Air embolism, also known as gas embolism, is a complication that occurs when air bubbles enter the arterial or venous system. It is a serious complication as it leads to adverse effects. Symptoms of the patient range from mild to severe depending upon the volume of air entering the body. Prompt management can lead to better outcomes.
What is Air Embolism?
Air embolism is a rare but serious medical condition that occurs when air bubbles enter the blood vessels, either the arterial or venous system. This can happen during medical procedures involving the insertion of instruments into arteries or veins, such as central line placements or surgical interventions. Other causes include penetrating or blunt trauma, decompression sickness (in divers), and complications during childbirth.
The air bubbles can obstruct blood flow within the vessels, potentially traveling to critical organs such as the lungs, heart, or brain. This obstruction can lead to reduced blood flow, tissue ischemia, and, in severe cases, life-threatening complications or death. 1Gordy, S., & Rowell, S. (2013). Vascular air embolism. International journal of critical illness and injury science, 3(1), 73–76. https://doi.org/10.4103/2229-5151.109428
The Pathophysiology of Air Embolism
Venous air embolism (VAE) is more common than arterial one. The basic pathophysiology of VAE is a direct connection between the venous system and the air. Another factor that plays a role in developing this embolism is a pressure gradient that helps to push air into the circulation.
Factors Influencing Outcomes
Several factors influence the severity of a venous air embolism:
- Volume of Air: The body typically absorbs Small volumes of air without causing harm. However, volumes exceeding 5 mL/kg can lead to significant complications. Even smaller volumes, such as 0.5 mL of air in the coronary arteries or cerebral circulation, can cause life-threatening conditions like ventricular fibrillation or stroke.
- Rate of Air Entry: Rapid entry of air into the venous system can overwhelm compensatory mechanisms, leading to acute symptoms.
- Patient Position: Certain positions, such as head-down (Trendelenburg), can exacerbate the condition by increasing the likelihood of air traveling to critical regions like the pulmonary circulation or brain.
When large volumes of air enter the venous system with rapid force, it increases the pulmonary pressure. The increase in pulmonary pressure makes it difficult for the right heart to pump blood, leading to a decrease in cardiac output. People with this condition collapse due to a sudden decrease in cardiac output. Moreover, a large volume of air in the pulmonary venous system also causes severe endothelial damage. Injury to the vasculature also causes free radical formation, further deteriorating the symptoms and causing pulmonary edema.2Marsh, P. L., Moore, E. E., Moore, H. B., Bunch, C. M., Aboukhaled, M., Condon, S. M., 2nd, Al-Fadhl, M. D., Thomas, S. J., Larson, J. R., Bower, C. W., Miller, C. B., Pearson, M. L., Twilling, C. L., Reser, D. W., Kim, G. S., Troyer, B. M., Yeager, D., Thomas, S. G., Srikureja, D. P., Patel, S. S., … Walsh, M. M. (2023). Iatrogenic air embolism: pathoanatomy, thromboinflammation, endotheliopathy, and therapies. Frontiers in immunology, 14, 1230049. https://doi.org/10.3389/fimmu.2023.1230049
What are the Causes of Air Embolism?
There are several causes, but iatrogenic is the most common one.
Some important ones are:
Surgical Procedures:
Neurosurgical procedures are particularly associated with air embolism. The risk varies based on the patient’s position during surgery. It has been estimated that patients having neurosurgical procedures in a prone position have a 10% chance of developing this complication. In contrast, in procedures where patients have to be in a sitting position, such as posterior cranial fossa surgeries, the incidence of this condition increases to 80%.
Other surgical procedures such as craniofacial surgery, vascular procedures, hip replacement, and thoracotomy can also cause entrapment of air, resulting in air embolism.3Ji, J., Tian, Y., Chen, L., & Li, B. (2020). Intraoperative VAE in the non-cardiac surgery role of perioperative echocardiography in a case series report. Annals of translational medicine, 8(12), 798. https://doi.org/10.21037/atm-20-497
Gynecological Procedures & Laparoscopy:
Gynecological procedures commonly are not considered as a risk factor for this complication. However, they do have a risk of almost 50% of developing venous air embolism. Cesarean deliveries in which the uterus is externalized for observation or surgery have higher chances of developing VAE.
Insufflation of gas during laparoscopy is not a major risk of VAE, but if there is a formation of abnormal venous channels, there is a chance of it.4Lowenwirt, I. P., Chi, D. S., & Handwerker, S. M. (1994). Nonfatal venous air embolism during cesarean section: a case report and review of the literature. Obstetrical & gynecological survey, 49(1), 72–76. https://doi.org/10.1097/00006254-199401000-00028
Central Venous Catheterization:
Central venous catheterization, such as central lines, pulmonary catheters, and hemodialysis catheters, is a major and life-threatening cause. Detachment of the catheter, dysfunctional catheter, deep inspiration during insertion, and already present hypovolemia contribute to embolism. Moreover, an upright position of the patient during insertion increases the risk of air embolism. The incidence of this condition due to central venous catheterization is 1 in 47 to 1 in 3000.
Mechanical Infusion:
Mechanical infusion is another significant cause of air embolism. Many procedures in the medical field use insufflation (blowing something into the body cavity), such as laparoscopy, CO2 hysteroscopy, and some arthroscopic and urethral procedures. The use of IV contrast agents for CT scans, angiography, or cardiac ablation is also associated with the life-threatening development of this complication.
Positive Pressure Ventilation:
Positive pressure ventilation uses either a mask or a ventilator to help severely ill patients breathe, and it makes them vulnerable to developing barotrauma, eventually causing air embolism. Air enters into the circulation when positive pressure is high, and it ruptures the alveoli.
Scuba divers can also develop venous air embolism due to over-distension of alveoli.5Kane, G., Hewins, B., & Grannis, F. W., Jr (1988). Massive air embolism in an adult following positive pressure ventilation. Chest, 93(4), 874–876. https://doi.org/10.1378/chest.93.4.874
How common is Air Embolism?
Venous air embolism has an incidence of almost 0.13% due to central venous catheter procedures, and the frequency ranges from 1 in 47 to 1 in 3000. The incidence of air embolism during neurosurgical interventions is 10-80%. Almost 4-14% of cases of severe lung trauma also develop venous air embolism.6Alrasheedi, S. M., Alhumaidan, L. S., Alkhathami, A. A., & Alhati, M. (2023). Incidental Finding of Venous Air Embolism: A Case Report. Cureus, 15(1), e33896. https://doi.org/10.7759/cureus.33896
Signs & Symptoms of Air Embolism
Symptoms of air embolism vary from person to person depending on the position of entry of the air bubble, the amount of air, and the position of the patient at the time of the incident. Initial symptoms of venous air embolism nearly resemble the symptoms of cardiac, pulmonary, and neurological origin. That’s why it is essential to do a proper examination before declaring it as an embolism.
Some of the nonspecific symptoms of air embolism are:
- Shortness of breath with cough
- Tachypnea (increased heart rate )
- Vertigo and dizziness
- Gasping
- Nausea and vomiting
- Headache and seizures
- Syncope (fainting)
- Slurred speech and blurred vision due to dizziness
- Anxiety
Air bubbles in venous gas embolisms that form due to any cause can reach the pulmonary, cardiac, or neurological systems. System-related signs and symptoms vary in every patient. It is better to rule out every disease of that specific system before doing any treatment for air embolism.7Yeung, E., Adeboye, A., Granet, P., & Casos, S. (2021). Rare pathology in a trauma patient: air embolism following peripheral intravenous access. BMJ case reports 14(1), e240428. https://doi.org/10.1136/bcr-2020-240428
Pulmonary Findings:
When an air bubble enters the pulmonary circulation, it produces abnormal chest sounds such as rales, wheezing, and hemoptysis. Obstruction in pulmonary circulation leads to decreased arterial oxygen saturation causing cyanosis (change of body color to blue-purple) as well as increasing the carbon dioxide saturation in the blood.8Lanfranco, J., Romero Legro, I., Freire, A. X., Nearing, K., & Ratnakant, S. (2017). Pulmonary Air Embolism: An Infrequent Complication in the Radiology Suite. The American journal of case reports, 18, 80–84. https://doi.org/10.12659/ajcr.901098
Neurological & Eye Signs:
Air bubbles may enter into your neurological system and produce symptoms like:
- Altered mental status
- Seizures
- Weakness or paralysis
- Collapse
- Coma and death
Sometimes, air bubbles enter into the retinal vessels and the fundoscopic examination helps to visualize them.
Cardiovascular Signs:
When the cardiovascular system gets involved in venous air embolism, the patients present with myocardial ischemia due to obstruction of blood to the heart. They may also show signs like arrhythmias, “Mill-wheel murmurs ” (a machinery murmur over the precordium), and hypotension. ECG findings would show nonspecific ST-segment and T-wave changes. Some patients have increased jugular venous pressure as well as central venous pressure. When symptoms become severe, the patient collapses and dies.9Rahman, Z. U., Murtaza, G., Pourmorteza, M., El Minaoui, W. K., Sethi, P., Mamdouhi, P., & Paul, T. (2016). Cardiac Arrest as a Consequence of Air Embolism: A Case Report and Literature Review. Case reports in medicine, 2016, 8236845. https://doi.org/10.1155/2016/8236845
How to diagnose Air Embolism?
Signs and symptoms of this condition resemble many other diseases, such as acute coronary syndrome, cardiogenic or septic shock, Atrial fibrillation, and COPD. Therefore, only history and physical examination are insufficient to accurately diagnose air embolism. The following are some important studies to diagnose this condition properly:
Laboratory Studies:
Laboratory studies are done when there is a suspicion of organ damage due to air embolism, as these studies are not specific and sensitive to diagnosing gas embolism.
Right-to-left shunting develops when this condition reaches the cardiovascular system. When it happens, taking arterial blood samples would help as they often show hypercapnia, hypoxemia, and metabolic acidosis.
Imaging Modalities:
Imaging studies for diagnosis are:
Transesophageal Echocardiography
TEE is a highly sensitive study that diagnoses embolism, and it detects even a minor amount of air in the right ventricle of the heart and pulmonary circulation. Studies show that even if 0.02 ml/kg air enters your body through a bolus injection, transesophageal echocardiography can detect it easily and efficiently.
Transesophageal and transthoracic echocardiography are used not only to detect VAE but also to rule out other differentials. For example, they help diagnose cardiac problems and pulmonary hypertension and assess the volume status of your body.10Guo, J. L., Wang, H. B., Wang, H., Le, Y., He, J., Zheng, X. Q., Zhang, Z. H., & Duan, G. R. (2021). Transesophageal echocardiography detection of air embolism during endoscopic surgery and validity of hyperbaric oxygen therapy: Case report. Medicine, 100(23), e26304. https://doi.org/10.1097/MD.0000000000026304
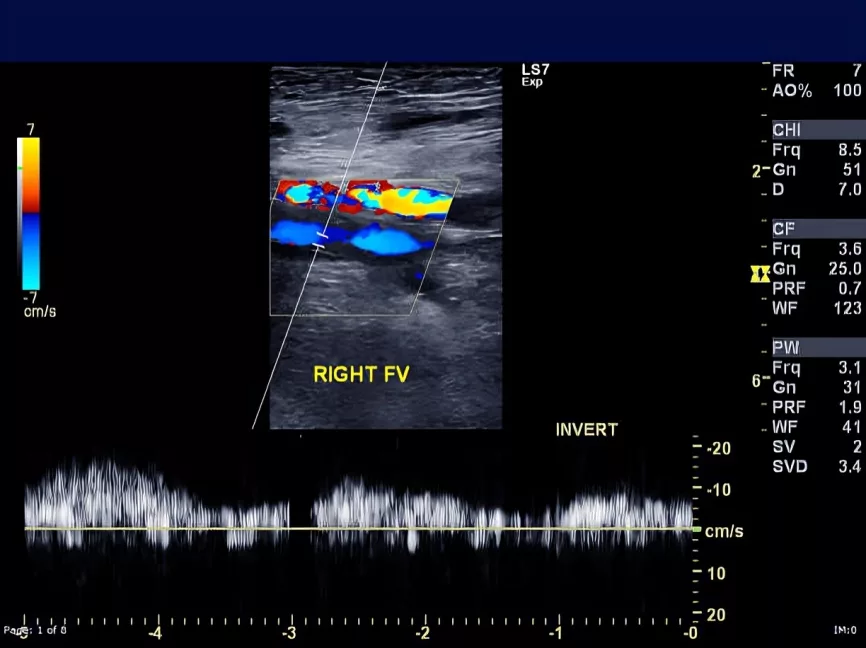
Doppler Ultrasonography
Doppler ultrasound is a noninvasive technique that can detect air emboli as small as 0.12 ml.It is a valuable tool for monitoring venous air embolism, especially in intraoperative and intensive care settings.11Gildenberg, P. L., O’Brien, R. P., Britt, W. J., & Frost, E. A. (1981). The efficacy of Doppler monitoring for the detection of venous air embolism. Journal of Neurosurgery, 54(1), 75–78. https://doi.org/10.3171/jns.1981.54.1.0075
Radiography
Chest radiographs are mostly normal in air embolism but, in some cases, can detect gas in the pulmonary arterial system and can also detect pulmonary edema.
CT and MRI
CT Scan is highly effective in identifying larger air emboli in the central venous system, right ventricle, or pulmonary artery. CT can also reveal brain edema or infarction in cases of arterial embolism. On the other hand, MRI is less commonly used for gas embolism and primarily detects changes in water concentration in brain tissues rather than directly visualizing air bubbles.
ECG:
ECG has less sensitivity to detect gas embolism. However, it may show signs like tachycardia and ST elevation. Patients developing MI have ST elevation in inferior leads, ST depression in AVL, and bradycardia.
End-Tidal Carbondioxide & Nitrogen:
Air embolism disrupts the ventilation-perfusion ratio, leading to a reduction in ETCO2 levels. A drop of more than 2 mmHg is suggestive of VAE. End-tidal nitrogen levels can also indicate embolism, but these methods are less sensitive than imaging modalities.
Pulse Oximetry:
Pulse oximetry shows a decreased oxygen saturation in the later stages of air embolism. Therefore, it isn’t considered a valuable option to diagnose early embolism.12Brathwaite, C. E., O’Malley, K. F., Ross, S. E., Pappas, P., Alexander, J., & Spence, R. K. (1992). Continuous pulse oximetry and the diagnosis of pulmonary embolism in critically ill trauma patients. The Journal of Trauma, 33(4), 528–531. https://doi.org/10.1097/00005373-199210000-00007

Pulmonary Artery Catheter:
A pulmonary artery catheter is not a well-known method for diagnosing air embolism. It only detects the pulmonary artery pressure that increases secondary to any obstruction caused by embolism.
Treatment of Air Embolism
Management of this complication involves:
- Finding its source.
- Preventing further entry of air into the body.
- Providing initial necessary support to the patient.
Initial Steps
- If air embolism is suspected, positioning the patient in the left lateral decubitus (Durant’s) position with a slight Trendelenburg tilt is recommended. This helps trap the air in the apex of the right ventricle, reducing its entry into the pulmonary circulation.
- For patients requiring cardiopulmonary resuscitation (CPR), the supine position is maintained for effective chest compressions.
Oxygen Therapy
Administering 100% oxygen is critical for reducing hypoxemia and displacing nitrogen, thereby decreasing the size of air bubbles.
Catheterization
Central venous catheterization directly removes air from the right atrium and is a valuable method for stable patients.
Cardiopulmonary Resuscitation
CPR helps to break large air bubbles into smaller ones and eventually remove them from the body.
Hyperbaric Oxygen Therapy (HBOT)
HBOT is the gold standard for treating gas embolism, particularly when the brain or heart is affected. It works by reducing the size of air bubbles and oxygenating ischemic tissues. Early initiation, ideally within six hours, improves prognosis significantly.

Fluid resuscitation is necessary to increase the intravascular volume of the body. The use of vasopressors and mechanical ventilation also give major support.13Shaikh, N., & Ummunisa, F. (2009). Acute management of vascular air embolism. Journal of emergencies, trauma, and shock, 2(3), 180–185. https://doi.org/10.4103/0974-2700.55330
Difference between Air Embolism and Pulmonary Embolism
The main difference between these two is the location of embolism. In an air embolism, the air bubble forms in any vein and artery and then blocks its blood supply, leading to ischemia.
When the air bubbles travel towards your lungs through the right heart and disrupt the pulmonary circulation, it is called pulmonary embolism.
Precautions
Some self-care tips to prevent the potential risks are:
- Put the head lower than the legs in a neurosurgical procedure
- Lower the air pressure during mechanical ventilation
- Avoid positive end-expiratory pressure as it may cause paradoxical emboli
- During catheter insertion and removal, cover the needle hub and prefer a sitting position. 14McCarthy, C. J., Behravesh, S., Naidu, S. G., & Oklu, R. (2016). Air Embolism: Practical Tips for Prevention and Treatment. Journal of clinical medicine, 5(11), 93. https://doi.org/10.3390/jcm5110093
Conclusion
In conclusion, faulty catheter insertion and removal form air bubbles in the artery or vein, causing central cardiovascular, pulmonary, and neurological symptoms. The prognosis depends upon the procedure that causes it. This complication can take one’s life if not treated at the right time.
Refrences
- 1Gordy, S., & Rowell, S. (2013). Vascular air embolism. International journal of critical illness and injury science, 3(1), 73–76. https://doi.org/10.4103/2229-5151.109428
- 2Marsh, P. L., Moore, E. E., Moore, H. B., Bunch, C. M., Aboukhaled, M., Condon, S. M., 2nd, Al-Fadhl, M. D., Thomas, S. J., Larson, J. R., Bower, C. W., Miller, C. B., Pearson, M. L., Twilling, C. L., Reser, D. W., Kim, G. S., Troyer, B. M., Yeager, D., Thomas, S. G., Srikureja, D. P., Patel, S. S., … Walsh, M. M. (2023). Iatrogenic air embolism: pathoanatomy, thromboinflammation, endotheliopathy, and therapies. Frontiers in immunology, 14, 1230049. https://doi.org/10.3389/fimmu.2023.1230049
- 3Ji, J., Tian, Y., Chen, L., & Li, B. (2020). Intraoperative VAE in the non-cardiac surgery role of perioperative echocardiography in a case series report. Annals of translational medicine, 8(12), 798. https://doi.org/10.21037/atm-20-497
- 4Lowenwirt, I. P., Chi, D. S., & Handwerker, S. M. (1994). Nonfatal venous air embolism during cesarean section: a case report and review of the literature. Obstetrical & gynecological survey, 49(1), 72–76. https://doi.org/10.1097/00006254-199401000-00028
- 5Kane, G., Hewins, B., & Grannis, F. W., Jr (1988). Massive air embolism in an adult following positive pressure ventilation. Chest, 93(4), 874–876. https://doi.org/10.1378/chest.93.4.874
- 6Alrasheedi, S. M., Alhumaidan, L. S., Alkhathami, A. A., & Alhati, M. (2023). Incidental Finding of Venous Air Embolism: A Case Report. Cureus, 15(1), e33896. https://doi.org/10.7759/cureus.33896
- 7Yeung, E., Adeboye, A., Granet, P., & Casos, S. (2021). Rare pathology in a trauma patient: air embolism following peripheral intravenous access. BMJ case reports 14(1), e240428. https://doi.org/10.1136/bcr-2020-240428
- 8Lanfranco, J., Romero Legro, I., Freire, A. X., Nearing, K., & Ratnakant, S. (2017). Pulmonary Air Embolism: An Infrequent Complication in the Radiology Suite. The American journal of case reports, 18, 80–84. https://doi.org/10.12659/ajcr.901098
- 9Rahman, Z. U., Murtaza, G., Pourmorteza, M., El Minaoui, W. K., Sethi, P., Mamdouhi, P., & Paul, T. (2016). Cardiac Arrest as a Consequence of Air Embolism: A Case Report and Literature Review. Case reports in medicine, 2016, 8236845. https://doi.org/10.1155/2016/8236845
- 10Guo, J. L., Wang, H. B., Wang, H., Le, Y., He, J., Zheng, X. Q., Zhang, Z. H., & Duan, G. R. (2021). Transesophageal echocardiography detection of air embolism during endoscopic surgery and validity of hyperbaric oxygen therapy: Case report. Medicine, 100(23), e26304. https://doi.org/10.1097/MD.0000000000026304
- 11Gildenberg, P. L., O’Brien, R. P., Britt, W. J., & Frost, E. A. (1981). The efficacy of Doppler monitoring for the detection of venous air embolism. Journal of Neurosurgery, 54(1), 75–78. https://doi.org/10.3171/jns.1981.54.1.0075
- 12Brathwaite, C. E., O’Malley, K. F., Ross, S. E., Pappas, P., Alexander, J., & Spence, R. K. (1992). Continuous pulse oximetry and the diagnosis of pulmonary embolism in critically ill trauma patients. The Journal of Trauma, 33(4), 528–531. https://doi.org/10.1097/00005373-199210000-00007
- 13Shaikh, N., & Ummunisa, F. (2009). Acute management of vascular air embolism. Journal of emergencies, trauma, and shock, 2(3), 180–185. https://doi.org/10.4103/0974-2700.55330
- 14McCarthy, C. J., Behravesh, S., Naidu, S. G., & Oklu, R. (2016). Air Embolism: Practical Tips for Prevention and Treatment. Journal of clinical medicine, 5(11), 93. https://doi.org/10.3390/jcm5110093

