Pityriasis Rosea is a skin disorder that starts with forming a scaly oval patch on your trunk and extremities. It mostly occurs in children and young adults and is a self-limiting condition, which means that it resolves on its own with time, mostly without treatment.
What is Pityriasis Rosea?
The name Pityriasis rosea means “fine pink scale,” and it is also known as Pityriasis Circinata or Roseola Annulata. It is a benign skin condition characterized by the formation of herald patches, rashes, and scales on your chest, abdomen, back, arms, or legs. The rash may or may not be itchy and typically resolves in 6-8 weeks without medication. Some people also experience prodromal symptoms before the actual disease starts. Many factors contribute to the development of this condition, such as infections and vaccines.1Litchman, G., Nair, P. A., Syed, H. A., & Le, J. K. (2024). Pityriasis Rosea. In StatPearls. StatPearls Publishing.
How common is Pityriasis Rosea?
It is a common disease with a peak incidence in the spring and winter—some regions of Australia, India, and Malaysia experience peak cases in the summer. The approximate frequency of this condition in the US is 0.13 % in females and 0.14% in males. People of all ages can get this disease if they are exposed to the risk factors. However, it affects people aged 10-35 more than infants and elders.2Joshi, T. P., Calderara, G. A., & Lipoff, J. B. (2022). Prevalence of pityriasis rosea in the United States: A cross-sectional study using the All of Us database. JAAD international, 8, 45–46. https://doi.org/10.1016/j.jdin.2022.04.006
Causes of Pityriasis Rosea
There is no clear cause of this condition, as various factors affect this disease. Some people experience it with a change of season; sometimes, it only affects certain communities in a region. These factors imply the infectious nature of pityriasis rosea.
Some important factors which play a part in causing it are:
Infections
No specific infectious agent has been singled out yet that causes pityriasis rosea. However, recent PCR reports suggest that human herpesvirus 7 and 6 might be a cause. Another probable infectious agent is the influenza virus, specifically its H1N1 strain. Some studies propose that a fungal infection is a more potent cause of pityriasis rosea rather than a viral agent, yet isolation of any fungal agent has not been achievable.3Chuh, A., Chan, H., & Zawar, V. (2004). Pityriasis rosea–evidence for and against an infectious aetiology. Epidemiology and infection, 132(3), 381–390. https://doi.org/10.1017/s0950268804002304
Vaccination
Vaccinations for smallpox, TB, polio, tetanus, hepatitis B, influenza, and yellow fever are known to start eruptions and rashes similar to pityriasis rosea. Some people also got it with certain COVID-19 vaccines.4Khattab, E., Christaki, E., & Pitsios, C. (2022). Pityriasis Rosea Induced by COVID-19 Vaccination. European journal of case reports in internal medicine, 9(2), 003164. https://doi.org/10.12890/2022_003164
Medication
One of the causes of this condition is medications and drugs. These include barbiturates, captopril, gold, isotretinoin, metronidazole, omeprazole, and ketotifen. Cancer patients who take anti-tumor necrosis factor TNF-a are also at risk of having this condition. It is not easy to clearly distinguish drug and non-drug pityriasis rosea. The only difference is that the drug-induced pityriasis rosea remains for a longer period as compared to the non-drug type.
Stages of Pityriasis Rosea
Depending upon the course of its symptoms, this condition has the following four stages:
Preliminary Stage
During this stage, you only feel the initial typical symptoms of illness, such as weakness, sore throat, and sometimes fever. It is not possible to diagnose this condition at the preliminary stage as its symptoms resemble the symptoms of a common cold.
Herald Patch Stage
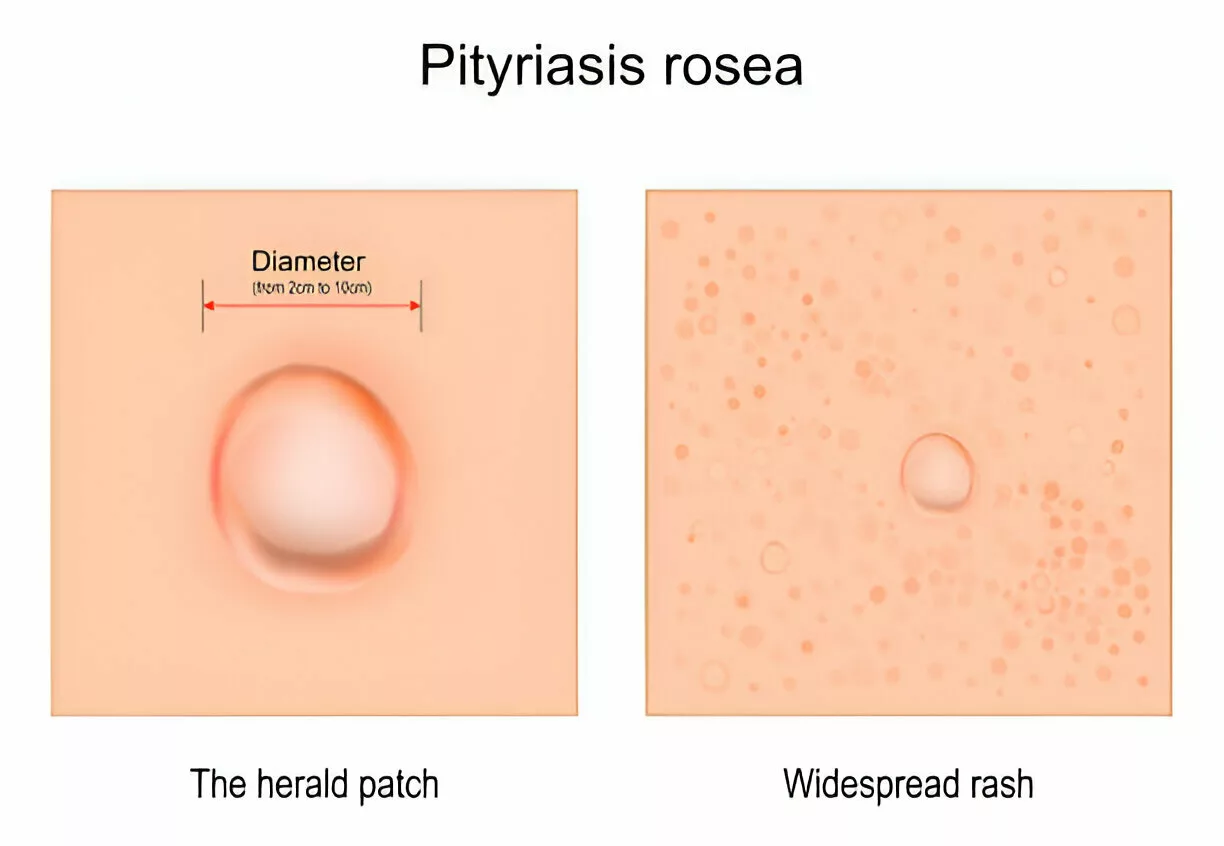
After some days, the herald patch starts to appear on your skin. It is oval and red or pink in appearance. The round shape of the herald patch closely resembles a ringworm infection. However, a herald patch typically starts from your trunk.
Rash Stage
The rash stage starts a few days after forming the herald patch. It appears as small bumps or patches alongside the herald patch. The rash can also spread to your arms and legs and can be itchy.
Resolution Stage
The resolution stage begins within six to eight weeks, and all the patches, scales, and rashes on your skin start to clear up.
Symptoms of Pityriasis Rosea
It starts with atypical symptoms such as fever, sore throat, irritability, gastrointestinal disturbance, joint pains, and flu-like illness. You may confuse these symptoms with the common cold or a viral infection.
After some days of prodromal symptoms, the appearance of a herald patch confirms the clinical diagnosis of pityriasis rosea as it is a specific finding of pityriasis rosea. The Herald patch starts as a round and oval patch typically appearing on the torso ( trunk ). The next possible site of the herald patch is your neck and proximal extremities. The color of the herald patch is red or pink, and in dark skin tones, it may appear brown or black.5Gay, J. T., Huq, M. E., Saleh, H. M., & Gross, G. P. (2024). Herald Patch. In StatPearls. StatPearls Publishing.
After the herald patch, numerous lesions or rashes appear in a series and increase in number over time. These lesions are symmetrical and bilateral and formed mainly on your upper chest, back, arms, abdomen, and some neck areas. Lesions are in the form of raised macules or papules having scales around them. The collarette appearance ( edges attached to the skin and the center lifted) of these scales is a distinguishable feature that enables them to be pointed out from other disorders. The rash of pityriasis rosea can be itchy in some cases, which, if severe, becomes an irritating and painful symptom and takes almost 6-8 weeks to fade completely.6Relhan, V., Sinha, S., Garg, V. K., & Khurana, N. (2013). Pityriasis rosea with erythema multiforme-like lesions: an observational analysis. Indian journal of dermatology, 58(3), 242. https://doi.org/10.4103/0019-5154.110855
Some people also experience pigment changes after the rash disappears. These could be hypopigmented or hyperpigmented areas on the body, and people with dark skin are most likely to get hyperpigmentation. Less than 10% of people with pityriasis rosea have also reported oral lesions such as ulcers, punctate hemorrhages, bullae, or plaques.7Urbina, F., Das, A., & Sudy, E. (2017). Clinical variants of pityriasis rosea. World journal of clinical cases, 5(6), 203–211. https://doi.org/10.12998/wjcc.v5.i6.203
Diagnose of Pityriasis Rosea
To make a complete diagnosis, the steps followed by dermatologists are:
History
If there is a suspicion of pityriasis rosea, a dermatologist must ask about the following important things:
- History of medication
- Pregnancy
- Previous history of any skin disorder
- History of upper respiratory tract infection
- Travel history
- History of itching
Physical Examination
Physical examination is important as it helps in the diagnosis of this condition.
More than 50% of the patients with this condition develop salmon pink-colored herald patches on their chest, back, or neck. The Herald patch is a distinct finding of pityriasis rosea that usually doesn’t develop in other skin disorders.
Moreover, the appearance of scales with edges attached to the skin is also a significant physical finding in Pityriasis rosea. The bilateral and diffuse distribution of scales from the trunk to the extremities resembles a Christmas tree, and it is another noteworthy finding.
Laboratory Studies
It is a clinical condition easily diagnosed through history and physical examination. However, laboratory tests are sometimes necessary to rule out other conditions.
In some patients, the count of white blood cells and ESR increase, especially if infection is the underlying cause of pityriasis rosea.
Some lesions of this condition resemble ringworm infection; a KOH test is recommended to differentiate them. Dermatologists also consider advising VDRL and rapid plasma reagin (RPR) because some cases of pityriasis rosea are closely related to the lesions of syphilis.8Halteh, P., & Lipner, S. R. (2017). A retrospective study on rapid plasma reagin testing in patients with Pityriasis rosea. International Journal of STD & AIDS, 28(13), 1348–1351. https://doi.org/10.1177/0956462417702312
COVID-19 is one of the causative factors of pityriasis rosea. Therefore, it is crucial to obtain immunohistochemistry of the CoV-2 spike protein.
Dermatoscopy
Dermatoscopy is a procedure in which dermatologists use a dermatoscope to visualize the lesions on the skin deeply. It is a microscope with a magnifying glass and a higher magnification that assesses the skin’s deeper structures and even records them for future use.
Dermatoscopy is gaining popularity in diagnosing lesions and scales in pityriasis rosea, enabling differentiation from other lesions.9Chuh A. A. (2001). Collarette scaling in pityriasis rosea demonstrated by digital epiluminescence dermatoscopy. The Australasian journal of dermatology, 42(4), 288–290. https://doi.org/10.1046/j.1440-0960.2001.00538.x

Skin Biopsy & Histopathology
Skin biopsy is useful in cases that are not yet diagnosed or lesions that are not readily differentiated. It is also valuable when lesions are not self-limited and last over three months.
A skin biopsy specimen is observed under a microscope, and it shows dermatitis in the superficial layer of your skin. In the epidermis, there is hyperplasia and spongiosis, as well as thinning of the granular layer. The dermis shows extravasation of your red blood cells and other cells, such as lymphocytes and eosinophils.10Ozyürek, G. D., Alan, S., & Cenesizoğlu, E. (2014). Evaluation of clinical-epidemiological and histopathological features of pityriasis rosea. Postepy dermatologii i alergologii, 31(4), 216–221. https://doi.org/10.5114/pdia.2014.40641
Treatment & Management
The treatment of pityriasis is mainly based on supportive care as it is a self-limited disease that resolves on its own with no complications in almost 6-8 weeks. However, the symptomatic treatment of pityriasis rosea promises a good outcome.
Avoidance of Triggering Factors
It is necessary to avoid the factors causing this condition. In the early stage of the disease, when the triggering factor is not yet analyzed, you should avoid hot water, sweat, fragrances, and irritating soaps.
Treatment of Pruritus
Topical calamine lotions and zinc oxide are particularly helpful for pruritus (itching). Doctors also prescribe oral antihistamines (Diphenhydramine or Hydroxyzine) and emollients for the pruritus associated with pityriasis rosea.
Steroids
Systemic steroids are usually not advised in pityriasis rosea as they are notorious for exacerbating the symptoms. However, skin specialists may advise you to take a small dose of prednisolone (0.5-1 mg/kg/day) for 5 days if you are experiencing severe itching, blisters all over the body, or hyperpigmented patches. Moreover, topical steroids such as betamethasone and hydrocortisone are also useful in alleviating severe rash in pityriasis rosea.

Phototherapy
Phototherapy is also a well-known option for treating resistant pruritus in pityriasis rosea. A commonly used phototherapy is UV-B, and its dose can be increased if symptoms don’t subside with a low dose. In addition to treating pruritus, light therapy also reduces pigmentation in a resolved case of pityriasis rosea.11Lim, S. H., Kim, S. M., Oh, B. H., Ko, J. H., Lee, Y. W., Choe, Y. B., & Ahn, K. J. (2009). Low-dose Ultraviolet A1 Phototherapy for Treating Pityriasis Rosea. Annals of Dermatology, 21(3), 230–236. https://doi.org/10.5021/ad.2009.21.3.230

Antiviral & Antibiotic Medications
As viral agents are a factor in causing pityriasis rosea, doctors may also prescribe 1g acyclovir to some patients in the initial stages of the disease, which aids in reducing the duration of the disease. 12Rodriguez-Zuniga, M., Torres, N., & Garcia-Perdomo, H. (2018). Effectiveness of acyclovir in the treatment of pityriasis rosea: A systematic review and meta-analysis. Anais brasileiros de dermatologia, 93(5), 686–695. https://doi.org/10.1590/abd1806-4841.20187252
Some patients also benefit from taking 1g of oral erythromycin 4 times a day for 2 weeks.13Drago, F., & Rebora, A. (2009). Treatments for pityriasis rosea. Skin therapy letter, 14(3), 6–7.
Is Pityriasis Rosea Contagious?
It spreads from one point of your body to the whole body and settles on its own in weeks. Nonetheless, PR is not a contagious disease, which implies that it can not spread from an infected person to a healthy person.
How can I prevent Pityriasis Rosea?
It does not have a specific causative factor, so it is not easy to prevent it. However, you can control the course of the disease by taking some precautionary measures. Avoid soaps and body sprays that contain irritant ingredients. Some people get rash from hot water and sweating, so these factors must be avoided. It would help if you stayed away from dust and dirt as it may contain viral or fungal agents. If you are taking some medicines, it is better to stop taking them to slow down the course of this condition.
Pityriasis Rosea vs Tinea Versicolor
Both of these conditions are skin disorders, but they have several differences.
PR mainly presents as a single patch on your back and chest and then spreads to your arms and legs with time, but tinea versicolor presents as several pigmented patches on your trunk and shoulder.
Tinea versicolor is a fungal disease caused by the excessive growth of a fungus normally residing in your skin. However, a definite cause of pityriasis rosea has not been identified yet.
In tinea versicolor, doctors advise staying indoors to avoid sunlight, as it exacerbates the appearance of patches. In pityriasis roses, no specific precaution is needed. Similarly, pityriasis rosea does not require medication in minor cases, while in tinea versicolor, you must take prescribed antifungal medications.

Prognosis of Pityriasis Rosea
It has an excellent prognosis because the lesions settle down in some weeks without any sequelae, even if one takes no medication.
Conclusion
In conclusion, this self-limiting skin disorder starts with a herald patch on your back, chest, or neck and eventually spreads over time on your extremities. Infection, vaccinations, and some medications can lead to this condition. You don’t need medication in minor cases, but you can take antihistamines to reduce itching. Avoid triggering factors like water, sweat, and soap. The prognosis is good, but without proper care, you might experience pigment changes after the lesions subside.
Refrences
- 1Litchman, G., Nair, P. A., Syed, H. A., & Le, J. K. (2024). Pityriasis Rosea. In StatPearls. StatPearls Publishing.
- 2Joshi, T. P., Calderara, G. A., & Lipoff, J. B. (2022). Prevalence of pityriasis rosea in the United States: A cross-sectional study using the All of Us database. JAAD international, 8, 45–46. https://doi.org/10.1016/j.jdin.2022.04.006
- 3Chuh, A., Chan, H., & Zawar, V. (2004). Pityriasis rosea–evidence for and against an infectious aetiology. Epidemiology and infection, 132(3), 381–390. https://doi.org/10.1017/s0950268804002304
- 4Khattab, E., Christaki, E., & Pitsios, C. (2022). Pityriasis Rosea Induced by COVID-19 Vaccination. European journal of case reports in internal medicine, 9(2), 003164. https://doi.org/10.12890/2022_003164
- 5Gay, J. T., Huq, M. E., Saleh, H. M., & Gross, G. P. (2024). Herald Patch. In StatPearls. StatPearls Publishing.
- 6Relhan, V., Sinha, S., Garg, V. K., & Khurana, N. (2013). Pityriasis rosea with erythema multiforme-like lesions: an observational analysis. Indian journal of dermatology, 58(3), 242. https://doi.org/10.4103/0019-5154.110855
- 7Urbina, F., Das, A., & Sudy, E. (2017). Clinical variants of pityriasis rosea. World journal of clinical cases, 5(6), 203–211. https://doi.org/10.12998/wjcc.v5.i6.203
- 8Halteh, P., & Lipner, S. R. (2017). A retrospective study on rapid plasma reagin testing in patients with Pityriasis rosea. International Journal of STD & AIDS, 28(13), 1348–1351. https://doi.org/10.1177/0956462417702312
- 9Chuh A. A. (2001). Collarette scaling in pityriasis rosea demonstrated by digital epiluminescence dermatoscopy. The Australasian journal of dermatology, 42(4), 288–290. https://doi.org/10.1046/j.1440-0960.2001.00538.x
- 10Ozyürek, G. D., Alan, S., & Cenesizoğlu, E. (2014). Evaluation of clinical-epidemiological and histopathological features of pityriasis rosea. Postepy dermatologii i alergologii, 31(4), 216–221. https://doi.org/10.5114/pdia.2014.40641
- 11Lim, S. H., Kim, S. M., Oh, B. H., Ko, J. H., Lee, Y. W., Choe, Y. B., & Ahn, K. J. (2009). Low-dose Ultraviolet A1 Phototherapy for Treating Pityriasis Rosea. Annals of Dermatology, 21(3), 230–236. https://doi.org/10.5021/ad.2009.21.3.230
- 12Rodriguez-Zuniga, M., Torres, N., & Garcia-Perdomo, H. (2018). Effectiveness of acyclovir in the treatment of pityriasis rosea: A systematic review and meta-analysis. Anais brasileiros de dermatologia, 93(5), 686–695. https://doi.org/10.1590/abd1806-4841.20187252
- 13Drago, F., & Rebora, A. (2009). Treatments for pityriasis rosea. Skin therapy letter, 14(3), 6–7.