Compartment Syndrome is a life-threatening condition that occurs when pressure within a muscle compartment increases. These compartments consist of muscles, nerves, and blood vessels that are enclosed in a compact membrane called fascia. As pressure rises in these areas, it can cut off the blood supply, which ultimately damages muscles and nerves.1Mubarak, S. J., & Owen, C. A. (1975). Double incision fasciotomy of the leg for decompression in compartment syndromes. The Journal of Bone and Joint Surgery.
This condition can involve any part of the body, but is most commonly seen in the arms, legs, and particularly in the lower legs. If this pressure builds up quickly, it is referred to as acute compartment syndrome. If it spreads slowly over time, it is called chronic compartment syndrome.
The key factor in the development of compartment syndrome is increased intracompartmental pressure. Usually, pressure in the muscular compartment is not very high and is well-regulated. However, the problem arises if you develop any swelling, bleeding, or fluid buildup that increases this pressure, resulting in restricted blood flow. If not promptly treated, the resulting ischemia can lead to permanent damage to muscles and nerves, and in severe cases, may require limb amputation.2Matsen, F. A. (1980). Compartmental syndromes: diagnosis and treatment. Clinical Orthopaedics and Related Research.
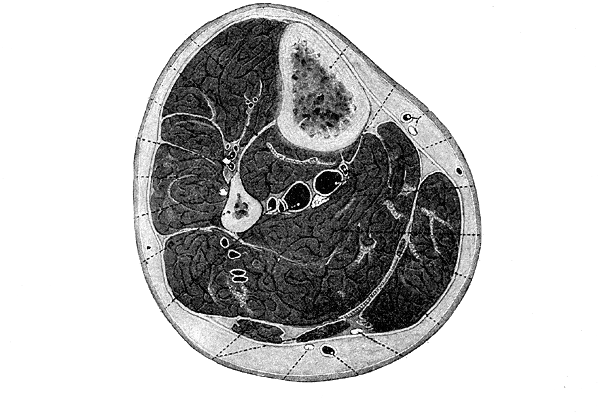
Image courtesy of Gray’s Anatomy, 20th edition (1918), via Wikimedia Commons. Public Domain.
How Common is Compartment Syndrome?
This is not a very common condition, but it is highly important in orthopedics and trauma treatments. Acute compartment syndrome is most commonly observed among people who have suffered severe injury. The prevalence of acute compartment syndrome is around 3.1/100000 persons annually. Nevertheless, in patients having any fracture, particularly a tibial shaft fracture, the chances are multiplied almost 7 times.3McQueen, M. M., Gaston, P., & Court-Brown, C. M. (2000). Acute compartment syndrome: who is at risk?. The Journal of Bone and Joint Surgery.
Conversely, chronic compartment syndrome is much more common among athletes, particularly runners, cyclists, and soldiers. Many athletes who complain about pain in their legs or calves may be experiencing chronic compartment syndrome without knowing it.4Turnipseed, W. D. (2002). Clinical review of patients treated for chronic compartment syndrome of the lower extremity. Archives of Surgery.
Types of Compartment Syndrome
Acute Compartment Syndrome:
Acute compartment syndrome is a medical emergency. Normally, it is a sequel to trauma, such as a fracture, crush injury, or even the fitting of a tight cast or bandage. This can develop within a few hours after injury and progresses rapidly. The hallmark feature is severe pain that’s out of proportion to the injury. If left untreated, it can cause irreversible damage in just 6 to 8 hours.5Rorabeck, C. H., & Macnab, I. (1976). The pathophysiology of the anterior tibial compartmental syndrome: an experimental investigation. The Journal of Bone and Joint Surgery.
Chronic Compartment Syndrome:
This type, also known as chronic exertional compartment syndrome (CECS), develops gradually with repeated physical activity. It’s more common in athletes. When the activity stops, the pain usually goes away.6Pedowitz, R. A., et al. (1990). Modified criteria for the objective diagnosis of chronic compartment syndrome of the leg. The American Journal of Sports Medicine.
This type doesn’t require emergency surgery but may necessitate medical evaluation and lifestyle adjustments. According to the area involved, the following are some variants of this condition:
Calf Compartment Syndrome
- Common among runners.
- The calf muscles, confined in tight fascia, can swell during exertion.
- It’s a major reason why runners may suddenly drop their stamina or feel intense pain after running a few miles.
Lateral Compartment Syndrome
- Affects the outer side of the lower leg.
- It often presents with symptoms in foot movement.
- You can misunderstand it as ankle sprains or shin splints.
Ankle Compartment Syndrome
Though rarer, compartment syndrome can also affect the ankle area, especially following trauma or surgical procedures.
Leg Compartment Syndrome
- This is the most common site for both acute and chronic types.
- With four distinct muscle compartments in the lower leg, any of them can be affected.
- The anterior compartment is most often involved.
- Untreated leg compartment syndrome can result in foot drop—a condition where you can’t lift the front part of your foot.
Acute Compartment Syndrome Causes
Acute compartment syndrome is often sudden and aggressive. Trauma is usually the main cause of acute disease, which results in bleeding or swelling within a compartment. Common triggers include:7Elliott, K. G., & Johnstone, A. J. (2003). Diagnosing acute compartment syndrome. Journal of Bone and Joint Surgery.
- Fractures – Especially tibial shaft fractures, which are the leading cause.
- Crush injuries – Car accidents, industrial injuries, or building collapses can crush limbs, leading to increased internal pressure.
- Burns – These can cause extensive swelling under the skin.
- Overtight bandages or casts – External compression can inhibit circulation, raising internal pressure.
- Surgery complications – Post-surgical swelling or bleeding may result in acute pressure buildup.
As pressure builds, capillary perfusion decreases, starving the muscles and nerves of oxygen and nutrients. If left untreated, this can lead to necrosis, tissue death, and permanent disability.
Chronic Compartment Syndrome Causes
Chronic or exertional compartment syndrome is different. It develops gradually due to repeated muscle use, especially during exercise. Typical causes include:8Styf, J. R. (1989). Chronic compartment syndrome: diagnosis and management. Clinics in Sports Medicine.
- High-impact sports – Running, biking, and rowing are common culprits.
- Improper footwear – Shoes lacking support may alter stride and increase stress.
- Poor biomechanics – Flat feet or abnormal gait can strain muscles unevenly.
- Overtraining – Lack of rest doesn’t allow muscles to heal between workouts.
During activity, muscles expand. In healthy individuals, this expansion is accommodated by the fascia. In those with chronic compartment syndrome, the fascia doesn’t stretch sufficiently, leading to increased compartment syndrome pressure and associated pain. Once activity stops, the pressure normalizes, and the pain subsides until the next workout.
Compartment Syndrome Symptoms
The symptoms of compartment syndrome vary depending on whether the condition is acute or chronic, but certain signs are crucial in both.
- Severe pain – The patient often describes it as deep, persistent, and out of proportion to the injury.
- Swelling, tightness, and shiny skin in the affected limb.
- Numbness, tingling, and muscle weakness are due to nerve and blood vessel compression.
- Pain doesn’t ease with rest or medication, making it a surgical emergency. Without prompt treatment, tissue death can occur within hours.
Unlike other injuries, the pain doesn’t subside with rest or medication. It continues to intensify.9Heemskerk, J. L., & Kitslaar, P. J. (1990). Clinical features and diagnosis of acute compartment syndrome. Injury
Chronic Compartment Syndrome:
- Cramping pain during exercise, typically in the calves.
- Tightness, tingling, and weakness, which resolve after rest.
- Symptoms are cyclical, often delaying diagnosis.10Detmer, D. E., et al. (1985). Chronic compartment syndrome: diagnosis and management. The American Journal of Sports Medicine.
The 6 Ps of Acute Compartment Syndrome:
A classic diagnostic tool includes:
- Pain – Severe, worsens with movement (early sign)
- Paresthesia – Numbness or tingling
- Pallor – Pale skin from poor circulation
- Paralysis – Loss of movement
- Pulselessness – Absent pulse (late and unreliable)
- Poikilothermia – The Affected limb feels cold
The earliest and most frequent signs are pain and paresthesia. Waiting for pulselessness or paralysis means you’ve waited too long.11Mubarak, S. J., & Hargens, A. R. (1981). Compartment syndromes and Volkmann’s contracture. Saunders Publishing.
The doctors and responders are under training to take immediate action even when only a couple or so of these Ps are involved, particularly in cases of high risk, such as fractures or crush injuries.
How Do Providers Diagnose Compartment Syndrome?
Compartment syndrome is mainly diagnosed clinically, which focuses on patient history and physical examination. But, because of the high stakes involved, doctors use some tools to verify the suspicions.12Matsen, F. A., & Winquist, R. A. (1980). Diagnosis and management of compartmental syndromes. The Western Journal of Medicine. Rapid diagnosis is the challenge in acute cases. Doctors look for:
- History of trauma
- Severe, unrelenting pain
- Pain with passive movement
- Tense, swollen compartments
In chronic cases, diagnosis is more structured. Testing is usually done before and after exercise using a pressure monitor. The patient performs activities that trigger their symptoms, and then pressures are measured.
A clear, accurate diagnosis is essential because treatment for compartment syndrome, especially the acute type, is surgical. Misdiagnosis can lead to permanent muscle loss or even amputation.
Compartment Syndrome Tests & Tools:
Several diagnostic tools and tests aid in identifying compartment syndrome:13Rorabeck, C. H. (1984). The pathophysiology of the anterior tibial compartmental syndrome: an experimental investigation. Clinical Orthopaedics and Related Research.
- Stryker Intra-Compartmental Pressure Monitor – The gold standard for pressure measurement.
- MRI – Especially useful in chronic cases to detect muscle changes.
- Near-Infrared Spectroscopy (NIRS) – A newer, non-invasive method under research.
- Electromyography (EMG) – Sometimes used in chronic cases to assess nerve function.

Compartment Pressure Monitor:
If the clinical picture is uncertain, doctors may use a compartment pressure monitor. This tool directly measures the pressure inside the muscle compartment using a needle and a specialized device. A reading above 30 mmHg or a delta pressure (diastolic BP minus compartment pressure) less than 30 is usually diagnostic. It’s calculated as:
Delta Pressure = Diastolic Blood Pressure – Intracompartmental Pressure
Compartment Syndrome Treatment
Immediate Emergency Treatment:
Time is most important in managing acute cases. The primary goal of emergency care is to relieve pressure within the compromised compartment. This is done by a surgical procedure called a fasciotomy. Here’s what emergency treatment typically looks like:14Matsen, F. A., Krugmire, R. B. (1978). Compartmental syndromes. The New England Journal of Medicine.
- Remove restrictive dressings or casts immediately if they’re contributing to the condition.
- Assess compartment pressure if symptoms suggest an acute case.
- Immediate fasciotomy when pressure readings and symptoms meet the criteria.
If a fasciotomy is delayed, tissues begin to die from lack of oxygen. Within 6 hours, irreversible damage can occur. That’s why it’s often said in medicine: “Time is muscle.”
Supportive care is also essential. Patients may receive:
- IV fluids
- Pain management
- Antibiotics to prevent infection post-surgery
- Monitoring in an intensive care unit, if necessary
No amount of medication can lower compartment pressure—that’s why surgery is non-negotiable in acute cases.
Surgical Options: Fasciotomy Explained:
Fasciotomy is the best available treatment in case of acute compartment syndrome. During the process, a surgeon cuts the fascia and the skin using one or several long incisions in order to relieve pressure and normalize blood flow.15Mubarak, S. J., et al. (1976). The pathophysiology of acute compartment syndrome: an experimental investigation. The Journal of Bone and Joint Surgery.

It depends on the area involved and how severe the case is; various compartments may need to be opened.
What happens during a Fasciotomy?
- Long incisions are made across the affected compartments by the surgeon.
- After the pressure has been relieved, the muscles and nerves are examined to check their viability.
- After a few days, the wound might be closed, provided the tissue involved is healthy.
- When the swelling is heavy, the wound is usually left to heal itself, and a temporary dressing or vacuum-assisted closure apparatus is applied.
Elective fasciotomy can be advised in chronic cases where conservative management methods such as physical therapy, rest, and anti-inflammatory drugs do not work.
Recovery & Rehabilitation
Recovery after fasciotomy or after the treatment is dependent on several factors, such as the time of commencement of treatment, as well as the severity of the disease.16Vaillancourt, C., et al. (2001). Long-term functional outcomes following fasciotomy for compartment syndrome. The Canadian Journal of Surgery.
Short-term recovery is:
- 1–3 days stay in the hospital after surgery
- Daily dressing or vacuum-assisted wound management
- Pain management and antibiotics
The long-term rehabilitation can include:
- Physical therapy to restore the strength and range of movements
- Scar management
- Observation of signs of infection or damage to the nerves
How Soon After Treatment Will I Feel Better?
The duration during which a person feels better is extremely different according to the nature of the disease, its severity, and the time of prompt treatment. Patients with leg compartment syndrome may be required to do retraining of the gait, whereas patients with calf compartment syndrome can concentrate on muscle flexibility and strength.
Milestones of rehabilitation usually appear in the following way:
| Timeframe | Recovery Stage |
| First 1–2 weeks | Pain control, wound healing begin |
| 3–6 weeks | Begin physical therapy, light movement |
| 2–3 months | Strength training, return to normal activity |
| 6+ months | Full return to sport (if applicable) |
Proper follow-up and rehabilitation can greatly enhance recovery and ensure long-term function is preserved.
Compartment Syndrome vs Crush Syndrome
Although both can be related, they are not the same condition. Understanding their differences can help clarify the proper treatment path and avoid dangerous missteps.17Smith, J. F. (1990). Crush syndrome: pathophysiology and treatment. Journal of Trauma.
| Feature | Compartment Syndrome | Crush Syndrome |
| Cause | Increased pressure within a muscle compartment | Severe muscle damage from prolonged compression |
| Timing | It can happen within hours of injury | Develops after hours of continuous pressure |
| Key Danger | Muscle and nerve ischemia | Systemic release of toxins (myoglobin, potassium) |
| Main Treatment | Fasciotomy | IV fluids, dialysis, and manage systemic effects |
| Complications | Tissue death, amputation | Kidney failure, cardiac arrest |
The crush syndrome is a systemic disorder, and it is usually found in entrapment injuries (e.g., earthquakes, fallen buildings). It causes rhabdomyolysis, where the products of muscle catabolism enter the circulation, which is likely to result in kidney failure.18Better, O. S., & Stein, J. H. (1990). Early management of shock and prophylaxis of acute renal failure in traumatic rhabdomyolysis. The New England Journal of Medicine.
On the one hand, compartment syndrome is a local emergency, which is centered around one compartment or limb, the most severe danger of which is ischemia and irreversible muscle and nerve damage.
Long-Term Management & Prevention Tips
Preventing compartment syndrome is not always possible, especially in trauma cases. But small changes can minimize your risk in chronic cases.19Tzortziou, A., & Theodoropoulos, J. S. (2012). Preventing chronic exertional compartment syndrome. Clinical Journal of Sport Medicine.
The following are some of the prevention and management strategies:
- Physical therapy
- Avoid overtraining
- Proper footwear
- Cross-training
- Pay attention to your body – constant aching, pressure sensation, swelling are not normal, have checked out.
- Follow up regularly if you’ve experienced this condition before or are at high risk.
Most importantly, the best weapons are early detection and immediate medical treatment to save the long-term situation of health and mobility.
Conclusion
The compartment syndrome is definitely among the deadliest and most time-urgent conditions you may ever have. It comes either in acute form, where it requires urgent surgery, or in chronic form, which impairs the capability of an athlete to work. Learning acute and chronic pain symptoms and deciding when to help can be crucial. Be familiar with the 6 Ps and watch the symptoms.
Most people survive with a good prognosis if the diagnosis is made in time and correct treatment is administered. Therefore, be up to date, be active, and do not be afraid to ask for medical assistance in case something seems wrong.
Refrences
- 1Mubarak, S. J., & Owen, C. A. (1975). Double incision fasciotomy of the leg for decompression in compartment syndromes. The Journal of Bone and Joint Surgery.
- 2Matsen, F. A. (1980). Compartmental syndromes: diagnosis and treatment. Clinical Orthopaedics and Related Research.
- 3McQueen, M. M., Gaston, P., & Court-Brown, C. M. (2000). Acute compartment syndrome: who is at risk?. The Journal of Bone and Joint Surgery.
- 4Turnipseed, W. D. (2002). Clinical review of patients treated for chronic compartment syndrome of the lower extremity. Archives of Surgery.
- 5Rorabeck, C. H., & Macnab, I. (1976). The pathophysiology of the anterior tibial compartmental syndrome: an experimental investigation. The Journal of Bone and Joint Surgery.
- 6Pedowitz, R. A., et al. (1990). Modified criteria for the objective diagnosis of chronic compartment syndrome of the leg. The American Journal of Sports Medicine.
- 7Elliott, K. G., & Johnstone, A. J. (2003). Diagnosing acute compartment syndrome. Journal of Bone and Joint Surgery.
- 8Styf, J. R. (1989). Chronic compartment syndrome: diagnosis and management. Clinics in Sports Medicine.
- 9Heemskerk, J. L., & Kitslaar, P. J. (1990). Clinical features and diagnosis of acute compartment syndrome. Injury
- 10Detmer, D. E., et al. (1985). Chronic compartment syndrome: diagnosis and management. The American Journal of Sports Medicine.
- 11Mubarak, S. J., & Hargens, A. R. (1981). Compartment syndromes and Volkmann’s contracture. Saunders Publishing.
- 12Matsen, F. A., & Winquist, R. A. (1980). Diagnosis and management of compartmental syndromes. The Western Journal of Medicine.
- 13Rorabeck, C. H. (1984). The pathophysiology of the anterior tibial compartmental syndrome: an experimental investigation. Clinical Orthopaedics and Related Research.
- 14Matsen, F. A., Krugmire, R. B. (1978). Compartmental syndromes. The New England Journal of Medicine.
- 15Mubarak, S. J., et al. (1976). The pathophysiology of acute compartment syndrome: an experimental investigation. The Journal of Bone and Joint Surgery.
- 16Vaillancourt, C., et al. (2001). Long-term functional outcomes following fasciotomy for compartment syndrome. The Canadian Journal of Surgery.
- 17Smith, J. F. (1990). Crush syndrome: pathophysiology and treatment. Journal of Trauma.
- 18Better, O. S., & Stein, J. H. (1990). Early management of shock and prophylaxis of acute renal failure in traumatic rhabdomyolysis. The New England Journal of Medicine.
- 19Tzortziou, A., & Theodoropoulos, J. S. (2012). Preventing chronic exertional compartment syndrome. Clinical Journal of Sport Medicine.

