On average, a human’s heart beats 60 to 100 times per minute. But when the heart starts to beat more rapidly than the normal limit, it causes abnormal heart rhythm, known as Supraventricular Tachycardia (SVT). Although sinus tachycardia is typically a normal response to stress or physical activity, it raises concerns when it happens while the body is at rest.
In most cases, SVT is not a serious ailment, but it requires prompt management to prevent further cardiac problems.
What is SVT?
Supraventricular Tachycardia (SVT) is a type of abnormal heart rhythm characterized by a rapid heartbeat originating from above the ventricles, the lower chambers of the heart. This condition often causes the heart to beat faster than the normal range of 60 to 100 beats per minute.1KOSSMANN CE. The normal electrocardiogram. Circulation. 1953 Dec;8(6):920-36. In children, heart rate varies depending on age but is generally higher than the resting rate in adults. It typically ranges from about 100 to 150 beats per minute in infants and gradually decreases over the first six years of life.2Fleming S, Thompson M, Stevens R, Heneghan C, Plüddemann A, Maconochie I, Tarassenko L, Mant D. Normal ranges of heart rate and respiratory rate in children from birth to 18 years of age: a systematic review of observational studies. Lancet. 2011 Mar 19;377(9770):1011-8. While SVT is typically not life-threatening, prompt management is necessary to prevent potential complications and ensure the heart functions properly.
The term Supraventricular Tachycardia is taken from Latin, where supraventricular indicates “above the ventricles,” which are the inferior two chambers of the heart, whereas Tachycardia indicates “faster heart rate.”
Pathophysiology of Supraventricular Tachycardia
The human heart relies on an electrical circuit originating in the sinoatrial (SA) node.3Kashou AH, Basit H, Chhabra L. Physiology, Sinoatrial Node. [Updated 2022 Oct 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459238/ This electrical pathway typically travels through the upper chambers (atria) to the lower chambers (ventricles), coordinating the contraction and relaxation of all four chambers to facilitate functional heartbeats.
However, in Supraventricular Tachycardia (SVT), the heart’s conduction system experiences disruptions due to faulty electrical pathways in the atria. This results in rapid heartbeats originating from the upper chambers, or atria. When the atria receive electrical impulses prematurely, they contract prematurely as well. This premature contraction interferes with the normal electrical activity originating from the SA node, leading to an abnormal and accelerated heart rate that can reach speeds of 180 to 220 beats per minute (bpm).4Kotadia, I. D., Williams, S. E., & O’Neill, M. (2020). Supraventricular tachycardia: An overview of diagnosis and management. Clinical Medicine (London, England), 20(1), 43–47.
Types of SVT
Supraventricular tachycardia has three main types which include:
Atrioventricular Nodal Reentrant Tachycardia
It is the most prevalent type of SVT rhythm in which an extra electrical pathway is induced in the heart. Later, this electrical impulse circles around in the atria instead of traveling into the ventricles, causing an increased heartbeat.
Atrioventricular Reciprocating Tachycardia
This type of SVT rhythm occurs when electrical impulses keep moving around the atria and ventricles due to the presence of accessory pathways (AP). It causes the reentry of electrical signals and rapid heartbeats.
People with Wolff-Parkinson-White syndrome tend to have extra electrical pathways, which can be lethal. This condition is genetic and can be diagnosed with a positive family history.
Atrial Tachycardia
Atrial Tachycardia occurs when a short circuit generates an abnormal signal in the right or left atrium.
The aforementioned supraventricular tachycardia episode lasts only a few seconds or hours. However, when individuals experience a prolonged and regular episode of SVT, it falls under the category of paroxysmal supraventricular tachycardia.
Some rare types of SVT include:
- Sinus tachycardia
- Non-paroxysmal junctional tachycardia (NPJT)
- Junctional ectopic tachycardia (JET)
- Sinus nodal reentrant tachycardia (SNRT)
- Inappropriate sinus tachycardia (IST)
- Multifocal atrial tachycardia (MAT)
What Causes SVT?
Physiologically, the heart tends to pump quicker after exercise or during periods of anxiety. On the contrary, supraventricular tachycardia arises once there is an abnormality with cardiac nervous signals that allows it to beat faster under normal circumstances.
Studies suggest5Porter MJ, Morton JB, Denman R, Lin AC, Tierney S, Santucci PA, Cai JJ, Madsen N, Wilber DJ. Influence of age and gender on the mechanism of supraventricular tachycardia. Heart Rhythm. 2004 Oct;1(4):393-6. doi: 10.1016/j.hrthm.2004.05.007. PMID: 15851189./ that the exact cause of SVT is still unknown. Although pathology often shows its initial symptoms during adolescence or early 20s.
Moreover, people with SVT have had abnormal cardiac electrical activity since birth. However, scar tissues left by any previous heart surgery can trigger faulty impulses, leading to supraventricular tachycardia.
Some common risk factors are:
- Smoking
- Alcohol dependence
- Pregnancy
- Prevalence of Thyroid or Chronic Lung diseases
- High caffeine consumption
- Intake of certain medicines, including decongestants, asthma relieving pills, and herbal weight loss remedies
- Ingestion of certain recreational drugs, such as methamphetamine or cocaine
- A stressful or tiring routine
- Pre-existing heart diseases like coronary artery disease
- Obstructive sleep apnea
- Thyroid disorders
Symptoms of Supraventricular Tachycardia
The symptoms of supraventricular tachycardia (SVT) vary from individual to individual. However, the most prominent symptom is a fastening heart rate of over 100 beats per minute, which can persist for a few minutes to a few hours.
The episodes of SVT are intermittent. They come and go with the phases of a normal heartbeat in between. Additionally, in a few individuals, SVT can be asymptomatic.
Some common supraventricular tachycardia symptoms are as follows:
- Fastening heart rate
- Chest pain
- Shortness of breath
- Fluttering in the chest, known as palpitations
- Pounding pulses in the neck
- Malaise and fatigue
- Feeling dizzy
- Regular bouts of sweating
- Frequent fainting (syncope)
Although it is difficult to find the signs and symptoms of SVT in young children and infants, healthcare professionals look for complaints of rapid pulse, reduced appetite, pale skin, and frequent sweating in children to identify SVT.
If you experience any of the aforementioned symptoms, get your SVT screening done immediately to receive timely treatment.
How To Diagnose SVT?
When diagnosing Supraventricular arrhythmias, the healthcare professional might ask certain questions about your symptoms. These questions include how and when the symptoms began, their longevity, and whether they show gradually or suddenly.6Wang, K. (2013). Supraventricular Tachycardia (SVT). In Atlas of Electrocardiography (pp. 120–120). Jaypee Brothers Medical Publishers (P) Ltd.
In addition, the patient should notify the doctor if symptoms such as lightheadedness, breathlessness, and pounding pulse occur during exercise or if the symptoms worsen with caffeine or under stressful situations.
Also, the doctor may ask about the prevalence of cardiac diseases in your family. Positive family history increases the risk of individuals to develop supraventricular tachycardia. Answering these questions can assist in diagnosing supraventricular tachycardia and treating it accordingly.
Furthermore, healthcare providers listen to heart and chest sounds using a stethoscope to detect abnormalities in a heartbeat.
The doctor may also ask to get these tests done to identify supraventricular arrhythmias:
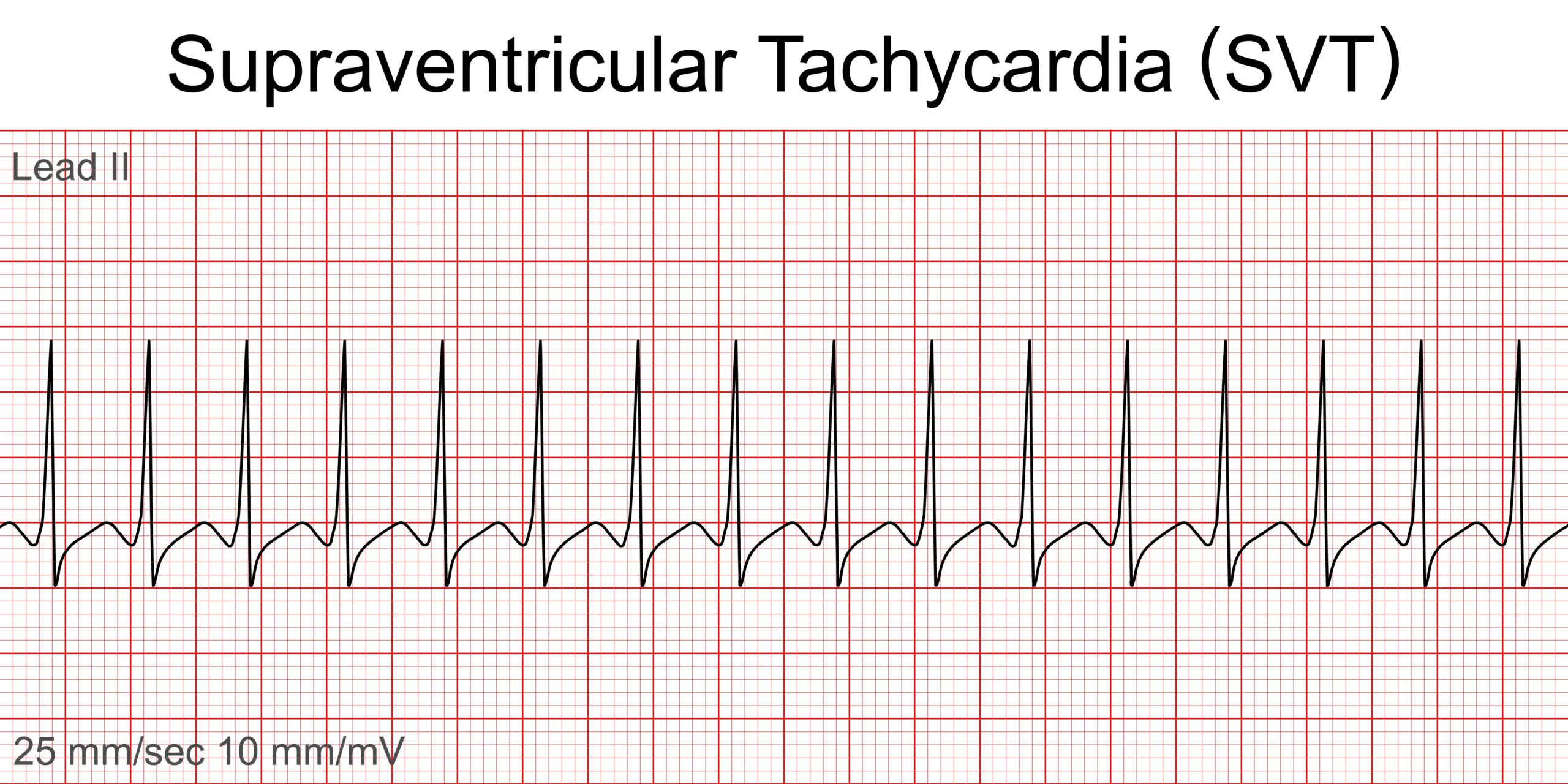
Electrocardiogram (ECG or EKG)
It is a key diagnostic test of SVT that records the heart rate and rhythm pattern. In supraventricular tachycardia, the ECG shows a narrow QRS complex with less than 100 ms and a heart rate of over 180 pm. Occasionally, P waves aren’t present on ECG due to faulty atrial contraction.7Bibas L, Levi M, Essebag V. Diagnosis and management of supraventricular tachycardias. CMAJ. 2016 Dec 6;188(17-18):E466-E473. doi: 10.1503/cmaj.160079. Epub 2016 Oct 24. PMID: 27777258; PMCID: PMC5135523.
Heart Monitor
It records the heart’s electrical signal for a longer duration, which helps the provider confirm the SVT diagnosis.
Treatment of Supraventricular Tachycardia
Mostly, the episodes of supraventricular tachycardia go on their own. But in certain cases, if SVT is left untreated, it causes severe heart problems.
Thereby, to treat SVT, the doctor may prescribe these medications to get the heart rate under control:8Brugada, J., Katritsis, D. G., Arbelo, E., Arribas, F., Bax, J. J., Blomström-Lundqvist, C., Calkins, H., Corrado, D., Deftereos, S. G., Diller, G.-P., Gomez-Doblas, J. J., Gorenek, B., Grace, A., Ho, S. Y., Kaski, J.-C., Kuck, K.-H., Lambiase, P. D., Sacher, F., Sarquella-Brugada, G., … ESC Scientific Document Group. (2020). 2019 ESC Guidelines for the Management of Patients with Supraventricular tachycardiaThe Task Force for the Management of Patients with Supraventricular Tachycardia of the European Society of Cardiology (ESC). European Heart Journal, 41(5), 655–720.
- Beta-blockers
- Calcium channel blockers
- Potassium channel blockers
- Digoxin
- Atropine
- Adenosine
If the medications are unable to manage episodes of supraventricular tachycardia, catheter ablation surgery is performed. In this procedure, the surgeon ablates faulty electrical pathways in the heart, which cures supraventricular arrhythmias in 95% of cases 9Upadhyay S, Marie Valente A, Triedman JK, Walsh EP. Catheter ablation for atrioventricular nodal reentrant tachycardia in patients with congenital heart disease. Heart Rhythm. 2016 Jun;13(6):1228-37. doi: 10.1016/j.hrthm.2016.01.020. Epub 2016 Jan 21. PMID: 26804568..
Conclusion
Is SVT dangerous? Certainly not if proper precautionary measures have been taken. However, once the supraventricular tachycardia symptoms get worse, such as fastening heartbeats persisting for hours, fainting, breathlessness, and chest pain, prompt medical attention is the way to go.
Refrences
- 1KOSSMANN CE. The normal electrocardiogram. Circulation. 1953 Dec;8(6):920-36.
- 2Fleming S, Thompson M, Stevens R, Heneghan C, Plüddemann A, Maconochie I, Tarassenko L, Mant D. Normal ranges of heart rate and respiratory rate in children from birth to 18 years of age: a systematic review of observational studies. Lancet. 2011 Mar 19;377(9770):1011-8.
- 3Kashou AH, Basit H, Chhabra L. Physiology, Sinoatrial Node. [Updated 2022 Oct 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459238/
- 4Kotadia, I. D., Williams, S. E., & O’Neill, M. (2020). Supraventricular tachycardia: An overview of diagnosis and management. Clinical Medicine (London, England), 20(1), 43–47.
- 5Porter MJ, Morton JB, Denman R, Lin AC, Tierney S, Santucci PA, Cai JJ, Madsen N, Wilber DJ. Influence of age and gender on the mechanism of supraventricular tachycardia. Heart Rhythm. 2004 Oct;1(4):393-6. doi: 10.1016/j.hrthm.2004.05.007. PMID: 15851189./
- 6Wang, K. (2013). Supraventricular Tachycardia (SVT). In Atlas of Electrocardiography (pp. 120–120). Jaypee Brothers Medical Publishers (P) Ltd.
- 7Bibas L, Levi M, Essebag V. Diagnosis and management of supraventricular tachycardias. CMAJ. 2016 Dec 6;188(17-18):E466-E473. doi: 10.1503/cmaj.160079. Epub 2016 Oct 24. PMID: 27777258; PMCID: PMC5135523.
- 8Brugada, J., Katritsis, D. G., Arbelo, E., Arribas, F., Bax, J. J., Blomström-Lundqvist, C., Calkins, H., Corrado, D., Deftereos, S. G., Diller, G.-P., Gomez-Doblas, J. J., Gorenek, B., Grace, A., Ho, S. Y., Kaski, J.-C., Kuck, K.-H., Lambiase, P. D., Sacher, F., Sarquella-Brugada, G., … ESC Scientific Document Group. (2020). 2019 ESC Guidelines for the Management of Patients with Supraventricular tachycardiaThe Task Force for the Management of Patients with Supraventricular Tachycardia of the European Society of Cardiology (ESC). European Heart Journal, 41(5), 655–720.
- 9Upadhyay S, Marie Valente A, Triedman JK, Walsh EP. Catheter ablation for atrioventricular nodal reentrant tachycardia in patients with congenital heart disease. Heart Rhythm. 2016 Jun;13(6):1228-37. doi: 10.1016/j.hrthm.2016.01.020. Epub 2016 Jan 21. PMID: 26804568.