Tinea versicolor, also known as pityriasis versicolor, is a common superficial fungal infection. It usually appears as hypopigmented, hyperpigmented, or reddish patches on the trunk and upper arms. The fungus disrupts the skin’s normal pigmentation, causing tiny, discolored spots.
The appearance of this skin condition resembles a bran-like picture, and it is thus called pityriasis. Versicolor, the second part of the name, derives from the numerous colors of the pityriasis versicolor. It is most likely to occur in females and older people. Unlike other “tinea” infections like athlete’s foot or ringworm, tinea versicolor is not caused by dermatophytes. Instead, it is caused by fungi from the Malassezia genus (formerly known as Pityrosporum).1Hainer, B. L., & Usatine, R. P. (2023). Tinea versicolor (pityriasis versicolor). In UpToDate. Retrieved June 26, 2024, from https://www.uptodate.com/contents/tinea-versicolor-pityriasis-versicolor?search=tinea%20versicolor&source=search_result&selectedTitle=1%7E26&usage_type=default&display_rank=1
Symptoms of Tinea Versicolor
Versicolor is the Latin word for “color variations.” It typically appears dark or red on light skin and light on dark skin.
- Discolored skin patches (light or dark)
- On the same patient, the appearance may vary based on body location, appearing pink/brown on the mid back and pale on the neck.
- Intense itchiness
- Growing lumps
- Skin ulcers secondary to itch
- Hair loss (if the scalp is involved)
- Swelling (if chronic)
Tinea versicolor usually involves the shoulders, mid-back, and chest and rarely goes lower down the arms. Like African Americans, facial involvement is observed in patients with darker skin tones. These spots typically affect the shoulders and trunk and may be lighter or darker than the surrounding skin. Individual lesions are generally small (e.g., <15 mm) and oval or round but frequently coalesce into larger patches or thin plaques.

How does Tinea Versicolor occur?
Tinea versicolor, caused by Malassezia, occurs when this yeast overgrows on the skin, disrupting the normal pigmentation process. The yeast interferes with normal melanin production by secreting azelaic acid, which inhibits the enzyme responsible for melanin synthesis. Consequently, areas affected by tinea versicolor display hypo- or hyperpigmentation due to this disruption of melanin production. The yeast’s overgrowth and the resultant alteration in pigmentation create the characteristic patches seen in tinea versicolor.2Hamdino, M., Saudy, A. A., El-Shahed, L. H., & Taha, M. (2022). Identification of Malassezia species isolated from some Malassezia-associated skin diseases. Journal de mycologie medicale, 32(4), 101301. https://doi.org/10.1016/j.mycmed.2022.101301
Causative Agent
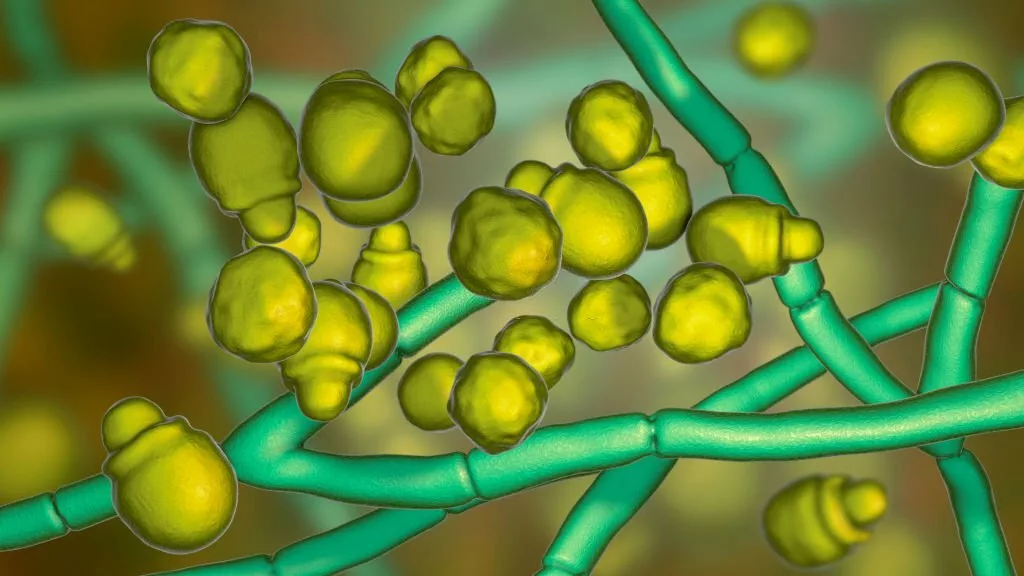
Malassezia- A Fungus:
The organisms responsible are saprophytic yeasts from the genus Malassezia (formerly known as Pityrosporum). Malassezia, a lipid-dependent and dimorphic fungus, is part of the normal skin flora. The transformation of Malassezia from yeast cells to its pathogenic, mycelial form is linked to the onset of clinical disease.3Leung, A. K., Barankin, B., Lam, J. M., Leong, K. F., & Hon, K. L. (2022). Tinea versicolor: an updated review. Drugs in Context, 11, 2022-9-2. https://doi.org/10.7573/dic.2022-9-2Malassezia live on healthy skin, therefore known as normal skin microbiome, a lipid is essential to their life.
Other Causative Agents:
Out of 14 Malassezia species, the following three are responsible for causing Pityriasis Versicolor.
- M.globosa
- M.furfur
- M.sympodialis
Malassezia typically grows sporadic in seborrheic areas (scalp, face, and chest) without producing a rash. It is unknown why they occasionally develop pityriasis versicolor on the skin’s surface more aggressively.
Risk Factors for Tinea Versicolor
The following factors may contribute to the development of Tinea Versicolor:
- Climate: Hot, humid climates have a higher prevalence of Pityriasis versicolor than cold and dry environments.
- Profession: People who sweat a lot are frequently affected.
- Dry Skin: Dry skin develops fungal infection more often than healthy moisturized skin.
- Animal Farming: If one farms different herbivores, he is at risk of Tinea Versicolor and its other types.
- Seasonal: It can go away in the winter and return every summer.
Diagnosis of Tinea Versicolor
Tinea versicolor is typically diagnosed through a combination of clinical examination and laboratory tests. A healthcare provider will first examine the affected skin physically, looking for characteristic signs of tinea versicolor.
Wood’s Lamp Test:
Yellow-green fluorescence may be seen in the damaged areas when a wood lamp (black light) is used to examine the lesion. Wood’s lamp is a particular device that can be used to diagnose a few dermatological diseases.4Moriarty, B., Hay, R., & Morris-Jones, R. (2012). The diagnosis and management of Tinea. BMJ (Clinical research ed.), 345, e4380. https://doi.org/10.1136/bmj.e4380
Dermoscopy:
Pallor, a faint pigment network in the background, and scales can be seen on a dermoscopy with pityriasis versicolor. A dermoscope is a device that noninvasively provides deep insights into skin lesions.
Fungal Smear:
A fungal smear uses potassium hydroxide (KOH) to scrape off skin cells and observe the results under a microscope — yeast cells and hyphae resembling spaghetti and meatballs. This appearance is diagnostic for tinea versicolor.
Management of Disease
Management of tinea versicolor typically involves a combination of lifestyle adjustments and medical treatments. Here are some steps for managing tinea versicolor:
Conservative Therapy:
The preferred initial treatments are topical azole antifungal drugs, topical terbinafine, and topical selenium sulfide. These therapies are generally well tolerated and have the most supporting data for their effectiveness.
- Antifungal Shampoo: Shampoo containing selenium sulfide, ketoconazole, or zinc pyrithione is usually recommended. Apply it for 5 to 10 minutes to the entire skin surface of the neck, trunk, and close extremities.5Ely, J. W., Rosenfeld, S., & Seabury Stone, M. (2014). Diagnosis and management of tinea infections. American Family Physician, 90(10), 702–710.
- Antifungal Creams: Imidazole-based antifungal creams or lotions (ciclopirox, oxiconazole, econazole, miconazole) are also a treatment line. The sole remedy for tinea versicolor that has received FDA approval is oxyconazole cream. Apply for one to four weeks, once or twice daily. Allylamines don’t work.
- Sulfate Drugs: Apply 25% sodium thiosulfate (Tinver) solution twice daily for two to four weeks. Its smell and propensity for irritation restrict use. Apply Sebulex, a sulfur-salicylic shampoo, overnight for a week.
- Salicylic Acid: Apply Salicylic acid preparations overnight for 1 to 2 weeks; they are usually effective but may irritate.
- Oral Antifungal Drugs: Ketoconazole 400 mg once every ten days or 200 mg per day, Itraconazole 200 mg once daily for seven days, Fluconazole 300 mg every week for two to four continuous weeks.6Gupta AK, Foley KA. Antifungal Treatment for Pityriasis Versicolor. J Fungi (Basel). 2015 Mar 12;1(1):13-29. doi: 10.3390/jof1010013. PMID: 29376896; PMCID: PMC5770013.
Maintenance Therapy:
Once the rash has healed, reapplying a topical remedy, such as selenium sulfide shampoo, every month will typically stop it from returning.
Dietary Recommendations:
With tinea versicolor, pay attention to diet.
- Take probiotic-supplemented food.
- Low-carb food like broccoli, green leaves, and avocado.
- Protein-rich food like chicken, meat, and beans.
- Avoid alcohol.
- Avoid sugary foods
These health guidelines assist in maintaining a healthy lifestyle and towards the cure of this disease.
Tinea Versicolor Healing Stages
The healing stages of tinea versicolor vary from person to person, but it generally follows a pattern:
Pre-Healing Stage:
Macule Formation
It appears as small, round, or oval-shaped patches on the skin. Depending on skin type and color, these patches may present from hyperpigmented lesions to somewhere between hypopigmented appearance. Lesion at this stage is called macule.
Patch Formation
When a macule increases in size, it forms patches on the body. These macules and patches have prominent demarcated borders.
Scaling & Change in Texture
Affected skin becomes scaly and dry. Scales change the texture of the skin, and the area becomes hyperpigmented or hypopigmented with reference to the surrounding skin.
Itch
Intense itchiness is not a prominent feature of tinea versicolor. It varies from person to person, depending upon the environmental factors.
Early Healing Stage:
The early healing stage starts after the initiation of treatment. Following changes usually indicate an early healing stage
- Reduction in scaling or flaking of the lesion.
- Fading of the central lesion
- The texture of the affected skin begins to resemble normal surrounding skin.
Late Healing Stage:
As the treatment process continues, the process of healing progresses with time. The following changes are significant when the lesion enters the late healing stage
- Affected patches continue to lighten and become less prominent.
- Demarcated borders lighten and gradually end up in normal skin.
- Scaling becomes mild and gradually diminishes.
- Itchiness (if present) subsidizes or completely vanishes away after treatment.
- Skin is back to its normal color as the treatment continues.
After complete treatment of tinea versicolor, the skin of the lesion becomes normal. It is important to note that healing time varies from person to person. Moreover, as per the doctor’s advice, treatment completion is important. Even if the symptoms resolve earlier, one should complete the course of medication to prevent recurrence.
Is Tinea versicolor Contagious?
Tinea versicolor may look dry and scaly, yet it is not transferred from person to person. It is treated with antifungals or anti-dandruff shampoo because the yeast grows on the skin. It may change the color of the skin, but it is not contagious.
Tinea Versicolor & Similar Diseases:
The differential diagnosis of tinea versicolor includes both common and uncommon skin disorders. A potassium hydroxide (KOH) preparation is a simple and reliable method to differentiate tinea versicolor from other conditions. Some of the conditions are discussed below:
Vitiligo
Even though Tinea can come in various colors, vitiligo and Tinea versicolor sometimes need clarification. In contrast to vitiligo, areas of tinea versicolor can also be dry and itchy. The distribution of lesions in vitiligo is often different from tinea versicolor; the macules and patches are depigmented (absence of melanin) rather than hypo- or hyperpigmented and do not have scales.
Difference in Treatment:
After treatment of Tinea versicolor with antifungal washes and ointments, the skin returns to its original tone.
Vitiligo skin darkening is more challenging to treat. While some patients choose not to get any treatment, others use topical creams and light therapy to help restore their skin’s color.
Pityriasis versicolor leaves similar post-healing plaques as vitiligo, but they are two completely different conditions.
Here are several signs that are different from pityriasis versicolor:
- Circular prominent borders, while versicolor does not show prominence borders.
- An extremely fine scale covers the spots.
- The sizes of the spots vary.
- The patches are light and don’t tan like regular skin does in the summer.
As the natural skin tone dries up in the winter, the spots seem darker (typically pink or brown) than the surrounding skin. Tinea corporis differs from pityriasis versicolor in its causing agent, signs, and symptoms, but treatment options are more or less identical.
Pityriasis Rosea:
Pityriasis Alba:
In atopic individuals, typically youngsters, pityriasis alba manifests as small, ill-defined, hypopigmented plaques with fine scales. The plaques most frequently affect the face, with sporadic involvement of the upper arms and shoulders.
Tinea Corporis:
Tinea corporis or ringworm symptoms include pruritic or asymptomatic red annular plaques with fine scales; they are often localized and can occasionally be widespread. It is more prevalent in warm, muggy settings. Adults and teenagers both suffer from the illness.7White, T. C., Findley, K., Dawson, T. L., Jr., Scheynius, A., Boekhout, T., Cuomo, C. A., Xu, J., & Saunders, C. W. (2014). Fungi on the skin: dermatophytes and Malassezia. Cold Spring Harbor Perspectives in medicine, 4(8), a019802. https://doi.org/10.1101/cshperspect.a019802

Here are several signs that are different from pityriasis versicolor:
- Circular prominent borders, while versicolor does not show prominence borders.
- An extremely fine scale covers the spots.
- The sizes of the spots vary.
- The patches are light and don’t tan like regular skin does in the summer.
- The KOH test, which shows long, thin branching hyphae or culture on Sabouraud’s medium, can confirm the diagnosis. It is uncommon to need a biopsy.
As the natural skin tone dries up in the winter, the spots seem darker (typically pink or brown) than the surrounding skin. Tinea corporis differs from pityriasis versicolor in its causing agent, signs, and symptoms, but treatment options are more or less identical.
Last but not the Least
Certainly, Malassezia species are the common cause of the superficial skin fungal illness known as pityriasis versicolor. Because tinea versicolor has many different clinical presentations, clinical expertise is crucial for diagnosing correctly. Since tinea versicolor is frequently a chronic and recurrent illness, long-term treatment regimens are sometimes mandatory. Treatment for tinea versicolor is effective with a variety of antifungal medications. Oral antifungal drugs are often the better treatment for severe and recurring diseases.
Refrences
- 1Hainer, B. L., & Usatine, R. P. (2023). Tinea versicolor (pityriasis versicolor). In UpToDate. Retrieved June 26, 2024, from https://www.uptodate.com/contents/tinea-versicolor-pityriasis-versicolor?search=tinea%20versicolor&source=search_result&selectedTitle=1%7E26&usage_type=default&display_rank=1
- 2Hamdino, M., Saudy, A. A., El-Shahed, L. H., & Taha, M. (2022). Identification of Malassezia species isolated from some Malassezia-associated skin diseases. Journal de mycologie medicale, 32(4), 101301. https://doi.org/10.1016/j.mycmed.2022.101301
- 3Leung, A. K., Barankin, B., Lam, J. M., Leong, K. F., & Hon, K. L. (2022). Tinea versicolor: an updated review. Drugs in Context, 11, 2022-9-2. https://doi.org/10.7573/dic.2022-9-2
- 4Moriarty, B., Hay, R., & Morris-Jones, R. (2012). The diagnosis and management of Tinea. BMJ (Clinical research ed.), 345, e4380. https://doi.org/10.1136/bmj.e4380
- 5Ely, J. W., Rosenfeld, S., & Seabury Stone, M. (2014). Diagnosis and management of tinea infections. American Family Physician, 90(10), 702–710.
- 6Gupta AK, Foley KA. Antifungal Treatment for Pityriasis Versicolor. J Fungi (Basel). 2015 Mar 12;1(1):13-29. doi: 10.3390/jof1010013. PMID: 29376896; PMCID: PMC5770013.
- 7White, T. C., Findley, K., Dawson, T. L., Jr., Scheynius, A., Boekhout, T., Cuomo, C. A., Xu, J., & Saunders, C. W. (2014). Fungi on the skin: dermatophytes and Malassezia. Cold Spring Harbor Perspectives in medicine, 4(8), a019802. https://doi.org/10.1101/cshperspect.a019802