What is Alkaptonuria?
Alkaptonuria, also known as black urine disease or black bone disease, is a rare hereditary “autosomal recessive” condition stemming from an inborn error in protein metabolism. This condition arises due to a deficiency in the enzyme known as homogentisate 1,2 dioxygenase (HGD) required for tyrosine catabolism. This deficiency results in the excessive accumulation of homogentisic acid (HGA) within the body’s connective tissues, which ultimately leads to a condition known as ochronosis. Ochronosis involves the deposition of dark pigments in various tissues, causing various clinical symptoms and manifestations. The hallmark of the disease is the passage of urine that turns black when left standing.
Epidemiology of Alkaptonuria
Alkaptonuria is a rare illness that affects people all over the world. Alkaptonuria affects 1 per 100,000 to 250,000 people worldwide. In the United States, the incidence is about 1 in 1,000,000 people, with the AKU Society and the DevelopAKUre Consortium estimating around 92 patients in the country. Slovakia and the Dominican Republic are where it is mostly recorded.1Sharabi, A. F., & Goudar, R. B. (2023). Alkaptonuria. In StatPearls. StatPearls Publishing. It affects people of all ethnicities, though Africans are significantly more likely to experience it. The illness affects men and women equally, albeit men are more severely affected.
Pathophysiology of Alkaptonuria
The defect lies in the catabolic pathway of tyrosine, which contains a para-hydroxylated ring structure. Tyrosine is a vital amino acid used for various essential functions in the body, including making melanin, hormones, and various proteins. However, most of the tyrosine we consume is not used and is eventually converted into substances called acetoacetate and malate.
Tyrosine requires an enzyme homogentisate1,2-dioxygenase (HGD) for its metabolism. It plays a crucial role in the tyrosine metabolic pathway. Its primary function involves the conversion of homogentisic acid (HGA) into maleylacetoacetate, a key step in the breakdown of tyrosine. HGD is a protein composed of 445 amino acids and is situated on chromosome 3q13.33 within the human genome.2Sharabi AF, Goudar RB. Alkaptonuria. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560571/
However, when mutations occur in the HGD gene, they disrupt the normal function of the HGD enzyme. This genetic alteration results in a deficiency of the HGD enzyme, leading to the abnormal accumulation of homogentisic acid (HGA) in the body, which is the hallmark feature of Alkaptonuria.
Symptoms of Alkaptonuria
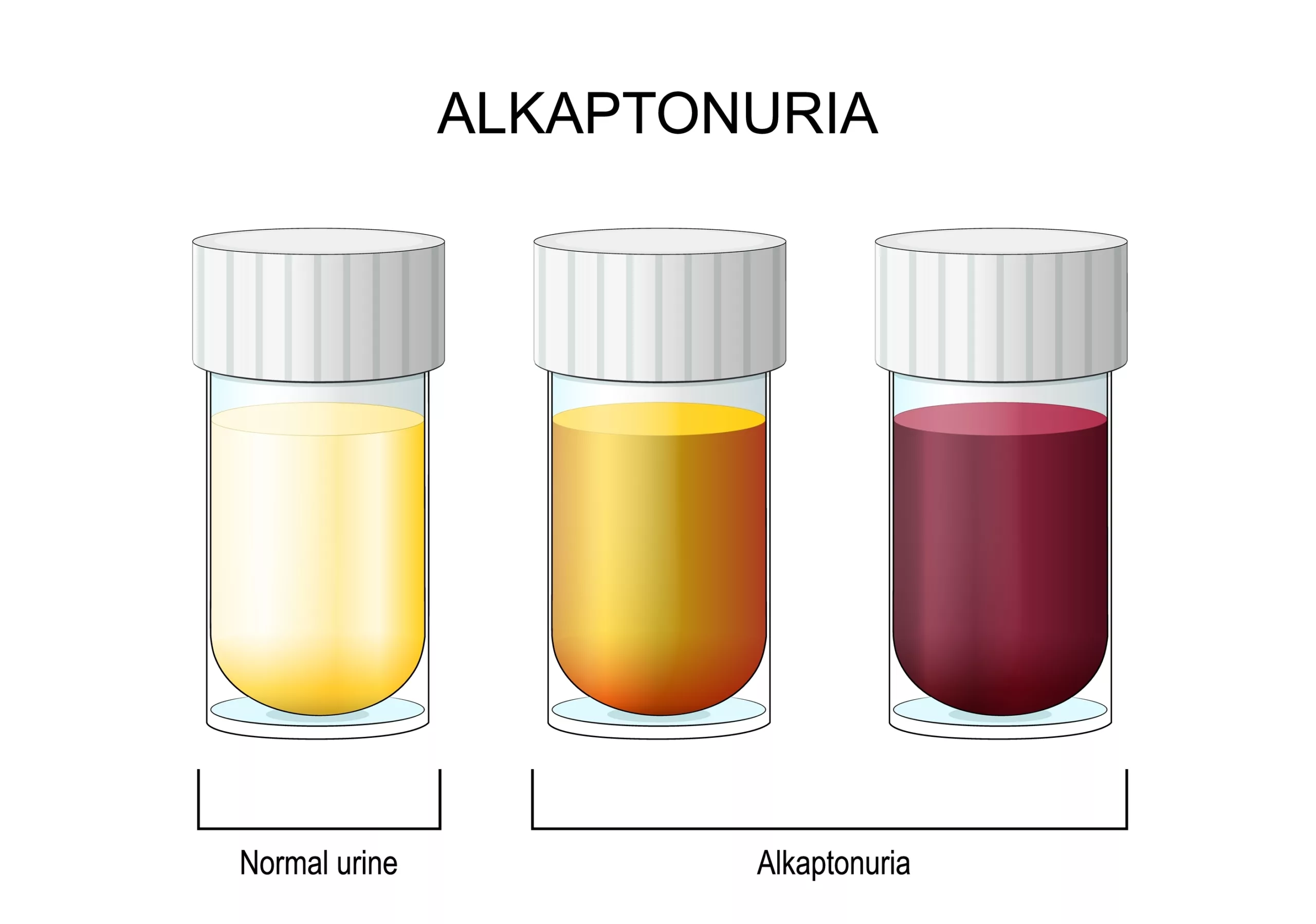
One of the earliest indications is dark stains on a baby’s nappy. The affected individual starts to experience symptoms of early-onset osteoarthritis by age 20 or 30. Moreover, the bones and cartilage seem discolored and brittle because of homogentisic acid buildup. This buildup can lead to osteoarthritis, especially in the spine and large joints. A hallmark of alkaptonuria is urine that turns dark brown or black when exposed to air, although this color change often goes unnoticed and may not occur until several hours after urination.3Rudebeck, M., Scott, C., Sireau, N., & Ranganath, L. (2020). A patient survey on the impact of alkaptonuria symptoms as perceived by the patients and their experiences of receiving diagnosis and care. JIMD reports, 53(1), 71–79. https://doi.org/10.1002/jmd2.12101
Additional signs of alkaptonuria include:
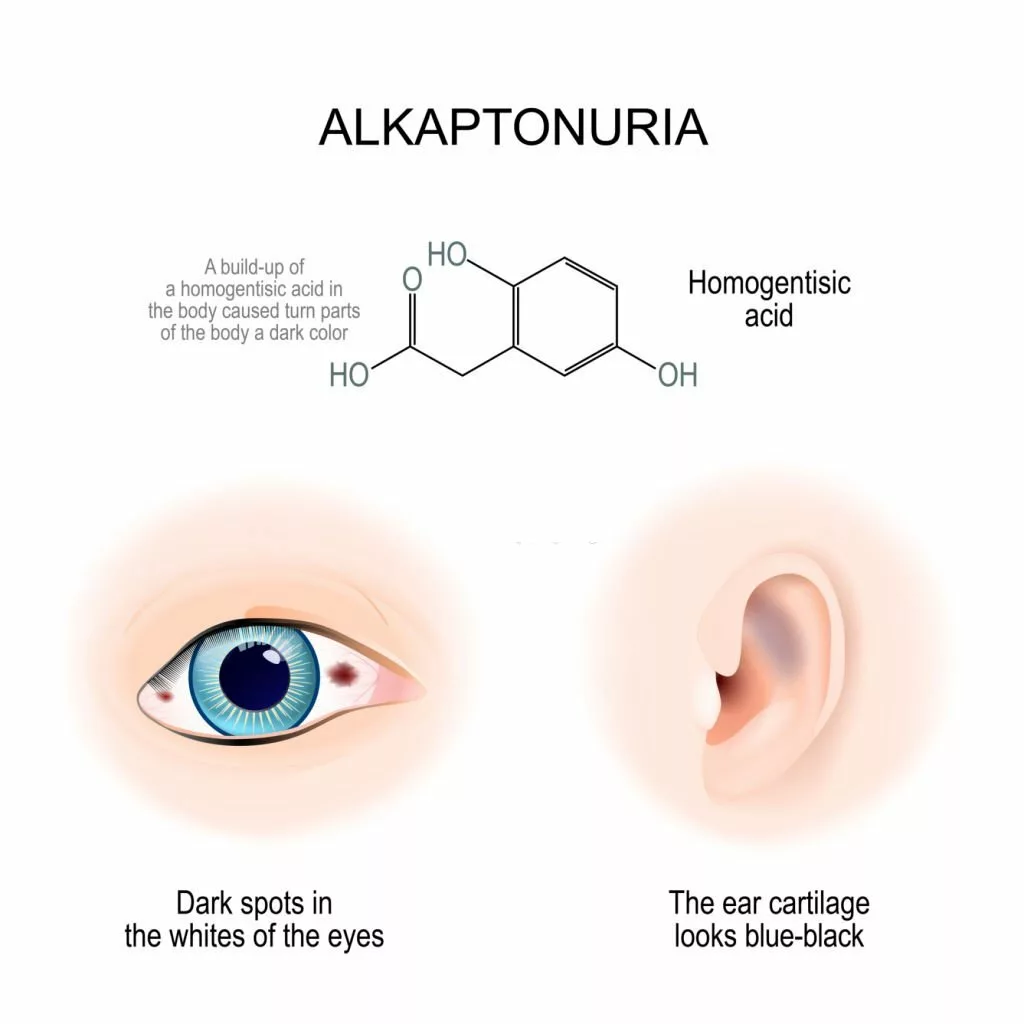
- Dark spots in the sclera of the eyes
- Thickened and darkened cartilage in your ears
- Blue-speckled discoloration of your skin, particularly around sweat glands
- Dark-colored sweat or sweat stains
- Black earwax
- Kidney stones.
- Arthritis (especially hip and knee joints)
Moreover, heart issues might potentially result from alkaptonuria.
Signs of Alkaptonuria
Grey discoloration may be found in the sclerae or ear cartilage. Calcifications may be palpable in the discolored areas, particularly in the cartilage of the ear. Joint mobility diminishes, as in osteoarthritis. Spontaneous fusion of one or more discs may occur, with consequent diminished spinal flexion. Joint effusions, particularly in the knee, are common, and the range of motion may be significantly diminished.
Alkaptonuria Diagnosis
Diagnosing alkaptonuria involves a comprehensive evaluation that takes into account unique symptoms, a detailed patient medical history, a meticulous clinical examination, and specialized diagnostic tests. These tests may include:
Chromatography Test of Urine:
This is a fundamental diagnostic step where urine samples are analyzed to detect the presence of homogentisic acid, a key marker of alkaptonuria. Homogentisic acid levels in a 24-hour urine sample are measured using gas chromatography-mass spectrometry (GC-MS) analysis. Typically, individuals with Alkaptonuria (AKU) excrete a daily amount of HGA ranging from 1 to 8 grams.4Introne WJ, Perry M, Chen M. Alkaptonuria. 2003 May 9 [Updated 2021 Jun 10]. In: Adam MP, Mirzaa GM, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1454/
Imaging Studies:
Various imaging techniques can be employed to assess the impact of alkaptonuria on different body systems. These may encompass:
- ECG (Electrocardiogram): An ECG is used to evaluate cardiac function and detect any potential cardiac complications associated with alkaptonuria.
- Chest X-ray: A chest X-ray can reveal any abnormalities in the chest area, providing insights into respiratory health.
- CT Scan (Computed Tomography): This imaging technique offers detailed cross-sectional images, helping assess organ and tissue involvement.
- MRI of the Spine: Magnetic Resonance Imaging is particularly useful in examining the spinal column for any alkaptonuria-related effects.
Histopathology:
In some cases, a histopathological examination of affected tissues or organs may be necessary. This involves microscopic analysis of tissue samples to confirm the presence of alkaptonuria-related changes.
Treatment of Alkaptonuria
Alkaptonuria has no specific treatment. Instead, most of the treatment time is spent in treating symptoms.5Ranganath LR, Jarvis JC, Gallagher JA. Recent advances in the management of alkaptonuria (invited review; best practice article). J Clin Pathol. 2013 May;66(5):367-73.
Anti-inflammatory Drugs
Doctors frequently prescribe anti-inflammatory drugs to people with alkaptonuria to address joint pain. In extreme circumstances, they may advise stronger drugs, including narcotics.
Nitisinone
Adults with alkaptonuria can delay its progression with the help of a medication called nitisinone. Nitisinone reduces homogentisic acid levels in the blood and urine, reducing and delaying the progression of alkaptonuria and enhancing morbidity.6Teke Kisa, P., Eroglu Erkmen, S., Bahceci, H., Arslan Gulten, Z., Aydogan, A., Karalar Pekuz, O. K., Yuce Inel, T., Ozturk, T., Uysal, S., & Arslan, N. (2022). Efficacy of Phenylalanine- and Tyrosine-Restricted Diet in Alkaptonuria Patients on Nitisinone Treatment: Case Series and Review of Literature. Annals of nutrition & metabolism, 78(1), 48–60. https://doi.org/10.1159/000519813
Vitamin C
The mild antioxidant nature of ascorbic acid retards the process of converting homogentisate into the polymeric material deposited in cartilaginous tissues. Furthermore, healthcare professionals often recommend ascorbic acid, also known as vitamin C, as a treatment because it inhibits the oxidative conversion of homogentisic acid to benzoquinone acetic acid. However, it does not impact the excretion of homogentisic acid through the urine.
Low-Protein Diet
A low-protein diet can lower the tyrosine load and lessen the severity of the illness, although following the recommended diet is challenging. However, there is no proof of effectiveness.7Mistry JB, Bukhari M, Taylor AM. Alkaptonuria. Rare Dis. 2013;1:e27475.
Pain Management
Pain management is individualized for each person’s unique situation and necessitates ongoing monitoring and modification.
Physical & Occupational Therapy
Physical and occupational therapy, which may keep muscles and joints flexible and strong, may be helpful for some people with alkaptonuria.
Genetic Counseling
Affected people and their families may benefit from genetic counseling.
Mortality & Morbidity
Life expectancy is normal; however, associated morbidity can be significant. Early involvement of the intervertebral discs at the thoracic and lumbar levels is very common. Typically, significant back pain begins at the age of 30 years. It frequently involves the large joints (knee, shoulder, and hip); at least half of all patients undergo joint replacement by the middle of the sixth decade of life. Achilles tendon involvement is also common and may result in tearing. Involvement of the aortic leaflets, mitral valve leaflets, or both is common, and calcifications of the coronary arteries occur in one-half of all patients before age 60 years.
Complications
Published case reports make it clear that complications can also occur in AKU, a chronic progressive disorder. The complications include:
Calcification of the Ear Cartilage
Affected individuals develop ochronosis, in which connective tissue such as cartilage turns blue, grey, or black due to the chronic accumulation of homogentisic acid. In many individuals, the cartilage within the ear may become thickened, irregular, and discolored blue, grey, or black.
Calcified Lumbar Discs
A unique form of lumbar disc herniation, characterized by the calcified herniated site occupying the vertebral canal bone, is known as calcified lumbar disc herniation. The particular imaging findings of alkaptonuria include the growing disc calcification and the related vacuum phenomena with limited osteophytic alterations.
Severe Arthritis
Long-term alkaptonuria notably brings on chronic joint pain and inflammation (arthritis), primarily affecting the spine and major joints, resulting in ochronotic arthropathy. Severe arthritis can be incapacitating. Common symptoms include low back pain and stiffness, which can occur before age 30.
Ankylosis
Ankylosis, which refers to the abnormal stiffening and immobility of a joint due to fusion of the bones, can occur in individuals with alkaptonuria. This condition often leads to lumbar discomfort and arthritis, resulting in joint effusions, reduced joint movement, and decreased spinal and thoracic mobility, which can cause significant disability. Additionally, osteopenia, or reduced bone density, increases the risk of fractures in affected individuals.
Aortic or Mitral Valvulitis
The emergence of aortic or mitral valvulitis is the most frequent significant consequence of alkaptonuric ochronosis. Although numerous valves may be involved, the aortic valve has the highest incidence of calcifications and stenosis, followed by the mitral and pulmonary valves.8Steger C. M. (2011). Aortic valve ochronosis: a rare manifestation of alkaptonuria. BMJ case reports 2011, bcr0420114119. https://doi.org/10.1136/bcr.04.2011.4119 Valvular disease in alkaptonuria typically affects individuals at least in middle age, with the average age being 54 years. The reported youngest patient was 26 years old. Males and females both have an equal prevalence of this complication.
Alkaptonuria Ochronosis
In alkaptonuria, ochronosis is the bluish-black staining in specific tissues, including ocular and ear cartilage. Accumulation of HGA causes this distinctive blue-black staining.9Albers SE, Brozena SJ, Glass LF, Fenske NA. Alkaptonuria and ochronosis: case report and review. J Am Acad Dermatol. 1992 Oct;27(4):609-14. doi: 10.1016/0190-9622(92)70230-d. PMID: 1401313. Exogenous ochronosis can occasionally result from exposure to various chemicals, including benzene, trinitrophenol, mercury, resorcinol, picric acid, hydroquinone, and antimalarials.
In conclusion, Alkaptonuria is a rare genetic disorder affecting the body’s ability to metabolize tyrosine, accumulating homogentisic acid. This buildup can cause a range of health issues, including joint and connective tissue problems. While there is no cure for AKU, early diagnosis and management can help improve the quality of life for individuals with this condition. Research into potential treatments continues, offering hope for a brighter future for those living with Alkaptonuria.
Refrences
- 1Sharabi, A. F., & Goudar, R. B. (2023). Alkaptonuria. In StatPearls. StatPearls Publishing.
- 2Sharabi AF, Goudar RB. Alkaptonuria. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK560571/
- 3Rudebeck, M., Scott, C., Sireau, N., & Ranganath, L. (2020). A patient survey on the impact of alkaptonuria symptoms as perceived by the patients and their experiences of receiving diagnosis and care. JIMD reports, 53(1), 71–79. https://doi.org/10.1002/jmd2.12101
- 4Introne WJ, Perry M, Chen M. Alkaptonuria. 2003 May 9 [Updated 2021 Jun 10]. In: Adam MP, Mirzaa GM, Pagon RA, et al., editors. GeneReviews® [Internet]. Seattle (WA): University of Washington, Seattle; 1993-2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK1454/
- 5Ranganath LR, Jarvis JC, Gallagher JA. Recent advances in the management of alkaptonuria (invited review; best practice article). J Clin Pathol. 2013 May;66(5):367-73.
- 6Teke Kisa, P., Eroglu Erkmen, S., Bahceci, H., Arslan Gulten, Z., Aydogan, A., Karalar Pekuz, O. K., Yuce Inel, T., Ozturk, T., Uysal, S., & Arslan, N. (2022). Efficacy of Phenylalanine- and Tyrosine-Restricted Diet in Alkaptonuria Patients on Nitisinone Treatment: Case Series and Review of Literature. Annals of nutrition & metabolism, 78(1), 48–60. https://doi.org/10.1159/000519813
- 7Mistry JB, Bukhari M, Taylor AM. Alkaptonuria. Rare Dis. 2013;1:e27475.
- 8Steger C. M. (2011). Aortic valve ochronosis: a rare manifestation of alkaptonuria. BMJ case reports 2011, bcr0420114119. https://doi.org/10.1136/bcr.04.2011.4119
- 9Albers SE, Brozena SJ, Glass LF, Fenske NA. Alkaptonuria and ochronosis: case report and review. J Am Acad Dermatol. 1992 Oct;27(4):609-14. doi: 10.1016/0190-9622(92)70230-d. PMID: 1401313.

