What is Pemphigus Vulgaris?
Pemphigus vulgaris belongs to the group of rare autoimmune disorders in which the body’s immune system mistakenly identifies the epithelial cells, which line the skin and mucous membranes covering organs, as foreign invaders. As a result, the immune system produces antibodies that target and destroy these cells.1Porro, A. M., Seque, C. A., Ferreira, M. C. C., & Enokihara, M. M. S. E. S. (2019). Pemphigus vulgaris. Anais brasileiros de dermatologia, 94(3), 264–278. https://doi.org/10.1590/abd1806-4841.20199011
This autoimmune response leads to the formation of mucocutaneous bullae, which are large, fluid-filled blisters that form on both the skin and mucous membranes. These bullae can be painful and are a hallmark symptom of the disease. The term ‘mucocutaneous’ underscores that these blisters can develop in the skin and the mucous membranes lining various body surfaces. Most of these are red in color and tender on touching. The most common locations of blisters are the nose, throat, mouth, eyes, and genitals. Blisters burst after a few days, leaving behind a sore skin. The development of blisters significantly impacts the quality of life for individuals with pemphigus vulgaris.2Giannetti, L., Generali, L., & Bertoldi, C. (2018). Oral pemphigus. Giornale italiano di dermatologia e venereologia : organo ufficiale, Societa italiana di dermatologia e sifilografia, 153(3), 383–388. https://doi.org/10.23736/S0392-0488.18.05887-X Severe pain associated with these blisters often hinders basic activities such as eating and walking.
Given that pemphigus vulgaris is an autoimmune disease, replacing the faulty immune system is impossible. Therefore, the primary goal of treatment is to minimize blister formation and enable patients to regain a semblance of normalcy in their daily lives.3Ingold, C. J., & Khan, M. A. B. (2023). Pemphigus Vulgaris. In StatPearls. StatPearls Publishing.
Incidence of Pemphigus Vulgaris
The incidence of pemphigus vulgaris is quite low. There is no specific gender and race predilection for its occurrence. However, it is essential to note that pemphigus vulgaris represents the most frequently diagnosed subtype within the pemphigus group. The estimated incidence rate stands at 2.83 cases per million person-years. While it can affect individuals of various age groups, it is notably more prevalent among middle-aged individuals, with minimal to no reported cases in children.4Zhao, L., Chen, Y., & Wang, M. (2023). The Global Incidence Rate of Pemphigus Vulgaris: A Systematic Review and Meta-Analysis. Dermatology (Basel, Switzerland), 239(4), 514–522. https://doi.org/10.1159/000530121
Types of Pemphigus Vulgaris
There are two clinical subtypes of pemphigus vulgaris: pemphigus vegetans and pemphigus herpetiform.
Pemphigus Vegetans
This subtype is uncommon and mostly appears in the area of the armpits and groin where skin folds develop. Histological features of this variant show an increase in the number of cells in the upper layer of skin, called hyperkeratosis, and the last layer of skin develops cleft.5Becker, B. A., & Gaspari, A. A. (1993). Pemphigus vulgaris and vegetans. Dermatologic clinics, 11(3), 429–452.
Pemphigus Herpetiform
This clinical variant of pemphigus vulgaris stands out because of its unusual symptoms. People with this condition develop itchy rashes in the form of raised, patchy areas or blisters, often arranged in clusters or rings on their skin. Unlike many other skin conditions, Pemphigus herpetiformis usually spares the inside of the mouth and other mucous membranes.
When doctors examine affected skin under a microscope, they typically find a pattern called “eosinophilic spongiosis,” distinguishing this condition from others. Interestingly, there is usually no “acantholysis,” a term for skin cells breaking apart.
Causes of Pemphigus Vulgaris
The most common cause of pemphigus vulgaris is an autoimmune reaction. Firstly, cells of the skin layers, known as keratinocytes, are tied together with the help of a structure called desmosomes. However, when the body’s immune system recognizes skin cells as a foreign substance, it produces antibodies, primarily immunoglobulin type G. These antibodies target and harm the desmoglein 1 and desmoglein 3, protein components of desmosomes, leading to their destruction. As these desmosomes are compromised, their vital function in maintaining the cohesion of keratinocytes is disrupted. This disruption causes keratinocytes to separate from one another, creating voids. Furthermore, the infectious fluid fills the space previously occupied by keratinocytes, leading to skin blisters. This is a normal causative cycle of pemphigus vulgaris.
Risk Factors
Although the exact cause of the abnormal immune response in PV is unknown, some factors trigger the reaction of immunoglobulin type G and act as risk factors for pemphigus vulgaris.
These factors are intake of certain medications, like angiotensin-converting enzyme inhibitors used in patients of hypertension, Nonsteroidal anti-inflammatory drugs used in inflammatory conditions of the body, and cephalosporins for bacterial infection, presence of stressful environment, presence of infection and trauma in the body.6Malik, A. M., Tupchong, S., Huang, S., Are, A., Hsu, S., & Motaparthi, K. (2021). An Updated Review of Pemphigus Diseases. Medicina (Kaunas, Lithuania), 57(10), 1080. https://doi.org/10.3390/medicina57101080 Therefore, patients with pemphigus vulgaris should avoid stress, any physical trauma, and infectious exposure to overcome the symptoms of this disorder.
Clinical Signs & Symptoms of Pemphigus Vulgaris
The symptoms of pemphigus vulgaris appear at a specific time.
Cutaneous manifestation
- The first symptom is the appearance of a lesion on the mucous membrane. This lesion can last days or months before blistering. In some cases, patients have only one symptom: the appearance of a lesion.
- Next, this lesion is converted to thin membrane fluid-filled blisters. These blisters are painful and easily rupture, releasing fluid.
- The rupture of blisters leaves a sore and crusted skin behind. This crusted and vegetative skin appears red and tender.
- The sore skin of the mouth and skin acts as the bedrock for various bacterial and viral infections.
Oral manifestations
- The symptoms of oral pemphigus vulgaris appear as fluid-filled ulcers in the oral cavity. The presence of ulcers in the oral cavity makes patients unable to eat, swallow, and speak.7Batistella, E. Â., Sabino da Silva, R., Rivero, E. R. C., & Silva, C. A. B. (2021). Prevalence of oral mucosal lesions in patients with pemphigus vulgaris: A systematic review and meta-analysis. Journal of Oral Pathology & medicine: official publication of the International Association of Oral Pathologists and the American Academy of Oral Pathology, 50(8), 750–757. https://doi.org/10.1111/jop.13167
- Oral ulcers have irregular margins and an erythematous halo (Red borders). These ulcers usually appear on the side of the cheeks and the lower surface of the tongue.
- These ulcers burst easily, making it difficult for patients to digest and swallow food.
Diagnosis of Pemphigus Vulgaris
The blister pattern of pemphigus vulgaris mimics various viral infections. So, an accurate diagnosis is necessary to avoid medicine resistance in the body. Given below are the steps to achieve an accurate diagnosis:
History
A complete medical history with greater emphasis on the onset, intensity, number, and location of blisters on the skin. Any intake of medicine to treat symptoms should be asked.
General Physical Examination
During the physical examination, the clinician thoroughly assesses several aspects of the blisters. This evaluation includes examining the size of the blisters, their degree of redness, and the characteristics of their bases. It’s crucial to compare the appearance of the affected skin to that of normal skin to identify any significant differences. In cases of oral ulcers, patients should seek consultation with a dentist who can perform a meticulous examination of the oral cavity.
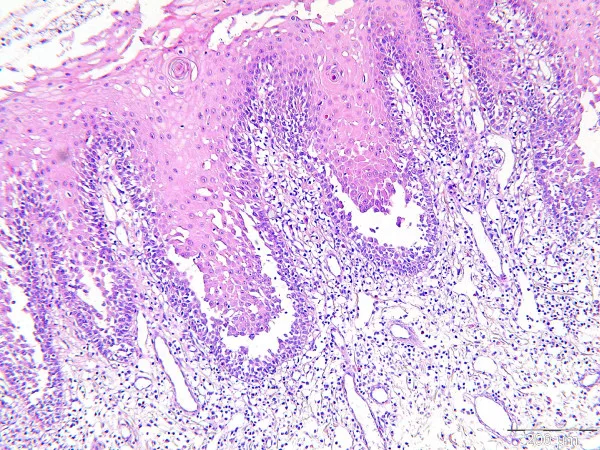
Biopsy
The diagnostic process often involves a biopsy, wherein a small sample is extracted from the affected area. Additionally, a sample of adjacent normal tissue is collected for clear differentiation. The biopsy results reveal distinctive features, such as separated keratinocytes with clefts, particularly in the basal or lower layer. Pemphigus Vulgaris (PV) typically presents a unique histological feature known as the ‘tombstone pattern.’ This pattern is characterized by the loss of adhesion between layers of skin cells above the basal layer and helps distinguish it from other conditions.
Direct Immunofluorescence
You should take the area around the lesion and undergo immunofluorescence staining to confirm the presence of immunoglobulin (Ig)G antibodies. Hence, this is one of the best confirmatory tests for pemphigus vulgaris.
Indirect immunofluorescence
In this test, we check the blood level of immunoglobulin (Ig)G antibodies to confirm the diagnosis.
Treatment of Pemphigus Vulgaris
There is no complete cure for pemphigus vulgaris. However, the intake of medicines and changes in lifestyle habits can help patients avoid all the painful symptoms.
Medication
Use of oral corticosteroids and topical corticosteroids can resolve the blister and reduce oral ulcers. Doctors may prescribe immunosuppressants to avoid unwanted reactions of the immune system on the body. Additionally, to avoid superficial infections, patients should be given antiviral and antibacterial drugs.8Yeh, S. W., Sami, N., & Ahmed, R. A. (2005). Treatment of pemphigus vulgaris: current and emerging options. American journal of clinical dermatology, 6(5), 327–342. https://doi.org/10.2165/00128071-200506050-00006
Plasmapheresis
Plasmapheresis or intravenous immunoglobulin may be necessary for individuals whose pemphigus vulgaris does not respond to other treatments. These intensive treatments involve replacing blood plasma and administering infusions of healthy immunoglobulin.9Johns Hopkins Medicine. Pemphigus vulgaris. Retrieved from https://www.hopkinsmedicine.org/health/conditions-and-diseases/pemphigus-vulgaris#:~:text=What%20causes%20pemphigus%20vulgaris%3F,a%20chemical%20or%20a%20drug.
Lifestyle Changes
- Patients should avoid all triggers, like certain medications or physical or mental stress.
- Start wearing soft clothes to prevent blisters from rupturing. To avoid pain, try covering the sore skin with a non-sticky bandage. Regularly clean the sore area with an antiseptic solution.
- In case of an oral infection, maintain meticulous oral hygiene with gentle brushing and mouthwashing. Use topical oral corticosteroids to relieve pain. Eat a soft diet to fulfill your nutrient requirements.
Pemphigus Vulgaris Vs. Bullous pemphigoid
The immune system normally fights infections, but in pemphigus and pemphigoid, the immune system forms antibodies against normal body structures in the skin, causing blisters.
The diagnosis of skin diseases needs to be accurate so that appropriate treatment can be given. There is a difference between pemphigus and pemphigoid.10Kayani, Mahaz, and Arif M. Aslam. “Bullous pemphigoid and pemphigus vulgaris.” bmj 357 (2017).
Pemphigus is characterized by shallow ulcers or fragile blisters that break open quickly.
Pemphigoid presents with stronger or “tense” blisters that don’t open easily. Those with pemphigoid are also more likely to have hot, red, and itchy hive spots.
| Pemphigus Vulgaris | Bullous pemphigoid | |
| Age | Usually 40 – 60 years. | Above 70 years. |
| Time Course | Chronic, relapse | Chronic, relapse |
| Symptoms | Painful | Itchy |
| Mucosal Involvement | Often seen | Only in 10-30% of cases |
| Blisters | These form within the epidermal layers and are often in the lowest section | These form beneath the epidermis |
| Bullae | Fragile, flaccid, and already ruptured. | Bullae tense |
| Antibodies | Autoantibodies against desmoglein 1 and 3. | Hemidesmosome antigens BP180 (Collage XVII) and BP230 |
| Nikolsky sign* | Positive | Negative |
| Histology | Tombstone appearance of the basal layer | Eosinophil infiltration |
| Direct Immunofluorescence | Net-like IgG | Linear IgG |
| Prognosis | Poor | Good |
*Nikolsky sign: This is a skin finding in which the top layer of skin slips away from the lower layers when rubbed.

In conclusion, pemphigus vulgaris (PV) is a rare but serious autoimmune disorder characterized by painful skin blistering and mucous membranes. Early diagnosis and comprehensive treatment are crucial for managing symptoms and preventing complications.
Refrences
- 1Porro, A. M., Seque, C. A., Ferreira, M. C. C., & Enokihara, M. M. S. E. S. (2019). Pemphigus vulgaris. Anais brasileiros de dermatologia, 94(3), 264–278. https://doi.org/10.1590/abd1806-4841.20199011
- 2Giannetti, L., Generali, L., & Bertoldi, C. (2018). Oral pemphigus. Giornale italiano di dermatologia e venereologia : organo ufficiale, Societa italiana di dermatologia e sifilografia, 153(3), 383–388. https://doi.org/10.23736/S0392-0488.18.05887-X
- 3Ingold, C. J., & Khan, M. A. B. (2023). Pemphigus Vulgaris. In StatPearls. StatPearls Publishing.
- 4Zhao, L., Chen, Y., & Wang, M. (2023). The Global Incidence Rate of Pemphigus Vulgaris: A Systematic Review and Meta-Analysis. Dermatology (Basel, Switzerland), 239(4), 514–522. https://doi.org/10.1159/000530121
- 5Becker, B. A., & Gaspari, A. A. (1993). Pemphigus vulgaris and vegetans. Dermatologic clinics, 11(3), 429–452.
- 6Malik, A. M., Tupchong, S., Huang, S., Are, A., Hsu, S., & Motaparthi, K. (2021). An Updated Review of Pemphigus Diseases. Medicina (Kaunas, Lithuania), 57(10), 1080. https://doi.org/10.3390/medicina57101080
- 7Batistella, E. Â., Sabino da Silva, R., Rivero, E. R. C., & Silva, C. A. B. (2021). Prevalence of oral mucosal lesions in patients with pemphigus vulgaris: A systematic review and meta-analysis. Journal of Oral Pathology & medicine: official publication of the International Association of Oral Pathologists and the American Academy of Oral Pathology, 50(8), 750–757. https://doi.org/10.1111/jop.13167
- 8Yeh, S. W., Sami, N., & Ahmed, R. A. (2005). Treatment of pemphigus vulgaris: current and emerging options. American journal of clinical dermatology, 6(5), 327–342. https://doi.org/10.2165/00128071-200506050-00006
- 9Johns Hopkins Medicine. Pemphigus vulgaris. Retrieved from https://www.hopkinsmedicine.org/health/conditions-and-diseases/pemphigus-vulgaris#:~:text=What%20causes%20pemphigus%20vulgaris%3F,a%20chemical%20or%20a%20drug.
- 10Kayani, Mahaz, and Arif M. Aslam. “Bullous pemphigoid and pemphigus vulgaris.” bmj 357 (2017).