walking). Most patients visit the clinic for visible deflection in the back and backache. Experts believe genetic and epigenetic factors contribute to the occurrence of disease.
The degree of deflection is measured via the Cobb angle. The condition is mild scoliosis if the angle is 10 to 24° and severe scoliosis if the angle is above 40°. Mild to moderate lumbar scoliosis is corrected with non-invasive techniques like bracing and physical therapy. Pain management is done via medicines and nerve-relieving injections. However, spinal fusion surgery is reserved for severe patients only. Moreover, certain exercises like pelvic tilts and leg raises can alleviate scoliosis symptoms.
Refrences
- 1Li, M., Nie, Q., Liu, J., & Jiang, Z. (2024). Prevalence of scoliosis in children and adolescents: a systematic review and meta-analysis. *Frontiers in Pediatrics*, 12. https://doi.org/10.3389/fped.2024.1399049
- 2Sebaaly, A., Daher, M., Salameh, B., Ghoul, A., George, S., & Roukoz, S. (2022). Congenital scoliosis: a narrative review and proposal of a treatment algorithm. EFORT Open Reviews, 7(5), 318-327.
- 3Janicki, J. A., & Alman, B. (2007). Scoliosis: Review of diagnosis and treatment. Pediatrics & Child Health, 12(9), 771-776.
- 4Di Felice, F., Zaina, F., Donzelli, S., & Negrini, S. (2018). The natural history of idiopathic scoliosis during growth: a meta-analysis. American journal of physical medicine & rehabilitation, 97(5), 346-356.
- 5Weinstein, S. L. (2019). The natural history of adolescent idiopathic scoliosis. Journal of Pediatric Orthopaedics, 39, S44-S46.
- 6Kikanloo, S. R., Tarpada, S. P., & Cho, W. (2019). Etiology of adolescent idiopathic scoliosis: a literature review. Asian Spine Journal, 13(3), 519.
- 7Loughenbury, P. R., & Tsirikos, A. I. (2022). Current concepts in the treatment of neuromuscular scoliosis: clinical assessment, treatment options, and surgical outcomes. Bone & joint open, 3(1), 85-92.
- 8Teles, A. R., St-Georges, M., Abduljabbar, F., Simões, L., Jiang, F., Saran, N., … & Ferland, C. E. (2020). Back pain in adolescents with idiopathic scoliosis: the contribution of morphological and psychological factors. European Spine Journal, 29(8), 1959-1971.
- 9Sarkovich, S., Leonardi, C., Darlow, M., Martin, D., Issa, P., Soria, T., … & Clement, C. (2024). Back pain in adolescent idiopathic scoliosis: frequency and risk factors. Spine Deformity, 1-9.
- 10Makino, T., Kaito, T., Sakai, Y., Takenaka, S., & Yoshikawa, H. (2019). Health-related quality of life and postural spinal alignment changes in female adolescents associated with back pain in adolescent idiopathic scoliosis: a prospective cross-sectional study. Spine, 44(14), E833-E840.
- 11Mahaudens, P., Banse, X., Mousny, M., & Detrembleur, C. (2009). Gait in adolescent idiopathic scoliosis: kinematics and electromyographic analysis. European Spine Journal, 18, 512-521.
- 12Pérez-Machado, G., Berenguer-Pascual, E., Bovea-Marco, M., Rubio-Belmar, P. A., García-López, E., Garzón, M. J., … & García-Giménez, J. L. (2020). From genetics to epigenetics to unravel the etiology of adolescent idiopathic scoliosis. Bone, 140, 115563.
- 13Shin, J. H., Ha, K. Y., Jung, S. H., & Chung, Y. J. (2011). Genetic predisposition in degenerative lumbar scoliosis due to the copy number variation. Spine, 36(21), 1782-1793.
- 14Gaddipati, R., Ma, J., Dayawansa, S., Shan, Y., Huang, J. H., Garrett, D., & Qaiser, R. (2021). Lumbar ganglioneuroma presenting with scoliosis. Cureus, 13(7).
- 15Senkoylu, A., Ilhan, M. N., Altun, N., Samartzis, D., & Luk, K. D. (2021). A simple method for assessing rotational flexibility in adolescent idiopathic scoliosis: modified Adam’s forward bending test. Spine deformity, 9, 333-339.
- 16Babaee, T., Moradi, V., Hashemi, H., Shariat, A., Anastasio, A. T., Khosposterior percutaneous instrumentation withravi, M., & Bagheripour, B. (2023). Does bracing control the progression of adolescent idiopathic scoliosis in curves higher than 40? A systematic review and meta-analysis. Asian Spine Journal, 17(1), 203.
- 17Grivas, T. B., Negrini, S., Aubin, C. E., Aulisa, A. G., De Mauroy, J. C., Donzelli, S., … & Zaina, F. (2022). Nonoperative management of adolescent idiopathic scoliosis (AIS) using braces. Prosthetics and Orthotics International, 46(4), 383-391.
- 18Charles, Y. P., & Ntilikina, Y. (2020). Scoliosis surgery in adulthood: what challenges for what outcome? Annals of Translational Medicine, 8(2).