Trachoma is a contagious eye disease caused by the bacterium Chlamydia trachomatis that causes visual impairment and blindness. It affects the eye’s conjunctiva, causing inflammation and scarring of eyelids with the erosion of the corneas. According to the World Health Organization (WHO)1World Health Organization. (2022). Trachoma. Retrieved from https://www.who.int/news-room/fact-sheets/detail/trachoma, around 1.9 million people suffer from trachoma-induced blindness/visual impairment. Trachoma alone is responsible for 1.4% of all cases of blindness across the globe. The disorder is commonly present in crowded areas with poor hygiene conditions. Treatment involves antibiotic (azithromycin) therapy with hygiene improvement strategies.
Trachoma Stages
There are multiple steps in which trachoma affects the eye structures, eventually leading to blindness. Based on the clinical features, WHO classifies trachoma into five stages.2Solomon, A. W., Kello, A. B., Bangert, M., West, S. K., Taylor, H. R., Tekeraoi, R., & Foster, A. (2020). The simplified trachoma grading system, amended. Bulletin of the World Health Organization, 98(10), 698. The first two stages are inflammatory stages, immediately followed by scarring of the tissues. Thus, they are known as active trachoma.
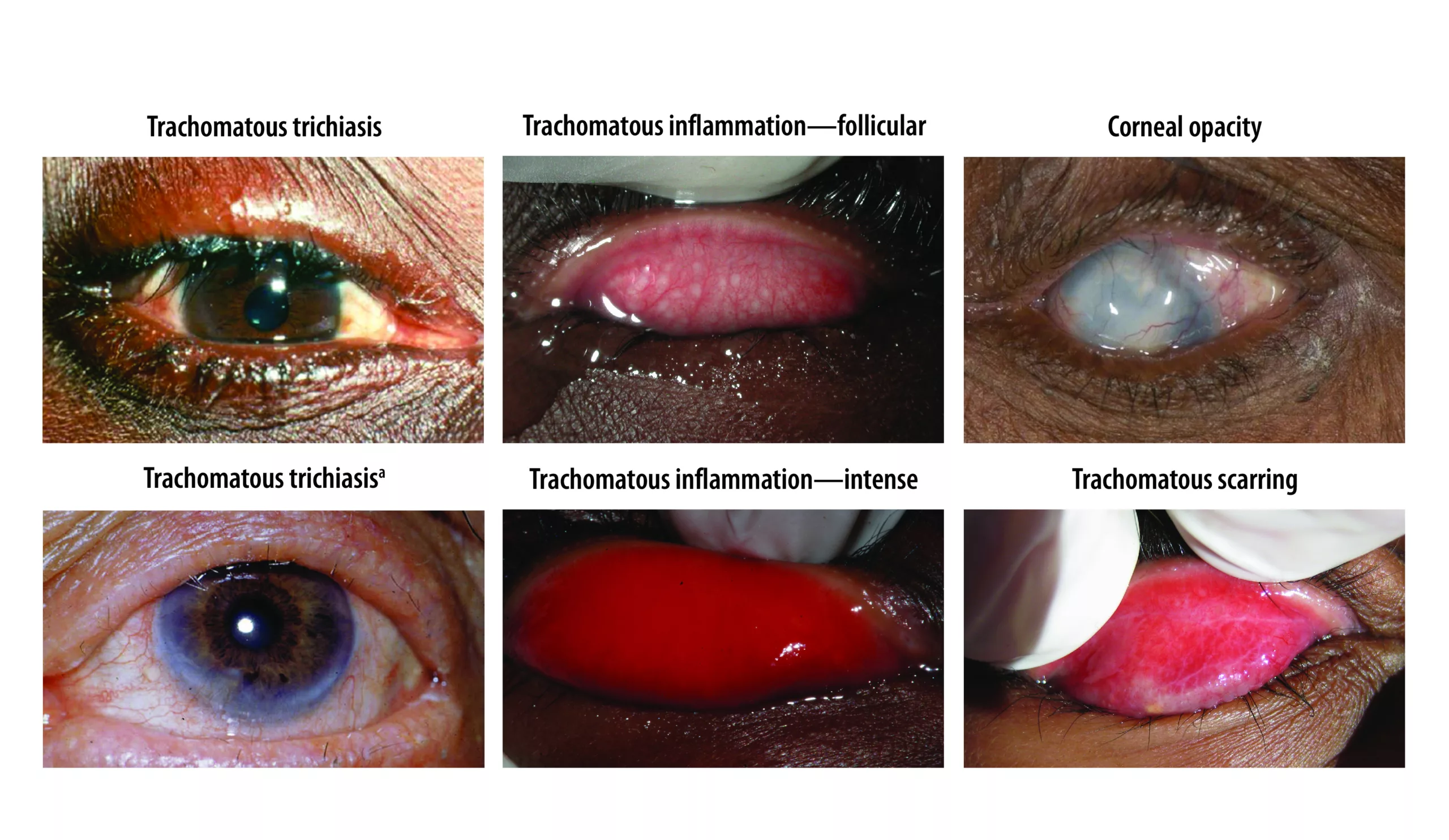
Trachomatous Inflammation-Follicular (TF)
The initial presentation of trachoma is the appearance of small bumps (1-5) on the back of the upper eyelid. The bumps form due to swelling of the lymph tissues in the eyelids. Thus, the bumps can even extend into the upper part of the eye. This stage is easily identifiable in young patients (aged 1-9 years). The prevalence of TF is almost twice in rural children than the WHO standard.3Altaseb, T., Lingerew, M., & Adane, M. (2024). Prevalence of trachomatous inflammation-follicular and associated factors among children aged 1-9 years in northeastern Ethiopia. BMC pediatrics, 24(1), 128. Physicians identify it as the TF stage if five or more follicles of 0.5mm diameter are present in the upper tarsal conjunctiva (part of the conjunctiva that lines the upper eyelid).
Epidemiological studies reveal that numerous individuals suffer merely from trachomatous inflammation follicular without any trachomatous trichiasis.4Atekem, K., Harding-Esch, E. M., Martin, D. L., Downs, P., Palmer, S. L., Kaboré, A., … & Meite, A. (2023). High prevalence of trachomatous inflammation–follicular with no trachomatous trichiasis: can alternative indicators explain the epidemiology of trachoma in Côte d’Ivoire?. International Health, 15(Supplement_2), ii3-ii11.
Trachomatous Inflammation-Intense (TI)
Swelling of the conjunctiva follows lymph tissue swelling in the upper eyelids. Per studies, this inflammation can be attributed to the activation of pro-inflammatory factors (IL17A, CTGF, etc.).5Burton, M. J., Ramadhani, A., Weiss, H. A., Hu, V., Massae, P., Burr, S. E., … & Bailey, R. L. (2011). Active trachoma is associated with increased conjunctival expression of IL17A and profibrotic cytokines. Infection and immunity, 79(12), 4977-4983.Moreover, there is a thickening of the tarsal conjunctiva, which obscures more than half of the deep tarsal blood vessels.
Trachomatous Scarring (TS)
The next step in the progression of trachoma is scarring. In this stage, scar formation initiates. Bands of scars appear in the conjunctiva that line the inside of the upper eyelid. The scars appear as fine, white horizontal lines. These lines or bands are parallel to the edge of the lid.
Trachomatous Trichiasis (TT)
In this stage, the thickening and tightening of the scar bands leads to two eye conditions. Entropion is the inward turning of the eyelid margins. Another condition, trichiasis, accompanies entropion. Trichiasis is a condition in which at least one eyelash rubs against the globe of the eye due to inward turning. Repeated rubbing of the eyes lays the foundation for corneal (outer clear covering layer of the eye) abrasions and permanent damage. This cicatricial stage is mostly seen in the middle ages.
Corneal Opacity
The cornea is the outer, transparent part of the eye that covers the inner iris and pupil. It allows light to enter the sensory structures of the eye. Persistent corneal abrasions (due to trichiasis) eventually lead to the most advanced stage of trachoma, i.e., corneal opacification. Abrasions potentially lead to infectious ulcers in the cornea, which scar, leading to blockage of light (from entering the eye). If left untreated, this leads to vision impairments and complete blindness. Trachoma accounts for a very large number of corneal opacity blindness across the globe.6Wang, E. Y., Kong, X., Wolle, M., Gasquet, N., Ssekasanvu, J., Mariotti, S. P., … & West, S. (2023). Global trends in blindness and vision impairment resulting from corneal opacity 1984–2020: A meta-analysis. Ophthalmology, 130(8), 863-871.
Trachoma Symptoms
Redness/Irritation And Tears
Eye redness is the initial symptom of trachoma. Many patients do not take it seriously because it resembles pink eye (conjunctivitis).

Eye irritation and redness are the first signs to appear. Irritation causes excessive tear production and discharge.
Discharge From Eyes & Nose
Many patients also complain of pus discharge from the eyes and nose. This is due to infection by the Chlamydia bacteria.
Eye Pain
The infection itself does not cause significant pain, so there is no ache during the initial stages of the disease. However, patients suffer from eye pain due to scrapping of the cornea with the eyelids. Young children are common targets; therefore, eye pain can be a major concern.
Eyelid Tightening
Scar bands also tighten the eyelids, making eye blinking and movement difficult. Labored blinking irritates and decreases generalized health.
Light Sensitivity/Intolerance
Patients with trachoma trichiasis often report a history of light intolerance and involuntary closure of both eyelids, i.e., blepharospasm. Several individuals complain of persistent pain and light intolerance.
Vision Loss/Blindness
The degeneration of the corneal layers leads to irreversible blindness (if not treated timely). Different factors, like inward turning of the eyelids and repeated corneal friction, contribute to blindness. As per reports, trachoma is the oldest known cause of human blindness.7Martini, M., Riccardi, N., Simonetti, O., Orsini, D., Samassa, F., & Parodi, A. (2024). “The blinding disease”. The history of trachoma in Italians between the 19th and 20th centuries: colonial or national blindness? Pathogens and Global Health, 1-6.
Trachoma Causes
Various serovars (types) of the C.trachomatis bacterium are responsible for the development of trachoma. The most common infection-causing serovars include:
- A
- B
- Ba
- C
Serovars D to K are responsible for adult conjunctivitis. Chlamydia infection induces conjunctival scarring. Collagen and fibronectin deposit at the scarring site, leading to fibrosis of the conjunctival tissues. The body undergoes recurrent cycles of tissue repair and inflammation to correct this scarring. Thus, the healing cycle results in entropion and trichiasis, eventually leading to blindness. The interaction between the bacterium and the host’s immune system causes scarring (conjunctival), inflammation, and tissue destruction.
Risk Groups
Chlamydia trachomatis survives in unclean water. Thus, individuals in trachoma-endemic areas are at a greater risk. The majority of cases are in the Sub-Saharan Africa region. However, affected individuals can also be found in the Middle East, South America, and Asia. As of 2022, around 125 million people were at risk of trachoma blindness.
Is Trachoma Contagious?
Yes, trachoma can spread from contact with an infected person. You can acquire the bacteria if an infected person’s eye/nasal discharge comes in contact by physical contact (touching) or sharing infected clothing/bedding. However, it generally takes around 5-12 days for symptoms to appear (after exposure to bacteria).
How Does Trachoma Spread?
Trachoma is known to spread via flies. Unhygienic water is another cause of the spread of the bacterial infection. A cluster-randomised controlled trial revealed that fly control maneuvers and provision of latrines significantly reduced trachoma prevalence in children indicating the role of flies in trachoma spread.8Emerson, P. M., Lindsay, S. W., Alexander, N., Bah, M., Dibba, S. M., Faal, H. B., … & Bailey, R. L. (2004). Role of flies and provision of latrines in trachoma control: cluster-randomised controlled trial. The Lancet, 363(9415), 1093-1098.
How Is Trachoma Diagnosed?
History
An ophthalmologist (eye doctor) starts by taking your history. The doctor asks about symptoms like eye irritation, redness, or photosensitivity. The patient’s residence and/or travel to endemic areas (like North Africa, the Middle East, and India) are important questions.
Physical Examination & Tests
If the history (medical and travel history) and symptoms of the patient correlate, the doctor goes on to perform a physical examination. Your doctor will evaluate the follicles in the eyelids and check for signs of conjunctival inflammation. Clinicians also examine the integrity of the cornea and the extent of scarring on the conjunctiva. Any signs of entropion and trichiasis are duly noted.9Diallo AO, Bayissasse B, Sisay A, Seyum D, Weaver J, Munoz B, Merbs SL, Gower EW. Effectiveness of Trachomatous Trichiasis Case-identification Approaches in Ethiopia. Epidemiology. 2023 Nov 1;34(6):909-920. doi: 10.1097/EDE.0000000000001656. Epub 2023 Sep 26. PMID: 37757880.
Your healthcare provider may also check visual acuity to assess visual impairments. Common methods of acuity check include visual acuity cards and Snellen charts.
Lab Examinations include tests to identify bacterial cells in the eye contents of the patient. In microbiological testing, a sample of fluid (swab) is taken from the patient’s eye (conjunctiva) and sent to the lab to examine C.trachomaits DNA.
Clinical Evaluation
Once trachoma is diagnosed, the doctor grades Trachoma based on WHO’s guidelines. The patient is put under any one of the five stages (TI to CO).
Some doctors also take help from radiographs and artificial intelligence for trachoma diagnosis.
Differential Diagnosis
Several ocular disorders have presentations similar to trachoma. Thus, it is very important to differentiate trachoma from other eye disorders.
Conjunctivitis Vs. Trachoma
Initial symptoms (tearing, redness, etc.) are similar, but allergic conjunctivitis is associated with a prior exposure to allergens (dust, pollen, etc.). On the other hand, symptoms of bacterial conjunctivitis appear rapidly and resolve spontaneously.
Dry Eye Syndrome
Patients with dry eye syndrome and trachoma experience eye pain, redness, and swelling. However, there is pronounced dryness and a lack of tearing in dry syndrome cases.
Trachoma Treatment/Management
The most effective treatment method for trachoma is the WHO-guided SAFE strategy, i.e., surgery (S), antibiotics (A), facial cleanliness (F), and environmental improvement (E). A decline in disease prevalence is seen with the implementation of the SAFE strategy.10Olamiju, F., Isiyaku, S., Olobio, N., Mogaji, H., Achu, I., Muhammad, N., … & Mpyet, C. D. (2023). Prevalence of trachoma following implementation of the SAFE strategy in three local government areas of Taraba State, North Eastern Nigeria. Ophthalmic epidemiology, 30(6), 619-627.
Antibiotic Therapy
Antibiotic administration is the first line of treatment for early trachoma. The spread of trachoma is unavoidable; therefore, the whole family must receive antibiotic treatment. The best results are seen with Azithromycin (20mg/kg). A one-time use of oral azithromycin is effective in alleviating symptoms. According to a systematic review, community-wide (mass drug administration) treatment with oral azithromycin significantly reduces C.trachomatis infection (in endemic regions).11Xiong, T., Yue, Y., Li, W. X., Choonara, I., Qazi, S., Chen, H. J., … & Mu, D. Z. (2021). Effectiveness of azithromycin mass drug administration on trachoma: a systematic review. Chinese Medical Journal, 134(24), 2944-2953. Another oral drug for trachoma management is erythromycin (500mg twice daily for two weeks).
Tetracycline ointments (1%) are less effective than oral drugs but do a good job as a topical drug.
Surgery
Timely diagnosis and treatment can save you from permanent blindness. Surgical intervention is the preferred mode of treatment in cases of entropion and trichiasis. Surgery is often done to prevent abrasion of inverted eyelids that cause corneal abrasion and blindness.
In eyelid rotation surgery (tarsal rotation with bilamellar tarsal rotation), the surgeon makes an incision on the scarred eyelid and rotates the eyelashes. The lashes are then positioned away from the cornea. Thus, there is reduced friction and fewer chances of further vision loss.
Your eye surgeon may opt for epilation, i.e., surgical removal of eyelashes, depending upon your condition.
Other non-surgical ways of destruction of eyelash follicles include cryotherapy, electrocautery, and radiofrequency ablation of follicles.
To correct vision loss from excessive corneal abrasion, a corneal transplantation is done. It is one of the most successful transplantation surgeries and can improve vision.12Singh, R., Gupta, N., Vanathi, M., & Tandon, R. (2019). Corneal transplantation in the modern era. Indian Journal of Medical Research, 150(1), 7-22.
Facial Cleanliness
The lack of facial cleanliness directly contributes to the spread of the infection. Therefore, cleaning the face can prevent the spread of trachoma.

Studies show that the provision of water access helps eliminate trachoma.13Barazanji, M., Ngo, J. D., Powe, J. A., Schneider, K. P., Rychtář, J., & Taylor, D. (2023). Modeling the “F” in “SAFE”: The dynamic game of facial cleanliness in trachoma prevention. Plos one, 18(6), e0287464. However, this step aids in prevention more than treatment.
Environmental Improvement
Steps to improve the environment can help minimize the spread but can not treat infected patients. Governmental and Non-governmental organizations (NGOs) must ensure access to clean drinking water. As most endemic areas are crowded, proper sanitation maneuvers must be adopted to prevent infections. Controlling the population of flies can also result in a decline in infection rates.
Trachoma Prevention
The environmental protection and improvement steps play a significant role in preventing the occurrence of the disease. Furthermore, endemic areas can receive blanket antibiotic therapy. In this therapy, certain areas are selected and children (1-9 year olds) are given antibiotics at least once a year.14Dawson, C & Daghfous, T & Whitcher, J & Messadi, M & Hoshiwara, T & Triki, Fatma & Chadgrah, F & Briones, O & Yoneda, C & Schachter, J. (1981). Intermittent trachoma chemotherapy: A controlled trial of topical tetracycline or erythromycin. Bulletin of the World Health Organization. 59. 91-7.
Final Word
Trachoma is an ocular disorder caused by Chlamydia trachomatis infection. It is a major cause of blindness and mostly affects young children. It is endemic in regions with poor sanitation, a lack of clean water sources, and flies. Trachomatis infection causes inflammation of the eyelids. If left untreated, the eyelids turn inwards (entropion), which leads to rubbing the cornea against the lashes (trichiasis). This rubbing induces corneal abrasions and scarring, which eventually leads to vision impairments and blindness.
According to WHO, the best management strategy for trachoma is the SAFE protocol. Surgery (S) is done to reposition the eyelids (and lashes) so there is no friction between the cornea and eyelids. A single dose of the antibiotic (A) azithromycin is effective in curing young patients. Facial cleanliness (F) decreases the chances of bacterial invasion. Environmental improvement (E) involves ensuring proper sanitation and access to clean drinking water. Improvement in living standards and overall hygiene has helped reduce the prevalence of trachoma.
Refrences
- 1World Health Organization. (2022). Trachoma. Retrieved from https://www.who.int/news-room/fact-sheets/detail/trachoma
- 2Solomon, A. W., Kello, A. B., Bangert, M., West, S. K., Taylor, H. R., Tekeraoi, R., & Foster, A. (2020). The simplified trachoma grading system, amended. Bulletin of the World Health Organization, 98(10), 698.
- 3Altaseb, T., Lingerew, M., & Adane, M. (2024). Prevalence of trachomatous inflammation-follicular and associated factors among children aged 1-9 years in northeastern Ethiopia. BMC pediatrics, 24(1), 128.
- 4Atekem, K., Harding-Esch, E. M., Martin, D. L., Downs, P., Palmer, S. L., Kaboré, A., … & Meite, A. (2023). High prevalence of trachomatous inflammation–follicular with no trachomatous trichiasis: can alternative indicators explain the epidemiology of trachoma in Côte d’Ivoire?. International Health, 15(Supplement_2), ii3-ii11.
- 5Burton, M. J., Ramadhani, A., Weiss, H. A., Hu, V., Massae, P., Burr, S. E., … & Bailey, R. L. (2011). Active trachoma is associated with increased conjunctival expression of IL17A and profibrotic cytokines. Infection and immunity, 79(12), 4977-4983.
- 6Wang, E. Y., Kong, X., Wolle, M., Gasquet, N., Ssekasanvu, J., Mariotti, S. P., … & West, S. (2023). Global trends in blindness and vision impairment resulting from corneal opacity 1984–2020: A meta-analysis. Ophthalmology, 130(8), 863-871.
- 7Martini, M., Riccardi, N., Simonetti, O., Orsini, D., Samassa, F., & Parodi, A. (2024). “The blinding disease”. The history of trachoma in Italians between the 19th and 20th centuries: colonial or national blindness? Pathogens and Global Health, 1-6.
- 8Emerson, P. M., Lindsay, S. W., Alexander, N., Bah, M., Dibba, S. M., Faal, H. B., … & Bailey, R. L. (2004). Role of flies and provision of latrines in trachoma control: cluster-randomised controlled trial. The Lancet, 363(9415), 1093-1098.
- 9Diallo AO, Bayissasse B, Sisay A, Seyum D, Weaver J, Munoz B, Merbs SL, Gower EW. Effectiveness of Trachomatous Trichiasis Case-identification Approaches in Ethiopia. Epidemiology. 2023 Nov 1;34(6):909-920. doi: 10.1097/EDE.0000000000001656. Epub 2023 Sep 26. PMID: 37757880.
- 10Olamiju, F., Isiyaku, S., Olobio, N., Mogaji, H., Achu, I., Muhammad, N., … & Mpyet, C. D. (2023). Prevalence of trachoma following implementation of the SAFE strategy in three local government areas of Taraba State, North Eastern Nigeria. Ophthalmic epidemiology, 30(6), 619-627.
- 11Xiong, T., Yue, Y., Li, W. X., Choonara, I., Qazi, S., Chen, H. J., … & Mu, D. Z. (2021). Effectiveness of azithromycin mass drug administration on trachoma: a systematic review. Chinese Medical Journal, 134(24), 2944-2953.
- 12Singh, R., Gupta, N., Vanathi, M., & Tandon, R. (2019). Corneal transplantation in the modern era. Indian Journal of Medical Research, 150(1), 7-22.
- 13Barazanji, M., Ngo, J. D., Powe, J. A., Schneider, K. P., Rychtář, J., & Taylor, D. (2023). Modeling the “F” in “SAFE”: The dynamic game of facial cleanliness in trachoma prevention. Plos one, 18(6), e0287464.
- 14Dawson, C & Daghfous, T & Whitcher, J & Messadi, M & Hoshiwara, T & Triki, Fatma & Chadgrah, F & Briones, O & Yoneda, C & Schachter, J. (1981). Intermittent trachoma chemotherapy: A controlled trial of topical tetracycline or erythromycin. Bulletin of the World Health Organization. 59. 91-7.