Lupus vasculitis is an inflammatory complication of systemic lupus erythematosus or SLE. It occurs when your body’s immune system mistakenly causes inflammation in your blood vessels. This happens in multiple organ systems, but especially affects your skin. Lupus vasculitis can cause permanent damage if left unmanaged.
What is Lupus Vasculitis?
SLE is a chronic autoimmune disorder in which your immune system starts attacking your own organs. Like other tissues, lupus can also attack the blood vessels present all over your body. This results in their inflammation and is called lupus vasculitis.
Lupus vasculitis has been seen in as many as 50% of patients who have SLE. It affects all kinds of vessels — small, medium, or large. It can cause a wide range of issues, from mild skin rashes to cerebrovascular accidents.1Gamal, S. M., Mohamed, S. S., Tantawy, M., Siam, I., Soliman, A., & Niazy, M. H. (2021). Lupus-related vasculitis in a cohort of systemic lupus erythematosus patients. Archives of Rheumatology, 36(4), 595–692. https://doi.org/10.46497/archrheumatol.2021.8804
Risk Factors of Lupus Vasculitis
Like other manifestations of lupus, lupus vasculitis is linked to certain “triggers” and risk factors that can influence when it starts and how severe it becomes. These include:
- Uncontrolled or severe lupus
- Low C3 and C4 complement levels
- High levels of antibodies, especially anti-dsDNA
- Infections
- Genetic predisposition
- Family history of autoimmune disease
- Smoking
- Being female
- Lupus at a young age
- Previous history of vasculitis
- Medications such as hydralazine and minocycline
- Exposure to ultraviolet radiation
- High physical or psychological stress2Saleh, A., Yee, C.-S., Acquah, A., Gordon, C., & Reynolds, J. A. (2024). Cutaneous vasculitis in systemic lupus erythematosus: epidemiology and risk factors over a 20-year follow-up. Lara D. Veeken. https://doi.org/10.1093/rheumatology/keae672
What actually causes Lupus Vasculitis?
Lupus vasculitis occurs when your immune system starts attacking your own blood vessels. The exact pathogenesis is unknown, but it is said to involve the following pathophysiology:
Immune Complex Deposition:
Immune complexes are a combination of antibodies and proteins. They are formed when antibodies mistakenly target the proteins in your tissues. These complexes deposit in the walls of your blood vessels, especially the small and medium ones. This process triggers inflammation that directly damages the vessels.
Autoantibody-Mediated Injury:
Your body produces several harmful autoantibodies in lupus. These greatly increase inflammation and cause injury to your blood vessel walls:
- Anti-dsDNA binds to DNA and forms immune complexes.
- ANCA/ Anti-Neutrophil Cytoplasmic Antibodies activate neutrophils that release damaging enzymes.
- AECA/ Anti-Endothelial Cell Antibodies target the cells lining your blood vessels.
- APL/ Anti-Phospholipid Antibodies increase clotting and contribute to vessel blockage.
Inflammatory Cascade:
After deposition of immune complexes, your immune system sees them as threats. Inflammatory cells like neutrophils and macrophages flock to the affected area. Here, they release enzymes and reactive molecular species. Consequently, there is vessel swelling, thickening, and sometimes even complete blockage.
Endothelial Cell Damage:
Immune complexes and autoantibodies directly attack the endothelium, or blood vessel lining. The vessel wall becomes leaky and fragile, which may trigger clot formation or bleeding.
Impaired Clearance of Dying Cells:
Normally, your body quietly clears out dead or dying cells. In lupus, this cleanup process is faulty. The leftover cellular debris fuels more autoantibody production and keeps the immune system in a constant state of attack, worsening the vasculitis.3Accapezzato, D., Caccavale, R., Paroli, M. P., Gioia, C., Nguyen, B. L., Spadea, L., & Marino Paroli. (2023). Advances in the Pathogenesis and Treatment of Systemic Lupus Erythematosus. International Journal of Molecular Sciences, 24(7), 6578–6578. https://doi.org/10.3390/ijms24076578
Symptoms of Lupus Vasculitis
If you have lupus, developing vasculitis can lead to a mix of general and organ-specific symptoms, such as:
Lupus Vasculitis General Symptoms:
Lupus vasculitis often starts subtly, and its early signs feel like a regular lupus flare.. These symptoms may not seem specific and include:
- Persistent fever
- Low-grade
- Extreme fatigue that is even more widespread than your usual lupus tiredness
- Unexplained weight loss
- Loss of appetite
- Widespread muscle aches and joint pain
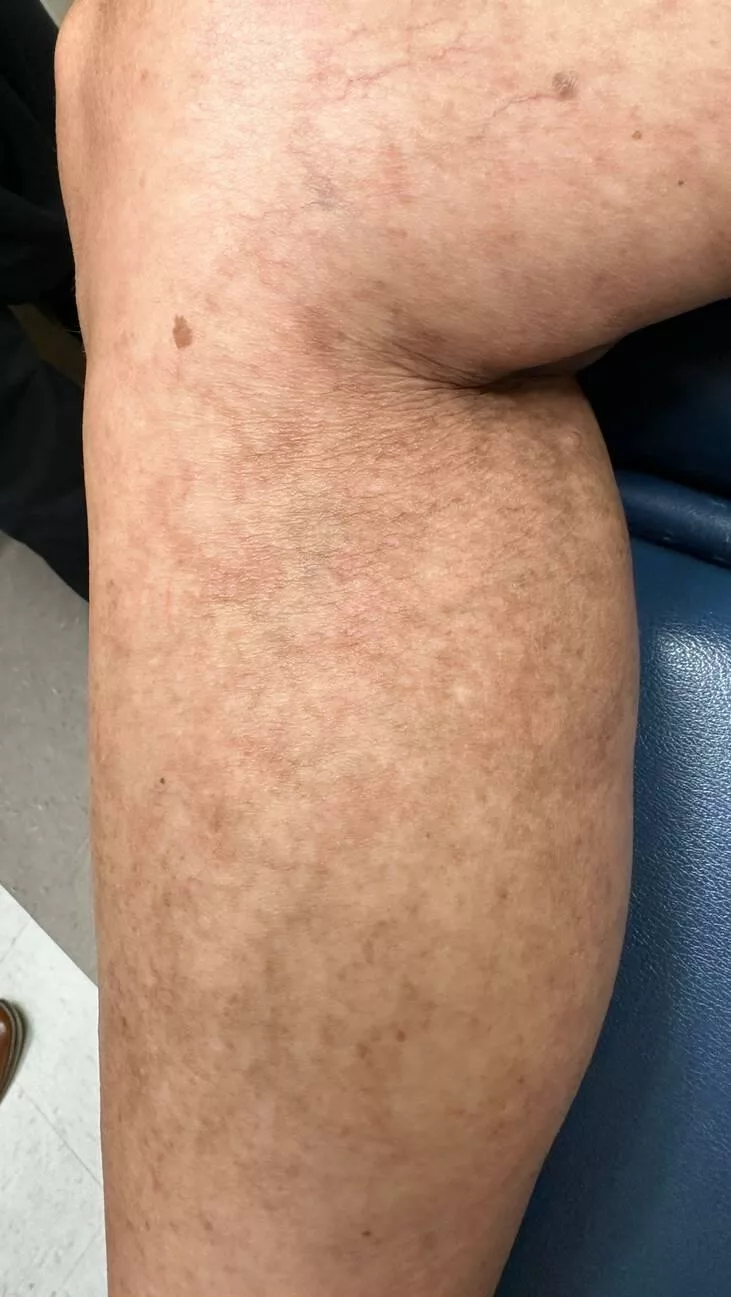
Skin Symptoms of Lupus Vasculitis:
The skin is the most common place where lupus vasculitis shows up, with signs and symptoms such as
- Palpable purpura, which are small red or purple dots that don’t fade when pressed (especially on your legs)
- Itchy, hive-like rashes that could be painful
- Ulcers, especially near your ankles
- Digital infarcts of black spots or dead skin at fingertips or toes in severe cases
- Livedo reticularis, which is a lace-like purple discoloration on the skin, is a sign of reduced blood flow
Joint & Muscle Symptoms of Lupus Vasculitis:
Though lupus already affects your joints, vasculitis can worsen symptoms:
- Increased swelling and stiffness in joints
- Pain that doesn’t improve with usual lupus meds
- Aching in large muscle groups from reduced blood supply
Nervous System Symptoms of Lupus Vasculitis:
When vasculitis involves blood vessels in your brain and nerves, you experience:
- Headaches (especially migraines) that feel different from usual
- Seizures, especially if vasculitis is severe
- Behavioral and mood changes
- Numbness, tingling, or burning in your hands and feet due to peripheral nerve involvement
- Sudden weakness
- Cerebrovascular accident, like stroke or hemorrhage
Gastrointestinal Symptoms of Lupus Vasculitis:
Lupus vasculitis affecting the digestive tract is rare. It can mimic a stomach bug, but is dangerous if left untreated:
- Intense abdominal cramping and pain
- Bloating
- Nausea or vomiting
- Blood in stool from bowel ischemia and ulceration
Pulmonary Symptoms
When your lungs are involved, lupus vasculitis symptoms can be both subtle and intense:
- Dry cough
- A fever that cannot be explained by the possibility of infection
- Shortness of breath, especially during physical activity
- Lung scarring can develop over time in a few cases
Cardiac Symptoms of Lupus Vasculitis:
Lupus vasculitis can affect the coronary arteries that supply your heart, although it’s rare. Symptoms of cardiac involvement in lupus vasculitis include:
- Chest pain or tightness
- Shortness of breath on exertion
- Unexplained palpitations
Kidney Symptoms of Lupus Vasculitis:
Lupus already targets the kidneys with lupus nephritis, but vasculitis in the kidneys can cause silent damage, high blood pressure, or changes in your urine. It may only be detected through a panel of renal function tests.
Eye Symptoms of Lupus Vasculitis:
Though uncommon, vasculitis in the eyes can threaten your vision with temporary or permanent loss if the vessels get damaged. Symptoms include sudden blurry vision, eye redness, and pain.4Leone, P., Prete, M., Malerba, E., Bray, A., Susca, N., Ingravallo, G., & Racanelli, V. (2021). Lupus Vasculitis: An Overview. Biomedicines, 9(11), 1626–1626. https://doi.org/10.3390/biomedicines9111626

How is a Lupus Vasculitis diagnosis established?
The diagnosis of lupus vasculitis involves a thorough medical history, physical examination, as well as rigorous lab tests.
History & Physical Exam:
If your doctor suspects that you have lupus vasculitis, they’ll start by asking you about your symptoms, like joint pain, skin rashes, headaches, or any unusual weakness or numbness. They might also ask if you’ve had any recent infections or have started a new medication.
During the physical exam, your doctor will check your skin for rashes, spots, or sores. They’ll look closely at your hands and feet for signs of poor blood flow. If you’ve mentioned memory issues or confusion, they may also check your nervous system to see if your brain or nerves are being affected.
Lab Tests:
A variety of general and specific lab tests are used to identify lupus vasculitis. A general lab panel for lupus vasculitis includes:
- CBC to find low red cells, white cells, or platelets seen in lupus.
- ESR and CRP to detect general inflammation in the body.
- Kidney and liver function tests to evaluate organ involvement from lupus.
- Urinalysis to catch blood or protein in urine, suggesting kidney damage.
- Blood cultures or viral studies to rule out infections that can mimic vasculitis.
Meanwhile, lab tests which are used to arrive at a diagnosis of lupus vasculitis include:
- ANA to support the diagnosis of lupus.
- Anti-dsDNA will be used to assess lupus activity and confirm the disease.
- C3 and C4 to check for immune system activation and inflammation.
- ANCA will explore other possible overlapping vasculitic conditions.
- aPL to identify abnormal clotting risk linked to lupus.
Tissue Biopsy:
Tissue biopsy is the gold standard for diagnosing lupus vasculitis. A sample of blood vessel tissue is taken, stained with special dyes, and examined by a histopathologist. This confirms the diagnosis by showing inflammation and immune complex deposition in blood vessels.
Imaging:
Different scans help doctors see inside your body without needing surgery. These provide a clearer picture of inflamed blood vessels and organ damage, such as:
- MRI scans find inflammation and damage in organs like your brain or muscles.
- A CT scan can identify vascular changes and organ involvement in lupus vasculitis.
- Ultrasound evaluates blood flow in your affected vessels, especially in larger arteries.
- Angiography is used to visualize narrowed or blocked blood vessels.
- PET scan to detect areas of active inflammation throughout your body5NIAMS. (2017, April 11). Systemic Lupus Erythematosus (Lupus). National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.niams.nih.gov/health-topics/lupus/diagnosis-treatment-and-steps-to-take
What are the treatment options for Lupus Vasculitis?
Lupus vasculitis is treated through a variety of treatments that affect your immune system and immune response, such as:
Corticosteroids:
When your vasculitis flares up, the first thing your doctor will probably give you is a corticosteroid. Corticosteroids prevent the immune system from attacking the body’s own tissues, which is the hallmark of vasculitis.
- Prednisone is the most common corticosteroid used to treat vasculitis. It works by suppressing your immune system to reduce inflammation in the blood vessels. By decreasing your overactive immune response, corticosteroids help prevent further damage to organs like the kidneys, lungs, and skin.
- Initially, you are given a high dose of prednisone to quickly control inflammation during a flare-up. As the disease comes under control, the dose is gradually lowered to minimize side effects.
- Steroids are only used for short time periods as they can cause side effects
- Weight gain
- Mood swings
- Blood sugar problems
- Thinning bones
Immunosuppressants:
Immunosuppressants suppress the overall function of your immune system. These drugs are especially important if your vasculitis is more severe or keeps coming back. Your doctor may choose one of the following:
- Methotrexate inhibits cell growth, particularly in rapidly dividing cells like those of your immune system. This reduces the inflammatory response and helps control the symptoms of vasculitis.6Gansauge, S., Breitbart, A., Rinaldi, N., & Schwarz-Eywill, M. (1997). Methotrexate in patients with moderate systemic lupus erythematosus (exclusion of renal and central nervous system disease). Annals of the Rheumatic Diseases, 56(6), 382-385. https://doi.org/10.1136/ard.56.6.382
- Azathioprine helps by interfering with the production of new DNA. It reduces the activity of the immune cells that are responsible for attacking the blood vessels and lowers the level of inflammation.
- Cyclophosphamide works by blocking the growth of immune cells that produce antibodies and cause inflammation in the blood vessels. It’s used when more aggressive treatment is needed.
- Mycophenolate mofetil targets enzymes involved in the growth of T and B cells, These cells are responsible for immune system dysfunction. Reducing these cells helps to control inflammation.
Biologic Therapy:
Biologic drugs are advanced medications that target very specific parts of your immune system. The most common ones include:
- Rituximab is a monoclonal antibody. It targets and destroys B cells.
- Tocilizumab is another monoclonal antibody that blocks the action of interleukin-6, a molecule involved in the inflammation process.
- Anti-TNF agents like infliximab work by blocking the tumor necrosis factor/TNF, a protein that causes inflammation.
Plasmapheresis:
Plasmapheresis is a procedure used to cleanse your blood. It works by removing harmful antibodies and immune complexes from the blood. This is achieved by circulating the blood through a machine that filters out these blood components. Plasmapheresis is particularly useful in life-threatening cases where lupus vasculitis has severely affected the kidneys, lungs, or other vital organs.

Surgery:
Surgical interventions can be needed when vasculitis causes structural complications like aneurysms or blockages in blood vessels. Angioplasty, a surgical procedure that involves using a balloon that open up narrowed or blocked arteries, is usually used.
Supportive Care
Even though these aren’t the main treatments, supportive care plays a huge role in your recovery from this condition.
- Bone-strengthening medications, e.g., calcium, vitamin D, and bisphosphonates, are often prescribed for long-term corticosteroid users. This can prevent bone loss and fractures, which are common side effects of steroids.
- Preventive antibiotics protect against infections, especially when medications suppress your immune system. Vaccines may also be recommended to reduce the risk of preventable infections like the flu, pneumonia, and shingles.
- Keeping an eye on your blood pressure and blood cholesterol levels is important since both lupus vasculitis and some lupus vasculitis treatments can increase your risk of heart disease and high blood pressure.7Bartels, C. M. (2024, October 29). Systemic Lupus Erythematosus (SLE) Treatment & Management: Approach Considerations, Pivotal and New Lupus Therapies, Emergency Department Management. Medscape.com; Medscape. https://emedicine.medscape.com/article/332244-treatment
Life Expectancy for Lupus Vasculitis
Around 85% of people diagnosed with SLE live at least 10 years, and nearly 75% reach the 20-year mark. If you have lupus vasculitis, your prognosis depends on how early it was caught and how well you have managed it. With proper treatment, your chances can still fall within this range.8García-Carrasco, M., Pinto, C. M., Carlos, J., Morales, I. E., Cervera, R., & Anaya, J.-M. (2013, July 18). Systemic lupus erythematosus. Nih.gov; El Rosario University Press. https://www.ncbi.nlm.nih.gov/books/NBK459474/
Conclusion
Lupus vasculitis is a secondary disorder of SLE. It sparks inflammation and damage to blood vessels present all across your body. Symptoms vary depending on which organ of your body has been affected. Treatment includes drugs that affect your immune system and lifestyle changes.
Refrences
- 1Gamal, S. M., Mohamed, S. S., Tantawy, M., Siam, I., Soliman, A., & Niazy, M. H. (2021). Lupus-related vasculitis in a cohort of systemic lupus erythematosus patients. Archives of Rheumatology, 36(4), 595–692. https://doi.org/10.46497/archrheumatol.2021.8804
- 2Saleh, A., Yee, C.-S., Acquah, A., Gordon, C., & Reynolds, J. A. (2024). Cutaneous vasculitis in systemic lupus erythematosus: epidemiology and risk factors over a 20-year follow-up. Lara D. Veeken. https://doi.org/10.1093/rheumatology/keae672
- 3Accapezzato, D., Caccavale, R., Paroli, M. P., Gioia, C., Nguyen, B. L., Spadea, L., & Marino Paroli. (2023). Advances in the Pathogenesis and Treatment of Systemic Lupus Erythematosus. International Journal of Molecular Sciences, 24(7), 6578–6578. https://doi.org/10.3390/ijms24076578
- 4Leone, P., Prete, M., Malerba, E., Bray, A., Susca, N., Ingravallo, G., & Racanelli, V. (2021). Lupus Vasculitis: An Overview. Biomedicines, 9(11), 1626–1626. https://doi.org/10.3390/biomedicines9111626
- 5NIAMS. (2017, April 11). Systemic Lupus Erythematosus (Lupus). National Institute of Arthritis and Musculoskeletal and Skin Diseases. https://www.niams.nih.gov/health-topics/lupus/diagnosis-treatment-and-steps-to-take
- 6Gansauge, S., Breitbart, A., Rinaldi, N., & Schwarz-Eywill, M. (1997). Methotrexate in patients with moderate systemic lupus erythematosus (exclusion of renal and central nervous system disease). Annals of the Rheumatic Diseases, 56(6), 382-385. https://doi.org/10.1136/ard.56.6.382
- 7Bartels, C. M. (2024, October 29). Systemic Lupus Erythematosus (SLE) Treatment & Management: Approach Considerations, Pivotal and New Lupus Therapies, Emergency Department Management. Medscape.com; Medscape. https://emedicine.medscape.com/article/332244-treatment
- 8García-Carrasco, M., Pinto, C. M., Carlos, J., Morales, I. E., Cervera, R., & Anaya, J.-M. (2013, July 18). Systemic lupus erythematosus. Nih.gov; El Rosario University Press. https://www.ncbi.nlm.nih.gov/books/NBK459474/