Amoebic Dysentery or Amoebiasis is a parasitic infection that causes diarrhea and abdominal cramping. The causative agent for amoebiasis is Entamoeba histolytica, a protozoal parasite that enters the intestines and leads to symptoms such as fever, nausea, cramps, diarrhea, etc. The condition is prevalent in regions with poor sanitation (mostly countries with low socioeconomic status). Every year, about 50 million people worldwide contract amoebiasis, and the disease causes around 100,000 deaths per annum.1Bercu, T. E., Petri, W. A., & Behm, B. W. (2007). Amebic colitis: new insights into pathogenesis and treatment. Current gastroenterology reports, 9, 429-433. Moreover, this disease contributes to more than 2.2 million disability-adjusted life years (DALYs) worldwide. Thus, there is a significant health burden. Therefore, timely and effective treatment is a must.2Nasrallah, J., Akhoundi, M., Haouchine, D., Marteau, A., Mantelet, S., Wind, P., … & Izri, A. (2022). Updates on the worldwide burden of amoebiasis: A case series and literature review. Journal of infection and public health, 15(10), 1134-1141. Healthcare professionals treat the parasitic disease with antibiotics.
Amoebiasis Symptoms
In some cases, the disease is completely asymptomatic. However, symptoms of amoebiasis appear 7-28 days after exposure to the parasite. The intensity of the symptoms varies between individuals. The most common amoebiasis symptoms include:

Abdominal Cramps & Nausea
These are the most common symptoms of amoebiasis.3Pritt, B. S., & Clark, C. G. (2008, October). Amebiasis. In Mayo Clinic Proceedings (Vol. 83, No. 10, pp. 1154-1160). Elsevier. Patients suffering from even the mild form of disease report unexplained cramping of the abdomen. Clinical cases reveal that amoebiasis can be an atypical cause of lower abdominal cramping pain.4De Somer, T., Baert, D., Deceuninck, M., Van Steenkiste, C., Marichal, D., Gabriel, C., … & Dewint, P. (2021). An atypical cause of right lower abdominal pain: amoebiasis, a family cluster. Acta gastro-enterologica belgica.-Bruxelles, 1996-2007, 84(2), 362-364.
Fever
This is one of the initial features of the protozoal infection. Occasional fever is present in the mild form of the disease. However, high-grade fever is seen in advanced stages.
Diarrhea
Loose, watery stools are frequently seen in amoebiasis patients. The stool color doesn’t change, but there is excessive water. Patients have 3-8 semi-formed stools per day that are usually mixed with mucus. However, bloody diarrhea results from more severe complications like colitis.
Tenesmus
The condition of rectal pain during bowel movement is known as tenesmus. Intestinal amoebiasis is linked to intense tenesmus and other symptoms like nausea, severe dysentery, and abdominal pain.5Kantor, M., Abrantes, A., Estevez, A., Schiller, A., Torrent, J., Gascon, J., … & Ochner, C. (2018). Entamoeba histolytica: updates in clinical manifestation, pathogenesis, and vaccine development. Canadian Journal of Gastroenterology and Hepatology, 2018(1), 4601420. Some patients also report anorexia (eating disorder) and unexplained weight loss along with tenesmus.
Complications Associated With Amoebiasis
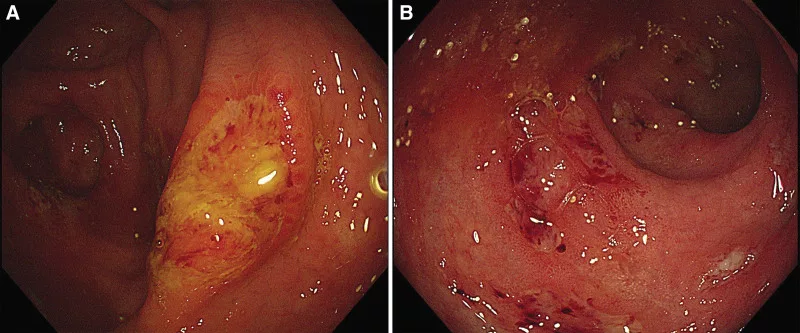
Ameobic Colitis
In some cases, amoebic infection has serious consequences. Several patients experience bloody diarrhea due to inflammation of the intestines, i.e., colitis. Endoscopic and pathological findings reveal that the cecum is the most commonly affected site for colitis that leads to bloody diarrhea.6Yue, B., Meng, Y., Zhou, Y., Zhao, H., Wu, Y., & Zong, Y. (2021). Characteristics of endoscopic and pathological findings of amebic colitis. BMC gastroenterology, 21, 1-6.
Fulminant Colitis
A rare complication of amoebic infestation is fulminant necrotising amoebic colitic (FulNAC). Fulminant amoebic colitis patients present with fever, abdominal cramps (severe pain), and mucous+blood mixed stools.7Beg, M. Y., Bains, L., Mahajan, R., Lal, P., Choudhury, S., Kumar, N. P., … & Pal, V. (2020). Fulminant necrotising amoebic colitis of whole of large bowel: a rare complication of a common infectious disease. Case Reports in Infectious Diseases, 2020(1), 8845263. Though rare, fulminant colitis is a fatal complication and requires immediate diagnosis and treatment.8Kiriwaththuduwa, S., Gnanapragasam, R., Amarasinghe, A., Adikari, Y., Ranasinghe, S., Morel, R., … & Bandara, L. (2020). Acute fulminant necrotizing amebic colitis in a pediatric patient: a rare complication of amebiasis with high mortality—a case report. Annals of Pediatric Surgery, 16, 1-4. Young patients are more prone to developing this.
Amoebic Liver Abscess
Extra-intestinal manifestations of amoebic infection are seen in very few cases. A liver abscess causes pain and tenderness in the upper right quadrant (due to hepatomegaly). Moreover, GIT symptoms include abdominal distention, pain, vomiting, diarrhea, etc.
In rare instances, the parasitic infection can also adversely affect the heart (pericardial effusion), lungs, brain, kidneys, and skin.
What Causes Amoebiasis?
The culprit for this intestinal disease is a protozoa, i.e., Entamoeba histolytica. The microbe enters your body if you ingest it. The most common means of transmission include:
- Drinking fecally-contaminated water (carrying E. histolytica)
- Eating food containing the protozoa
- By eating/washing from hands contaminated with the parasite
Humans serve as natural hosts for Entamoeba histolytica. The parasite exists in mature cyst forms. Once inside the small intestine, there is an excystation of the mature cysts, which leads to the release of trophozoites (active growth stage of a parasite) in the large intestine. The parasite feeds off the host and lays eggs in the host body that later become mature cysts.
Is Amoebiasis Contagious?
Yes, amoebiasis is contagious. An infected person releases cysts in his stool. You can contract the disease if you eat food or drink water contaminated with an infected person’s stool. Even physical contact with an infected person can make you sick if your (or the infected person’s) personal hygiene is poor.
High-Risk Groups
The following individuals are at a greater risk of developing the disease:

- Inhabitants of regions with poor sanitary conditions (parts of Asia, Africa, etc.)
- Travelers who visit places with poor sanitation
- Individuals who engage in anal sex9Hughes, R., Richardson, D., & Fitzpatrick, C. (2024). Factors associated with Entamoeba histolytica proctocolitis in men who have sex with men: a systematic review. Frontline Gastroenterology, 15(4), 321-327.
- People with weak immunity (malnutrition, alcohol consumption, corticosteroid medications use, etc.)
Amoebiasis Diagnosis
History & Physical Examination:
Your healthcare provider will take a complete history of your symptoms. Travel history to areas with poor water sanitation is of critical importance. Additionally, sexual history is also significant.
Then, your doctor will perform a thorough physical examination. He notes any tenderness and pain in the right upper quadrant to check for a liver abscess.
Diagnostic Tests:
Multiple amoebiasis tests are in practice in different countries. The most effective detection methods include10Tanyuksel, M., & Petri Jr, W. A. (2003). Laboratory diagnosis of amebiasis. Clinical microbiology reviews, 16(4), 713-729.
Direct Microscopy
A pathologist places stool samples (or rectal swabs) directly under the microscope to see the micro-organisms. This method helps reach diagnosis in about 30% of cases. However, this method is now obsolete.
Stool Antigen Detection Test
This test detects parasite structure (antigen) in stool samples.
Antibody Test
This blood test detects the presence of antibodies (in the blood) against the parasite.
Liver Aspiration
This involves obtaining fluid from the liver (via aspiration) to check for liver abscesses.
Imaging Tests:
Colonoscopy
Doctors opt for a colonoscopy to obtain mucosal scrapings when the stool studies are negative. Sometimes, healthcare workers perform a sigmoidoscopy to examine the lower part of the large intestine.
Ultrasound & CT scans
These imaging scans are done to check signs of extraintestinal amoebiasis.
Differential Diagnosis
Due to similar symptoms, the following conditions fall under DD of amoebiasis:
- Colitis (by E.coli or Campylobacter infection)
- Diverticulitis
- Cholecystitis
- Hepatitis A
Amoebiasis Treatment
If left untreated, amoebiasis can lead to grave consequences and even death. The disease is known to have a high morbidity and mortality rate. Thus, timely treatment is a must (especially in immunocompromised patients).
Antibiotic therapy is the mainstay of treatment. Amoebiasis medication includes different classes of antibiotics. Doctors mostly advise adult patients to take metronidazole (500mg/6-8 hours) for two weeks or tinidazole (2g/day) for three days. Healthcare professionals may also prescribe luminal agents.
How Can I Prevent/Reduce The Risk Of Amoebiasis?
You should exercise great caution when visiting areas with poor sanitation. By adopting these steps, you can minimize the risk of amoebiasis:
- Wash your hands frequently with clean water and soap
- Avoid drinking from the region’s water supply and drink only from a sealed water bottle. If bottled water is unavailable, make sure you boil your drinking water.
- Practice safe sex (use condoms) to prevent disease transmission.
- Peel off fruits and wash thoroughly before eating.
Final Word
Amoebiasis is a contagious, infectious disease caused by the protozoa Entamoeba histolytica. The parasite affects the intestines, leading to issues like diarrhea, nausea/vomiting, abdominal cramps, and fever. The disease may also have extra-intestinal manifestations. It is common in areas with poor water sanitation, and consumption of fecally contaminated drinking water is a major mode of transmission. It rarely causes serious complications. However, fulminant colitis can be fatal if left untreated. Diagnosis requires travel history, stool tests, blood tests (antigen/antibody), and imaging scans. Treatment involves antibiotic therapy, i.e., metronidazole or tinidazole. You can prevent transmission by frequently washing hands, avoiding tap water, and practicing safe sex.
Refrences
- 1Bercu, T. E., Petri, W. A., & Behm, B. W. (2007). Amebic colitis: new insights into pathogenesis and treatment. Current gastroenterology reports, 9, 429-433.
- 2Nasrallah, J., Akhoundi, M., Haouchine, D., Marteau, A., Mantelet, S., Wind, P., … & Izri, A. (2022). Updates on the worldwide burden of amoebiasis: A case series and literature review. Journal of infection and public health, 15(10), 1134-1141.
- 3Pritt, B. S., & Clark, C. G. (2008, October). Amebiasis. In Mayo Clinic Proceedings (Vol. 83, No. 10, pp. 1154-1160). Elsevier.
- 4De Somer, T., Baert, D., Deceuninck, M., Van Steenkiste, C., Marichal, D., Gabriel, C., … & Dewint, P. (2021). An atypical cause of right lower abdominal pain: amoebiasis, a family cluster. Acta gastro-enterologica belgica.-Bruxelles, 1996-2007, 84(2), 362-364.
- 5Kantor, M., Abrantes, A., Estevez, A., Schiller, A., Torrent, J., Gascon, J., … & Ochner, C. (2018). Entamoeba histolytica: updates in clinical manifestation, pathogenesis, and vaccine development. Canadian Journal of Gastroenterology and Hepatology, 2018(1), 4601420.
- 6Yue, B., Meng, Y., Zhou, Y., Zhao, H., Wu, Y., & Zong, Y. (2021). Characteristics of endoscopic and pathological findings of amebic colitis. BMC gastroenterology, 21, 1-6.
- 7Beg, M. Y., Bains, L., Mahajan, R., Lal, P., Choudhury, S., Kumar, N. P., … & Pal, V. (2020). Fulminant necrotising amoebic colitis of whole of large bowel: a rare complication of a common infectious disease. Case Reports in Infectious Diseases, 2020(1), 8845263.
- 8Kiriwaththuduwa, S., Gnanapragasam, R., Amarasinghe, A., Adikari, Y., Ranasinghe, S., Morel, R., … & Bandara, L. (2020). Acute fulminant necrotizing amebic colitis in a pediatric patient: a rare complication of amebiasis with high mortality—a case report. Annals of Pediatric Surgery, 16, 1-4.
- 9Hughes, R., Richardson, D., & Fitzpatrick, C. (2024). Factors associated with Entamoeba histolytica proctocolitis in men who have sex with men: a systematic review. Frontline Gastroenterology, 15(4), 321-327.
- 10Tanyuksel, M., & Petri Jr, W. A. (2003). Laboratory diagnosis of amebiasis. Clinical microbiology reviews, 16(4), 713-729.