Also known as a gingival graft, gum grafting is a periodontal (dental) surgery procedure done to treat loss of surrounding tissues and exposed teeth roots caused by gum recession. This type of surgery aids in covering exposed root surfaces and adding volume to the gum line. It is one of the most common periodontal surgical procedures performed in US dental clinics. Modified gingival graft procedures have a high success rate (above 90%).1Fatani, B., Alshalawi, H., Fatani, A., Almuqrin, R., Aburaisi, M. S., & Awartani, F. (2024). Modifications in the Free Gingival Graft Technique: A Systematic Review. Cureus, 16(4). Recovery from surgery generally takes a couple of weeks. Timely diagnosis and gum surgery reduce the risk of gum disease progression.
Indications for Gum Grafting
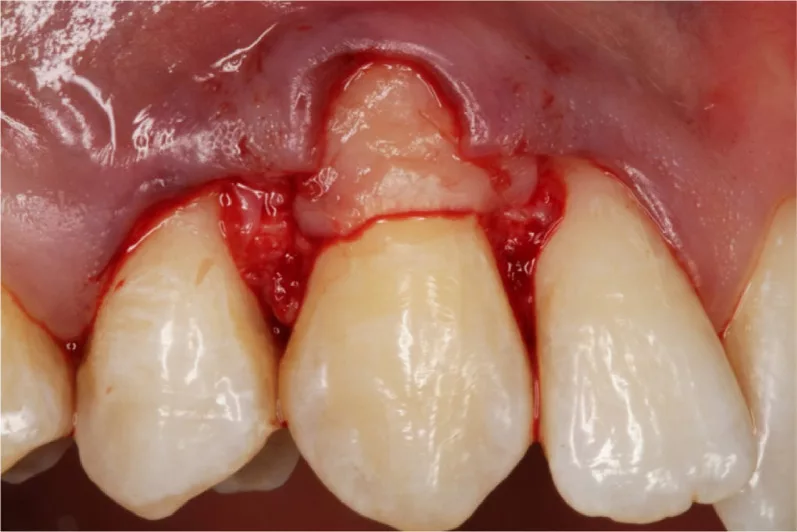
The most common reason for which people seek gum grafting is gum recession. It is a common dental problem that manifests as apical migration of the gingival margins, leading to exposure of roots. Improper brushing techniques, poor oral hygiene (deposition of tartar), and certain lifestyle habits (like smoking) contribute to gum recession.2Niemczyk, W., Niemczyk, S., Prokurat, M., Grudnik, K., Migas, M., Wągrowska, K., … & Kasperczyk, J. (2024). Etiology of gingival recession–a literature review. Wiadomosci Lekarskie (Warsaw, Poland: 1960), 77(5), 1080-1085.3 Niemi ML, Sandholm L, Ainamo J. Frequency of gingival lesions after standardized brushing as related to stiffness of toothbrush and abrasiveness of dentifrice. J Clin Periodontol. 1984;11(4):254–61. However, some people are prone to gum thinning due to genetic predisposition. Brushing aggressively can also lead to tooth abrasions and gingival recession.
Exposed roots can cause multiple problems. Generally, patients complain of hot/cold hypersensitivity and there is also an increased risk of tooth decay. There is also exacerbated loss of surrounding tissues (bone and the rest of periodontium). Therefore, it is important to get your gum grafting done as soon as possible.
Types of Gum Grafts
A periodontist (gum specialist) decides which type of graft will be best suitable for your condition. The most common types of gingival grafts include:
Free Gingival Graft (FGG)
Patients suffering from gum thinning mostly receive a free gingival graft to prevent further recession. Your doctor will obtain a free graft by removing a small piece of gum tissue from the roof of your mouth (palate). The surgeon then stitches the flap to the area lacking gingiva. Nowadays, periodontists perform a modified type of free gingival graft, i.e., gingival unit graft (GUG).
In GUG, the harvested graft (from the palate) contains some interdental tissue as well as the marginal gingiva. Therefore, the vascular supply of the graft is richer. This leads to results superior to the conventional free gingival graft, especially in the anterior mandibular gum recession cases.4Agrawal, P., Katti, N., Mohanty, D., Pradhan, S. S., Raj, S. C., Satyarup, D., … & Srivani, P. (2022). Treatment of Localized Gingival Recession Using Gingival Unit Grafts: An 18-month Follow-up Study. The Journal of Contemporary Dental Practice, 23(1), 49-55.
Connective Tissue Graft
A connective tissue graft is the most common type of periodontal graft. The surgeon makes an incision in the palate but instead of removing the whole gum tissue, he spares the top layer and removes connective tissue from underneath. He then stitches the top layer of the palatal mucosa back and adds the graft to the affected region.
Lateral (Pedicle)
In this type of flap, tissue is taken from the region neighboring the gum recession. Thus, it is more of a pedicular extension of the adjacent tissue which covers the exposed roots. As no blood flow is cut off in this flap (the flap remains attached from the base throughout), the results and tissue acceptance are best. Periodontists claim to have better results when pairing a periosteal pedicle flap with a coronally advanced flap.5Mahajan, A., Goyal, L., Asi, K. S., Walhe, M. S., & Chandel, N. (2023). Clinical effectiveness of periosteal pedicle graft for the management of gingival recession defects—a systematic review and meta-analysis. Evidence-Based Dentistry, 24(2), 93-94.
However, it requires robust gum tissue in the region around gum recession, which isn’t available in most cases.
Benefits Of Gum Grafting
A successful gum grafting procedure has the following therapeutic benefits:
- Improved aesthetics: Esthetic analyses reveal that free gingival grafts significantly improve a patient’s appearance and provide acceptable aesthetic outcomes.6Naziker, Y., & Ertugrul, A. S. (2023). Aesthetic evaluation of free gingival graft applied by partial de-epithelialization and free gingival graft applied by conventional method: a randomized controlled clinical study. Clinical Oral Investigations, 27(7), 4029-4038.
- Decreased root sensitivity: When performed properly, gum grafting surgeries can reduce root hypersensitivity and improve oral health.
- Increased keratinized gingiva: Keratinized gingiva is the strongest type of gum and is resistant to wear and tear. Grafts can help improve the amount of keratinized gingiva in the recipient site.
Gum Grafting Procedure
After careful analysis of the gum recession and the quality of gingiva at the donor site, a periodontist will give you an appointment for gum grafting surgery. The sequence of events for the surgery is as follows:
Administration of Local Anesthesia:
The first step is to numb the gums of the donor and recipient sites. The majority of periodontists use local anesthesia for this purpose (general anesthesia may also be used but is generally avoided). Conscious sedation is a new way in which the doctor sedates the patient using nitrous oxide gas.
Preparation of the Site:
After anesthesia sets in, the surgeon makes an incision at the recipient site. He thoroughly cleans and debrides the site after making a small flap in your gums.
Taking the Graft:
In the next step, the surgeon cuts across the palate (roof of the mouth) and removes a flap (FGG, GUG, or connective tissue graft). He then sutures the donor site back or places a periodontal dressing (in case of a free gingival graft).
Placing the Graft & Stitching it:
The periodontist then places the gum graft over the receded area to cover the exposed roots. The graft is accurately positioned and sutured in place. Most of the time, surgeons use self-resorbable sutures. If not, then you need to get them removed at the follow-up visit.
Removing the Gauze:
Your doctor will probably place a gauze dressing over the surgical site during the surgery. You can remove the gauze 30 minutes after the procedure is completed.
How long does it take to complete?
The complete procedure usually takes about an hour. The duration of the surgery can increase if multiple grafts are required.
Is the surgery painful?
No, local anesthesia numbs the gums and teeth so most people do not feel a thing during the procedure. Even after the surgery, you might just feel soreness but that is also managed well with medications.
Gum Grafting Recovery
Recovery from a gum grafting procedure usually takes one to two weeks, but certain factors can increase the recovery time.

A major obstacle in quick healing after periodontal surgery is smoking. Studies reveal that smokers have a slow healing rate after root coverage procedures.7Kanmaz, M. G., Kanmaz, B., & Buduneli, N. (2022). Gingival recession and root coverage outcomes in smokers. Population Medicine, 4(September), 1-12. Another narrative review concluded that in addition to delayed healing, smokers have a high risk of recurrence and treatment failure.8Kanmaz, M., Kanmaz, B., & Buduneli, N. (2021). Periodontal treatment outcomes in smokers: A narrative review. Tobacco-induced diseases, 19. Other factors that can delay periodontal healing include comorbidities like diabetes.
Gum Grafting Healing Stages
Healing of the grafted site occurs in stages, which are discussed below:
Hemostasis
Within minutes of graft connection with the receded gums, platelets rush to the injury site and stick at the wound openings. They promote the deposition of fibrin (a protein responsible for clotting). Activation of fibrin protein and clotting factors (by platelets) leads to the formation of a mesh that clogs the blood vessels and stops bleeding (hemostasis). The pale white graft is pale/white colored at this time due to a lack of vascular (blood) supply. The sides of the graft are covered with fibrin mesh.
Inflammation
The next day (after surgery) marks the initiation of the inflammatory stage. During this stage, you will notice redness in your gums that is indicative of blood (and inflammatory cells) build-up in the region.
An important event of this stage is necrosis (death) and flaking off of the graft’s top layer. If you notice peeling off of a white-gray layer from the graft, don’t worry, it’s completely normal and does not indicate failure of the graft. In fact, it is a natural process (phagocytosis) to remove any dead cells to ensure optimal gingival health.
Angiogenesis (growth of new blood vessels) sets in within 3 to 4 days. The growth of new blood vessels into the gum graft lays the foundation for tissue growth.
Cell Proliferation
After a week, the grafted gingiva starts to connect with the surrounding gingiva. The cells of the gum graft proliferate and fuse with the neighboring gingiva. There is an abundance of fibroblasts that promote connective tissue production. You can expect to see a seamless fusion of the graft by the 14th day.

Tissue Maturation
Fusion completes by the end of 2nd week. However, the process of healing continues for up to a year (or more even). The tissues continue to be matured and remodeled to cater to the changes.
Complications of Gum Grafting
Gum grafting is a safe procedure and complications are rare. However, you may experience issues like:
- Excessive bleeding (from surgical site)
- Infection
- Gum graft failure (rejection of the transplanted tissue by the recipient)
You must inform your dentist of any side effects. Sometimes, complications arise due to improper placement or adaptation of the graft site. This requires redoing the procedure.
Alternatives to Gum Grafting
Bonding Vs Gum Grafting
Composite bonding is an alternative to gum grafting that can alleviate symptoms of root exposure. In this procedure, the dentist covers the exposed root surfaces with composite resin. This results in reductions in hypersensitivity and aesthetic improvement. However, this is a short-term and affordable treatment option. For permanent correction, gum grafting is the treatment of choice.
Gum Grafting After Care
After the completion of the process, you are free to go home but have to follow post-op instructions. On the first day, you should eat cold and soft foods such as:
- Yogurt
- Eggs
- Icecream
- Pudding
- Smoothies
Take ample rest and avoid carrying out strenuous activities. You need to keep the surgical site clean but avoid flossing/brushing. Your dentist may advise you an antimicrobial mouthwash. Use it daily to keep surgical site infections at bay. Continue taking the medications (painkillers, etc.) prescribed by your doctor.
You can resume brushing/flossing and eating harder foods when your dentist allows. It usually takes a couple of weeks to return to normal routine.
Final Word
Gingival or gum grafting is a surgical procedure done to cover teeth roots exposed by gum recession. It is a successful procedure performed by a periodontist. A gum grafting procedure alleviates symptoms of cementum (root) exposure i.e., hypersensitivity, increased risk of caries, and bone loss.
After anesthetizing the donor (roof of the mouth) and the recipient area, the surgeon takes a small piece of gum tissue. Types of gum grafts include free gingival graft (full flap), gingival unit graft (modified FGF), connective tissue graft (underlying connective tissue), and pedicle graft (flap from neighboring tissues). Recovery usually takes a couple of weeks. During this time, you should avoid brushing/flossing the surgical area, avoid strenuous exercises, take rest and soft/cold foods.
Refrences
- 1Fatani, B., Alshalawi, H., Fatani, A., Almuqrin, R., Aburaisi, M. S., & Awartani, F. (2024). Modifications in the Free Gingival Graft Technique: A Systematic Review. Cureus, 16(4).
- 2Niemczyk, W., Niemczyk, S., Prokurat, M., Grudnik, K., Migas, M., Wągrowska, K., … & Kasperczyk, J. (2024). Etiology of gingival recession–a literature review. Wiadomosci Lekarskie (Warsaw, Poland: 1960), 77(5), 1080-1085.
- 3Niemi ML, Sandholm L, Ainamo J. Frequency of gingival lesions after standardized brushing as related to stiffness of toothbrush and abrasiveness of dentifrice. J Clin Periodontol. 1984;11(4):254–61.
- 4Agrawal, P., Katti, N., Mohanty, D., Pradhan, S. S., Raj, S. C., Satyarup, D., … & Srivani, P. (2022). Treatment of Localized Gingival Recession Using Gingival Unit Grafts: An 18-month Follow-up Study. The Journal of Contemporary Dental Practice, 23(1), 49-55.
- 5Mahajan, A., Goyal, L., Asi, K. S., Walhe, M. S., & Chandel, N. (2023). Clinical effectiveness of periosteal pedicle graft for the management of gingival recession defects—a systematic review and meta-analysis. Evidence-Based Dentistry, 24(2), 93-94.
- 6Naziker, Y., & Ertugrul, A. S. (2023). Aesthetic evaluation of free gingival graft applied by partial de-epithelialization and free gingival graft applied by conventional method: a randomized controlled clinical study. Clinical Oral Investigations, 27(7), 4029-4038.
- 7Kanmaz, M. G., Kanmaz, B., & Buduneli, N. (2022). Gingival recession and root coverage outcomes in smokers. Population Medicine, 4(September), 1-12.
- 8Kanmaz, M., Kanmaz, B., & Buduneli, N. (2021). Periodontal treatment outcomes in smokers: A narrative review. Tobacco-induced diseases, 19.





