Stevens-Johnson Syndrome (SJS) is a rare but life-threatening hypersensitivity reaction, most commonly triggered by medications. It ranks among the most severe dermatologic emergencies, with the disease process primarily involving the skin and mucous membranes. The illness typically begins with vague flu-like symptoms and progresses rapidly. In SJS, necrosis (cell death) causes the epidermis to detach from the dermis, leading to characteristic skin peeling and extensive wounds that expose the underlying tissue.1 Shah, H., Parisi, R., Mukherjee, E., Phillips, E. J., & Dodiuk-Gad, R. P. (2024). Update on Stevens–Johnson Syndrome and toxic epidermal necrolysis: Diagnosis and management. American Journal of Clinical Dermatology, 25(6), 891–908. https://doi.org/10.1007/s40257-024-00889-6
SJS only affects 1–12 people per million annually, but it cannot be ignored.2Saeed, H. N., Micheletti, R., & Phillips, E. J. (2024). Editorial: Stevens Johnson syndrome: Past, present, and future directions. Frontiers in Medicine, 11, 1383891. https://doi.org/10.3389/fmed.2024.1383891 In fact, without treatment, the condition can lead to infection, multi-organ damage, and even death.
Causes and Risk Factors of Stevens-Johnson Syndrome
- 80% of SJS cases are drug-induced, with antibiotics (e.g., sulfonamides), anticonvulsants (e.g., phenytoin), nonsteroidal anti-inflammatory drugs (NSAIDs) (e.g., ibuprofen), and allopurinol being common triggers. The reaction usually develops within the first few weeks of starting a new drug.3Saeed, H. N., Micheletti, R., & Phillips, E. J. (2024). Editorial: Stevens Johnson syndrome: Past, present, and future directions. Frontiers in Medicine, 11, 1383891. https://doi.org/10.3389/fmed.2024.1383891
- Infections can also be a trigger, especially Mycoplasma pneumoniae. Viral infections like herpes simplex or hepatitis have also been associated, though less commonly.
- Occasionally, no cause is found at all. In these cases, it’s called idiopathic.
Risk Factors for SJS
In many cases, individual susceptibility plays a role. People with certain genetic markers (like HLA-B15:02 and HLA-B58:01, especially among Southeast Asian populations) are at higher risk of severe reactions to specific drugs.
Other key risk factors include:
- HIV infection: Patients with human immunodeficiency virus (HIV) infection have a greater risk of SJS/TEN.4Sekula P, Dunant A, Mockenhaupt M, Naldi L, Bouwes Bavinck JN, Halevy S, Kardaun S, Sidoroff A, Liss Y, Schumacher M, Roujeau JC; RegiSCAR study group. Comprehensive survival analysis of a cohort of patients with Stevens-Johnson syndrome and toxic epidermal necrolysis. J Invest Dermatol. 2013 May;133(5):1197-204. doi: 10.1038/jid.2012.510. Epub 2013 Feb 7. PMID: 23389396.
- Cancer, organ transplantation, or immunosuppressive therapy
- Age-related vulnerability: Those aged 20 to 40 years are most likely to develop the condition. Children most commonly develop SJS secondary to infection. Older adults are at risk because of polypharmacy and comorbid conditions.

Stevens-Johnson Syndrome (SJS) vs Toxic Epidermal Necrolysis (TEN)
Technically, no—they are not separate diseases but rather two ends of the same spectrum of severe mucocutaneous reactions, most commonly triggered by medications. They differ only in the total body surface area affected:
- SJS: less than 10% of total body surface area (TBSA)
- TEN: greater than 30% of total body surface area (TBSA)
- Between 10% and 30% is called SJS-TEN overlap.5Zimmerman, D., & Dang, N. H. (2020). Stevens–Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN). In J. Nates & K. Price (Eds.), Oncologic critical care (pp. 267–280). Springer. https://doi.org/10.1007/978-3-319-74588-6_195
The pathology and mechanism are the same. TEN is more extensive and dangerous compared to SJS, and has a higher mortality (25–35%), but many clinicians consider them to be minor variations of the same disease rather than different diseases themselves.
How common is Stevens-Johnson Syndrome?
Overall, SJS and TEN are quite uncommon diseases across the world. They affect an average of 1 to 12 people per million every year. In the U.S., each year, about 5.3 out of every million children develop SJS, 0.8 develop SJS/TEN overlap, and 0.4 develop TEN.6Hsu DY, Brieva J, Silverberg NB, Paller AS, Silverberg JI. Pediatric Stevens-Johnson syndrome and toxic epidermal necrolysis in the United States. J Am Acad Dermatol. 2017 May;76(5):811-817.e4. doi: 10.1016/j.jaad.2016.12.024. Epub 2017 Mar 9. PMID: 28285784; PMCID: PMC5502094.
A study based on French national data (2013–2022) found that around 2.6 people per million are affected annually.7Bettuzzi T, Lebrun-Vignes B, Ingen-Housz-Oro S, Sbidian E. Incidence, In-Hospital and Long-Term Mortality, and Sequelae of Epidermal Necrolysis in Adults. JAMA Dermatol. 2024 Dec 1;160(12):1288-1296. doi: 10.1001/jamadermatol.2024.3575. PMID: 39356525; PMCID: PMC11447629.
However, this number differs widely by geography, genetics, and other risk factors that change between regions and populations. Some sites and groups of people have a much higher risk of developing SJS or TEN.
How does SJS happen – Pathogenesis
SJS and TEN happen when the immune system mistakenly attacks the skin, usually triggered by certain drugs. In about 15% of cases, no clear cause is found, but hidden exposures might play a role.
The reaction starts when specific drugs interact with genetic markers called HLA, activating immune cells (CD8+ T cells). These cells release toxic proteins that kill skin cells, causing blistering and peeling. The skin damage is mainly caused by toxic proteins like granulysin, leading to widespread skin cell death. Besides apoptosis (programmed cell death), other forms of cell death may also be involved.
Cytokines such as TNF-alpha and IL-15 increase inflammation and disease severity. New treatments might target immune pathways like JAK/STAT to help control the disease.
Signs & Symptoms of Stevens-Johnson Syndrome
Prodromal Symptoms
Stevens-Johnson syndrome (SJS) often begins with flu-like prodromal symptoms:
- Fever
- Sore throat
- Fatigue
- Red, watery eyes (Conjunctivitis)
- Body aches8Noe, M. H., & Micheletti, R. G. (2020). Diagnosis and management of Stevens-Johnson syndrome/toxic epidermal necrolysis. Clinics in Dermatology, 38(6), 607-612. https://doi.org/10.1016/j.clindermatol.2020.06.016
These symptoms usually appear before or alongside skin and mucous membrane involvement. Within a few days, the symptoms get worse.
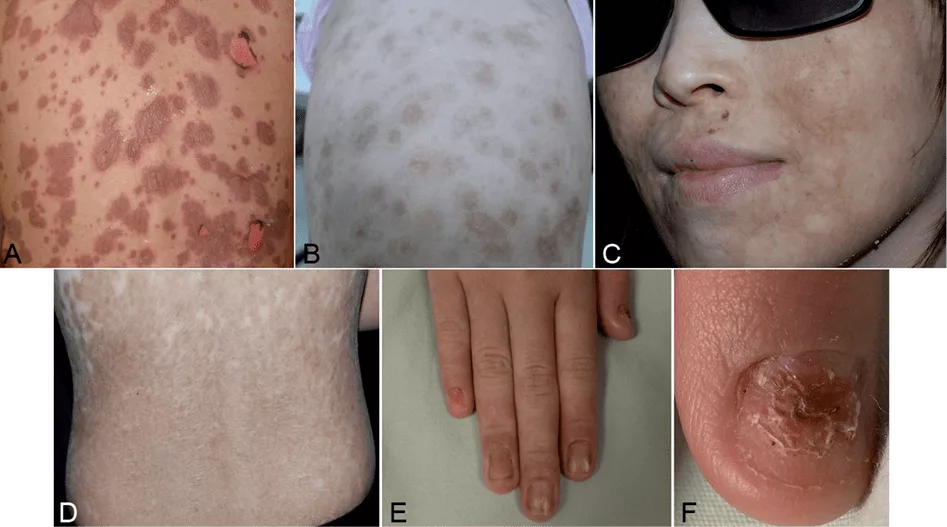
Cutaneous Manifestations
The skin rash typically starts on the face and upper body and then spreads symmetrically. Early signs include:
- Red patches that are poorly defined (erythematous macules)
- Dusky red areas with purplish spots
- Atypical target-like lesions (two rings instead of three)
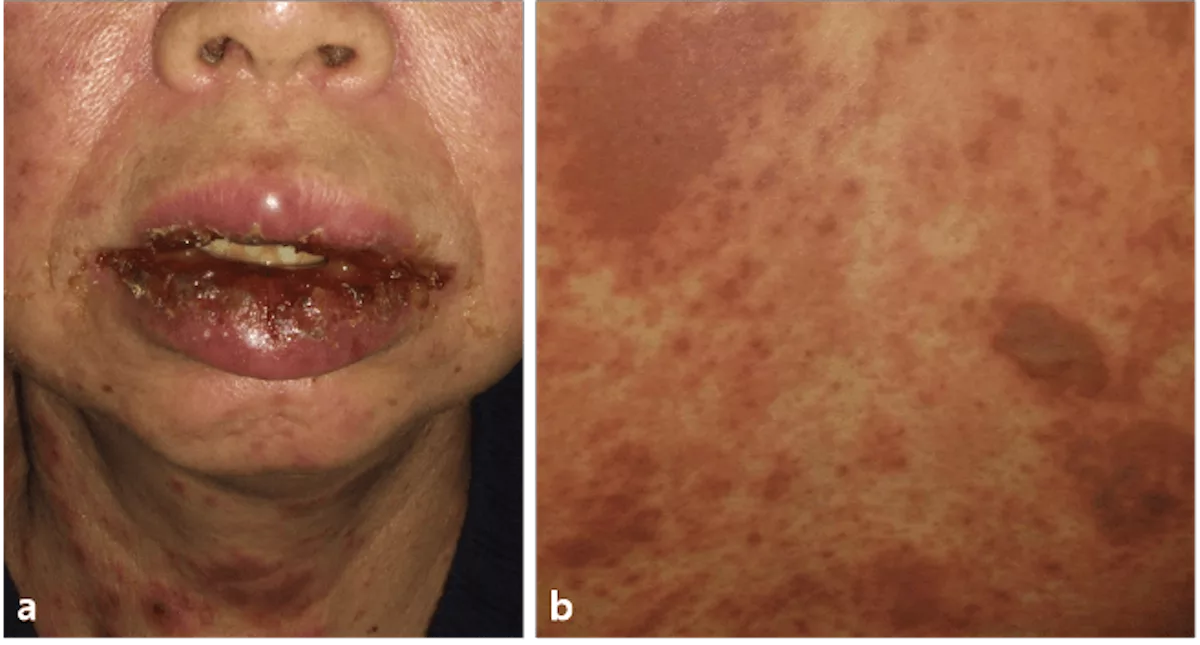
- Blisters on the inside of the mouth, throat, or eyes, and later in the genital area, making it hard to drink, eat, or even pee. These blisters are fragile.
- The skin becomes very tender, and gentle pressure can cause the outer layer to peel away—a positive Nikolsky sign, similar to severe burns.
- Crusting and swelling of the lips and eyes.9Zimmerman, D., & Dang, N. H. (2020). Stevens–Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN). In J. Nates & K. Price (Eds.), Oncologic critical care (pp. 267–280). Springer. https://doi.org/10.1007/978-3-319-74588-6_195
The acute phase usually lasts about one week, followed by skin healing over two to three weeks. During this time, patients are at risk for fluid loss and electrolyte imbalances.
Why is Stevens-Johnson Syndrome so dangerous?
In SJS, the outer layer of the skin dies and sloughs off, leaving bare tissue open to infection and dehydration. With a 5–10% death rate (higher in TEN), complications may include sepsis, multi-system organ failure, blindness, and scarring.10Wasuwanich, P., So, J. M., Chakrala, T. S., Chen, J., & Motaparthi, K. (2023). Epidemiology of Stevens-Johnson syndrome and toxic epidermal necrolysis in the United States and factors predictive of outcome. JAAD International, 13, 17. https://doi.org/10.1016/j.jdin.2023.06.014 Patients usually require an immediate hospital and burn unit admission.
Diagnosis of Stevens-Johnson Syndrome
There is no diagnostic test for SJS. As time is of the essence, doctors typically rely on a combination of their clinical judgement, history taking, and supportive tests to make the diagnosis quickly.
Clinical Evaluation:
- History of recent drug intake (within the last 1–3 weeks)
- Onset of symptoms: Did flu-like symptoms come first? Was there rapid skin involvement?
- Visible skin lesions- extensive red or purplish skin patches, blisters, and skin peeling
- The Nikolsky sign (skin slips off when lightly rubbed)
- Mucosal involvement (involvement of the mouth, eyes, genitals)11Zimmerman, D., & Dang, N. H. (2020). Stevens–Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN). In J. Nates & K. Price (Eds.), Oncologic critical care (pp. 267–280). Springer. https://doi.org/10.1007/978-3-319-74588-6_195
It is important to differentiate Stevens-Johnson syndrome from other blistering diseases such as dystrophic epidermolysis bullosa—a genetic disorder characterized by fragile skin—and pemphigus vulgaris, an autoimmune blistering condition. These disorders have different clinical courses and require distinct management approaches.
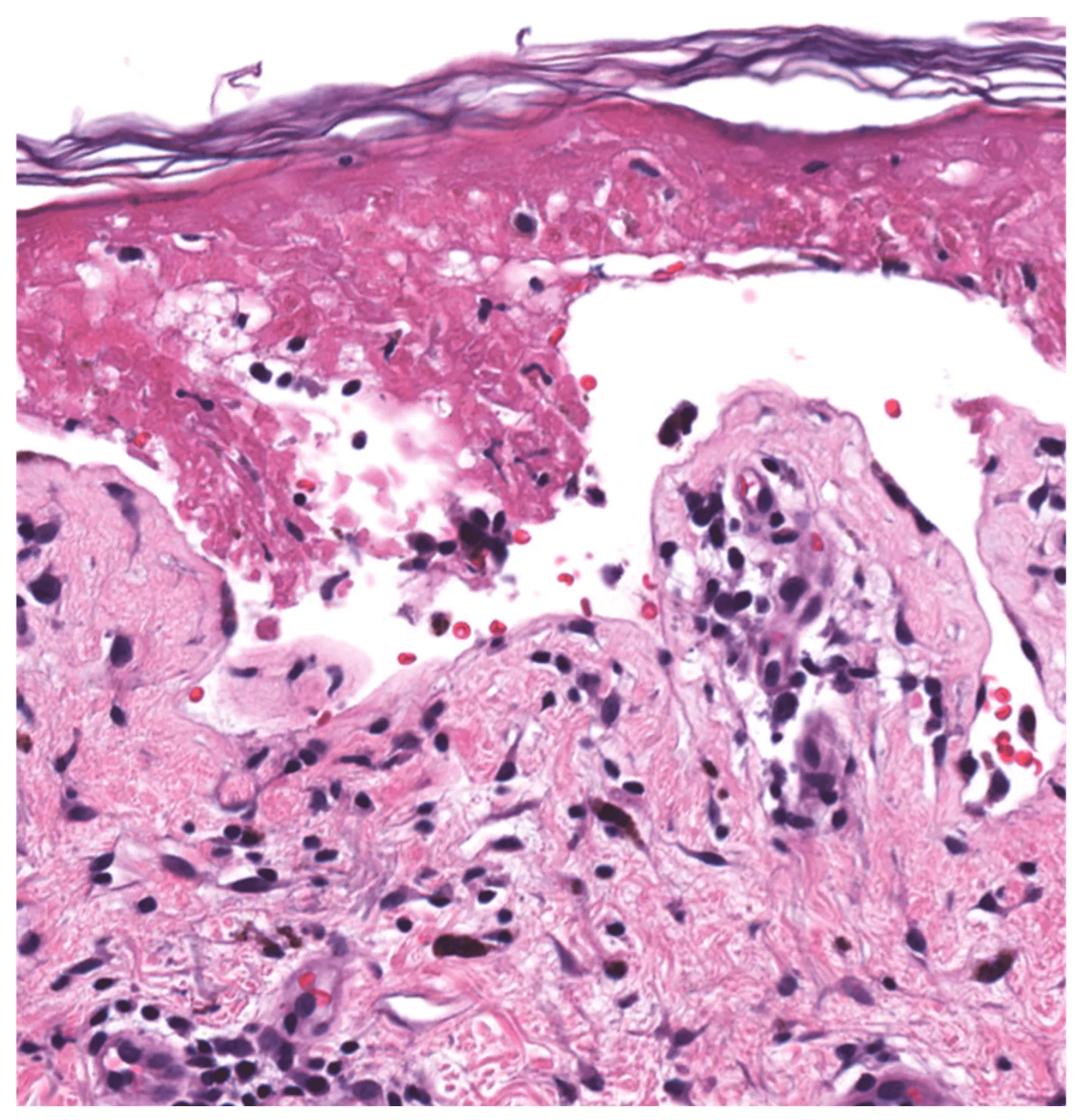
Skin Biopsy:
When doctors want to be absolutely sure, or rule out other conditions (like bullous pemphigoid or staphylococcal scalded skin syndrome), they may do a skin biopsy. It can show:
- Full-thickness epidermal necrosis (cell death)
- Epidermal detachment
- Minimal immune cell infiltration (helps rule out autoimmune conditions)12Frantz, R., Huang, S., Are, A., & Motaparthi, K. (2021). Stevens–Johnson Syndrome and Toxic Epidermal Necrolysis: A Review of Diagnosis and Management. Medicina, 57(9), 895. https://doi.org/10.3390/medicina57090895
Blood Tests:
Blood tests can assess the severity, monitor complications, and rule out similar conditions:
- Complete Blood Count (CBC): Signs of infection, anemia, or low platelet count
- Liver Function Tests (LFTs): Elevated enzymes like ALT/AST may suggest liver involvement
- Renal Function Tests: Increased creatinine and BUN can show decreased kidney filtration, important in cases of dehydration, sepsis
- Electrolytes: Skin loss and poor intake can lead to sodium or potassium imbalances
- Inflammatory Markers (CRP, ESR): Elevated in severe systemic inflammation
- Blood Cultures: Ordered if there’s fever, to rule out sepsis (a life-threatening complication)
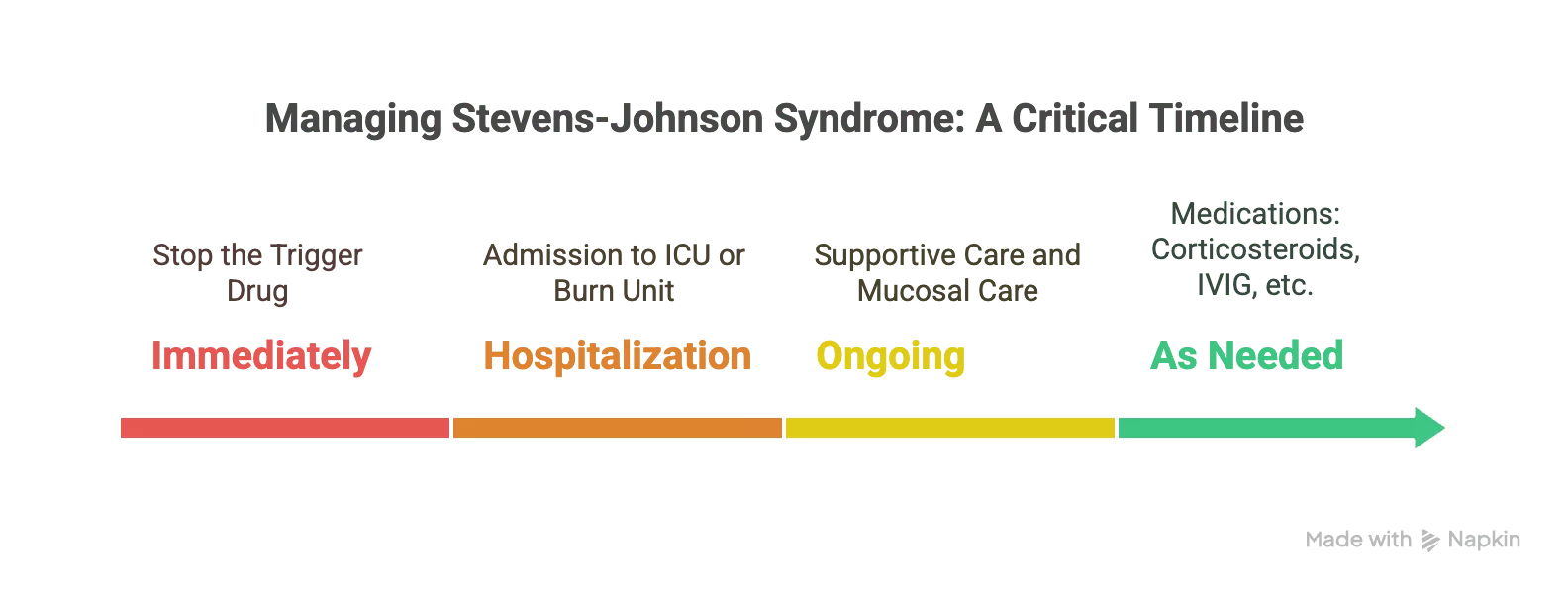
Treatment of Stevens-Johnson Syndrome
Treating SJS is a medical emergency. The goal is to stop the damage, manage symptoms, and prevent complications.13Frantz, R., Huang, S., Are, A., & Motaparthi, K. (2021). Stevens–Johnson Syndrome and Toxic Epidermal Necrolysis: A Review of Diagnosis and Management. Medicina, 57(9), 895. https://doi.org/10.3390/medicina57090895
Step 1: Stop the Trigger Drug (Immediately):
This is priority number one. If a medication is suspected (and it usually is), it must be stopped immediately. One extra dose can make things worse.
Step 2: Hospitalization in a Specialized Unit:
Patients with SJS are usually admitted to an ICU or burn unit because:
- Their skin is compromised like a burn injury
- Fluid loss, electrolyte imbalance, and infections are serious risks
- They need expert wound care
Step 3: Supportive Care (The Backbone of Treatment):
Supportive care includes:
- Replacement for fluid and electrolyte loss
- Nutritional support (often through a feeding)
- Pain management (IV opioids or other pain meds)
- Wound care (non-adhesive dressings, gentle cleaning)
Mucosal Care:
Special attention is given to eyes, mouth, and genitals:
- Ophthalmology consults early to prevent long-term vision issues
- Topical treatments for oral and genital lesions to reduce pain and scarring
Medications: Still Controversial:
Several medications are used in some cases, but their effectiveness is debated. These include:
- Corticosteroids (to reduce inflammation) — helpful in early stages, but risky if there’s an infection
- IVIG (Intravenous Immunoglobulin): Can halt disease progression by blocking Fas-mediated cell death
- Cyclosporine or TNF-alpha inhibitors: Occasionally used in severe, unresponsive cases
Treatment decisions vary depending on the patient’s condition and hospital protocols.
What are the Complications?
SJS has systemic complications and can be life-threatening:
- Sepsis: Open skin = infection risk = potentially fatal
- Dehydration & Electrolyte Imbalance
- Acute respiratory distress syndrome (ARDS): Especially if lung tissue is involved
- Chronic eye issues: Dry eyes, scarring, even blindness
- Skin changes: Scarring, pigmentation changes, and sensitivity
- Psychological impact: Especially in children and young adults—trauma, anxiety, PTSD14Hasegawa, A., & Abe, R. (2020). Recent advances in managing and understanding Stevens-Johnson syndrome and toxic epidermal necrolysis. F1000Research, 9, F1000 Faculty Rev-612. https://doi.org/10.12688/f1000research.24748.1
Recovery from Stevens-Johnson Syndrome
Recovery from SJS is slow and depends upon severity, age, and overall health. The skin often heals over weeks, but complications, such as scarring, chronic eye issues, and mucosal damage, can last much longer. Emotional recovery is also a real part of the journey.
The prognosis varies: for SJS, the mortality is said to be around 5–10%, however, TEN has a higher mortality, often greater than 30%, although it can vary widely.15Frantz, R., Huang, S., Are, A., & Motaparthi, K. (2021). Stevens–Johnson Syndrome and Toxic Epidermal Necrolysis: A Review of Diagnosis and Management. Medicina, 57(9), 895. https://doi.org/10.3390/medicina57090895
The SCORTEN system can help clinicians evaluate the severity of the disease. The SCORTEN score is used to predict the likelihood of all-cause mortality in patients with SJS or TEN based on the following parameters: age, presence of cancer, heart rate, and serum lab values.16Frantz, R., Huang, S., Are, A., & Motaparthi, K. (2021). Stevens–Johnson Syndrome and Toxic Epidermal Necrolysis: A Review of Diagnosis and Management. Medicina, 57(9), 895. https://doi.org/10.3390/medicina57090895
| Parameter | Weight |
|---|---|
| Age ≥ 40 years | 1 |
| Malignancy—Yes | 1 |
| BSA detached > 10% | 1 |
| Serum bicarbonate < 20 mmol/L | 1 |
| Serum urea nitrogen > 28 mg/dL | 1 |
| Serum glucose > 252 mg/dL | 1 |
| Tachycardia ≥ 120 bpm | 1 |
A higher SCORTEN score is associated with a higher likelihood of death and can be helpful for clinicians to make decisions about how aggressively to manage these patients.
| SCORTEN Score | Estimated Mortality (%) |
|---|---|
| 0-1 | 3.2 |
| 2 | 12.1 |
| 3 | 35.3 |
| 4 | 58.3 |
| >5 | 90 |
Early diagnosis, immediate withdrawal of the offending drug, and intensive supportive care significantly improve outcomes. Survivors usually require long-term follow-up and must avoid the trigger medication for life.
Red Man Syndrome vs. Stevens-Johnson Syndrome (SJS)
| Red Man Syndrome (now Vancomycin Infusion Reaction)17Martel, T. J., Jamil, R. T., & Afzal, M. (2025). Vancomycin infusion reaction. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482506/ | Stevens-Johnson Syndrome (SJS) | |
|---|---|---|
| Cause | Infusion reaction (not allergy), usually vancomycin | Severe hypersensitivity reaction to medications or infections |
| Onset | Minutes after starting IV infusion | Days to weeks after drug exposure |
| Common Triggers | Rapid vancomycin infusion | Antibiotics, anti-epileptics, NSAIDs, infections |
| Symptoms | Flushing, redness (face/neck), itching, ± low BP | Fever, sore throat, painful rash, blisters, skin peeling |
| Mucosal Involvement | No | Yes – mouth, eyes, genitals |
| Skin Detachment | No | Yes, extensive in severe cases |
| Severity | Mild to moderate (self-limiting) | Severe, life-threatening |
| Treatment | Slow infusion, antihistamines, supportive care | Immediate drug withdrawal, ICU care, wound management |
| Prognosis | Excellent with proper management | Variable; mortality rate 10–30% depending on severity |
Conclusion
Stevens-Johnson Syndrome is rare but relentless — a reminder of how fragile and fierce the human body can be in the face of hypersensitivity. Whether you’re a patient navigating recovery or a clinician racing to intervene, early recognition and the right response can make all the difference. Education, vigilance, and empathy remain our best defense because in conditions like SJS, timing is everything.
Refrences
- 1Shah, H., Parisi, R., Mukherjee, E., Phillips, E. J., & Dodiuk-Gad, R. P. (2024). Update on Stevens–Johnson Syndrome and toxic epidermal necrolysis: Diagnosis and management. American Journal of Clinical Dermatology, 25(6), 891–908. https://doi.org/10.1007/s40257-024-00889-6
- 2Saeed, H. N., Micheletti, R., & Phillips, E. J. (2024). Editorial: Stevens Johnson syndrome: Past, present, and future directions. Frontiers in Medicine, 11, 1383891. https://doi.org/10.3389/fmed.2024.1383891
- 3Saeed, H. N., Micheletti, R., & Phillips, E. J. (2024). Editorial: Stevens Johnson syndrome: Past, present, and future directions. Frontiers in Medicine, 11, 1383891. https://doi.org/10.3389/fmed.2024.1383891
- 4Sekula P, Dunant A, Mockenhaupt M, Naldi L, Bouwes Bavinck JN, Halevy S, Kardaun S, Sidoroff A, Liss Y, Schumacher M, Roujeau JC; RegiSCAR study group. Comprehensive survival analysis of a cohort of patients with Stevens-Johnson syndrome and toxic epidermal necrolysis. J Invest Dermatol. 2013 May;133(5):1197-204. doi: 10.1038/jid.2012.510. Epub 2013 Feb 7. PMID: 23389396.
- 5Zimmerman, D., & Dang, N. H. (2020). Stevens–Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN). In J. Nates & K. Price (Eds.), Oncologic critical care (pp. 267–280). Springer. https://doi.org/10.1007/978-3-319-74588-6_195
- 6Hsu DY, Brieva J, Silverberg NB, Paller AS, Silverberg JI. Pediatric Stevens-Johnson syndrome and toxic epidermal necrolysis in the United States. J Am Acad Dermatol. 2017 May;76(5):811-817.e4. doi: 10.1016/j.jaad.2016.12.024. Epub 2017 Mar 9. PMID: 28285784; PMCID: PMC5502094.
- 7Bettuzzi T, Lebrun-Vignes B, Ingen-Housz-Oro S, Sbidian E. Incidence, In-Hospital and Long-Term Mortality, and Sequelae of Epidermal Necrolysis in Adults. JAMA Dermatol. 2024 Dec 1;160(12):1288-1296. doi: 10.1001/jamadermatol.2024.3575. PMID: 39356525; PMCID: PMC11447629.
- 8Noe, M. H., & Micheletti, R. G. (2020). Diagnosis and management of Stevens-Johnson syndrome/toxic epidermal necrolysis. Clinics in Dermatology, 38(6), 607-612. https://doi.org/10.1016/j.clindermatol.2020.06.016
- 9Zimmerman, D., & Dang, N. H. (2020). Stevens–Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN). In J. Nates & K. Price (Eds.), Oncologic critical care (pp. 267–280). Springer. https://doi.org/10.1007/978-3-319-74588-6_195
- 10Wasuwanich, P., So, J. M., Chakrala, T. S., Chen, J., & Motaparthi, K. (2023). Epidemiology of Stevens-Johnson syndrome and toxic epidermal necrolysis in the United States and factors predictive of outcome. JAAD International, 13, 17. https://doi.org/10.1016/j.jdin.2023.06.014
- 11Zimmerman, D., & Dang, N. H. (2020). Stevens–Johnson syndrome (SJS) and toxic epidermal necrolysis (TEN). In J. Nates & K. Price (Eds.), Oncologic critical care (pp. 267–280). Springer. https://doi.org/10.1007/978-3-319-74588-6_195
- 12Frantz, R., Huang, S., Are, A., & Motaparthi, K. (2021). Stevens–Johnson Syndrome and Toxic Epidermal Necrolysis: A Review of Diagnosis and Management. Medicina, 57(9), 895. https://doi.org/10.3390/medicina57090895
- 13Frantz, R., Huang, S., Are, A., & Motaparthi, K. (2021). Stevens–Johnson Syndrome and Toxic Epidermal Necrolysis: A Review of Diagnosis and Management. Medicina, 57(9), 895. https://doi.org/10.3390/medicina57090895
- 14Hasegawa, A., & Abe, R. (2020). Recent advances in managing and understanding Stevens-Johnson syndrome and toxic epidermal necrolysis. F1000Research, 9, F1000 Faculty Rev-612. https://doi.org/10.12688/f1000research.24748.1
- 15Frantz, R., Huang, S., Are, A., & Motaparthi, K. (2021). Stevens–Johnson Syndrome and Toxic Epidermal Necrolysis: A Review of Diagnosis and Management. Medicina, 57(9), 895. https://doi.org/10.3390/medicina57090895
- 16Frantz, R., Huang, S., Are, A., & Motaparthi, K. (2021). Stevens–Johnson Syndrome and Toxic Epidermal Necrolysis: A Review of Diagnosis and Management. Medicina, 57(9), 895. https://doi.org/10.3390/medicina57090895
- 17Martel, T. J., Jamil, R. T., & Afzal, M. (2025). Vancomycin infusion reaction. In StatPearls. StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK482506/





