Pericardial effusion is a medical condition in which fluid abnormally accumulates in the pericardial sac, the protective, sac-like structure surrounding the heart. The term “effusion” refers to the leakage of fluid from the circulatory system into surrounding tissues or spaces. The pericardium consists of two layers: the inner visceral layer, which is attached to the heart’s surface, and the outer parietal layer. Together, these layers protect the heart from infection and mechanical injury.
In a healthy individual, the pericardial sac normally contains between 15 and 50 mL of clear fluid. This fluid can vary in type: it may be transudative (due to fluid imbalance), exudative (due to inflammation), or bloody. It may also contain substances like metabolites, biomolecules, or, in some cases, infectious organisms or cancer cells.1Willner DA, Goyal A, Grigorova Y, et al. Pericardial Effusion. [Updated 2024 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431089/ Pericardial effusion can lead to a variety of symptoms and complications, depending on the amount of fluid present and the underlying cause.

What Causes a Pericardial Effusion?
This condition can be caused2Corey, G. R., Campbell, P. T., Van Trigt, P., Kenney, R. T., O’Connor, C. M., Sheikh, K. H., … & Wall, T. C. (1993). Etiology of large pericardial effusions. The American journal of medicine, 95(2), 209-213. by various medical conditions, such as infections, heart failure, cancer, or trauma. Here is the list of a few causes:
Infections
The most common cause of pericardial effusion is an infection caused by a virus or bacteria, such as Human Immunodeficiency Virus (HIV), Cytomegalovirus (CMV), and Staphylococcus aureus. Infection caused by these agents can cause inflammation (swelling of tissues and leaky vessels) and increased fluid production in the pericardial sac.3Vakamudi, S., Ho, N., & Cremer, P. C. (2017). Pericardial effusions: causes, diagnosis, and management. Progress in cardiovascular diseases, 59(4), 380-388.
Myocardial Infarction
A heart attack or myocardial infarction can indirectly lead to pericardial effusion. The inflammation and damage caused by a heart attack can result in pericarditis, an inflammation of the pericardium. This inflammation can trigger fluid accumulation in the pericardial sac, causing pericardial effusion. Additionally, complications such as heart muscle rupture or damage to blood vessels can lead to bleeding into the pericardial sac, further contributing to pericardial effusion.
Autoimmune Disorders
In these disorders, the body’s immune system recognizes self-tissues as foreign. It attacks them, leading to widespread inflammation in the body and the development of pericardial effusion, among other symptoms. Systemic lupus erythematosus (SLE), rheumatoid arthritis (RA), and systemic sclerosis (SS) are examples of a few autoimmune diseases that lead to effusion.
Cancers
Cancers, such as lung and breast cancer, are also known to cause pericardial effusion.
Trauma
Chest surgery or blunt trauma from a direct blow to the front of the chest, for example, may puncture the heart and cause surrounding inflammation that causes the rapid development of effusion.
Kidney or Liver failure
Kidney or liver failure can also contribute to pericardial effusion by disrupting fluid balance and causing fluid retention in the body. In both cases, fluid accumulates in the pericardial sac, potentially compressing the heart and affecting its function. Close monitoring and management of fluid levels are important in these conditions.
Medications
In addition to the mentioned causes, certain medications have also been associated with pericardial effusion. Warfarin, an anticoagulant, and phenytoin, an antiepileptic drug, have been reported as potential contributors to the development of pericardial effusion.4Malouf JF, Alam S, Gharzeddine W, Stefadouros MA. The role of anticoagulation in the development of pericardial effusion and late tamponade after cardiac surgery. Eur Heart J. 1993 Nov;14(11):1451-7. doi: 10.1093/eurheartj/14.11.1451. Erratum in: Eur Heart J 1994 Apr;15(4):583-4. PMID: 8299624. These medications may disrupt normal fluid balance or directly affect the pericardium, leading to fluid accumulation in the pericardial sac.5Hori K, Kato Y, Suzuki S, Hirota N, Arita T, Yagi N, Kishi M, Kano H, Matsuno S, Otsuka T, Hori T, Matsuhama M, Iida M, Yajima J, Yamashita T, Uejima T, Oikawa Y. Descriptions of Etiology, Clinical Course, and Prognosis of Patients Presenting with Pericardial Effusion. Int Heart J. 2024 May 31;65(3):452-457.
Idiopathic
The precise cause is often undetermined, which is medically known as “idiopathic.”
What are the Symptoms of Pericardial Effusion?
The severity of symptoms depends upon the speed with which the effusion develops. If effusion develops slowly, you may have little symptoms with even large volumes of fluid in the sac, while the rapid collection of fluid in the cavity leads to more severe and rapid symptoms onset. The accumulation of fluid exerts pressure on the surrounding tissues of the heart, obstructs blood flow, and can cause a wide range of symptoms.
Common symptoms include:
- Chest pain or discomfort, especially when lying down
- Shortness of breath or difficulty breathing
- Palpitations or heart palpitations
- Anxiousness
- Cough
- A general feeling of being unwell
- Swelling of the abdomen
- Fatigue
- Fever
What Tests might your Doctor do to Confirm Pericardial Effusion?
Pericardial effusion can be diagnosed6Sagristà-Sauleda, J., Mercé, A. S., & Soler-Soler, J. (2011). Diagnosis and management of pericardial effusion. World journal of cardiology, 3(5), 135. through various methods. The initial step is taking a detailed history followed by a physical examination by your healthcare provider. Diagnostic tests may confirm the diagnosis and determine the effusion’s underlying cause.
History
It is often the first and crucial step, during which your doctor might ask you questions about the symptoms and try to differentiate the other look-alike disease from it.
Physical Examination
In addition, the second step almost always includes palpating the chest wall for tenderness, discomfort, or a pericardial friction rub (a finding observed on listening to a heartbeat with a stethoscope). If the effusion develops acutely, your BP may drop along with engorged neck veins. Upon auscultation, your heart sounds may also be muffled due to the presence of fluid around it.
Electrocardiogram (ECG/EKG)
An EKG can show changes consistent with pericardial effusion, which includes “pulsus alternans,” in which the heart’s electrical potential fluctuates due to the heart’s movement in the fluid-filled pericardium.
Echocardiography
It is a noninvasive test that can evaluate the amount, position, and velocity of blood flow in the pericardium. It can also detect changes associated with cardiac tamponade (a life-threatening condition with rapid fluid accumulation leading to decreased BP), the main complication of pericardial effusion.
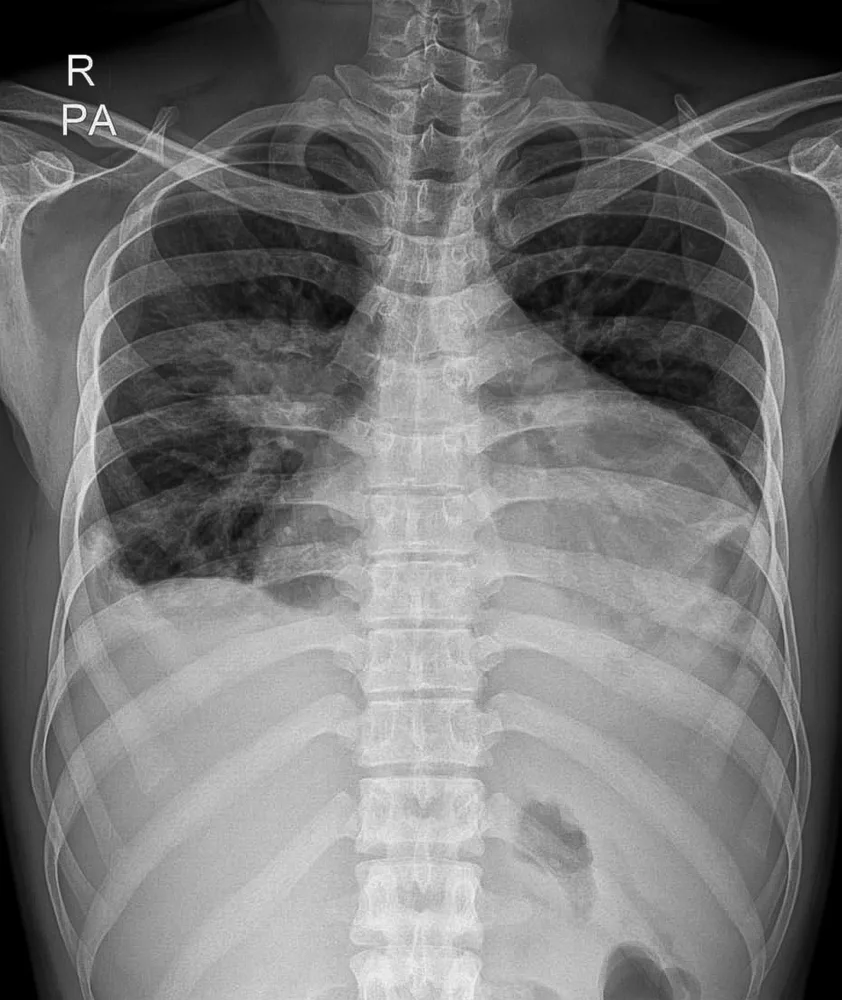
Chest X-rays
These can delineate fluid collections outside the heart and surrounding structures. Most X-rays show an enlarged cardiac silhouette (shadow).
CT Scans
A more advanced imaging modality that can provide a three-dimensional view of the pericardial space.
Pericardiocentesis
It is a diagnostic and therapeutic procedure in which the Doctor inserts a needle through the chest wall into the pericardial space. This procedure can be used to withdraw fluid for diagnostic analysis, as well as to relieve pressure and reduce the size of the effusion (therapeutic).
How do we Treat Pericardial Effusion?
The management7Imazio, M., & Adler, Y. (2013). Management of pericardial effusion. European Heart Journal, 34(16), 1186-1197. of pericardial effusion consists of treating the underlying cause, treating the actual effusion itself by removing excess fluid, and relieving the symptoms of pericardial effusion.
Treating the underlying cause can involve antibiotics for infectious causes, immunosuppressant drugs for autoimmune causes, and treatments for trauma, tumors, and radiation.8Soler-Soler, J., Sagristà-Sauleda, J., & Permanyer-Miralda, G. (2001). Management of pericardial effusion. Heart, 86(2), 235-240.
Medical Treatment of Pericardial Effusion
It aims at treating pericardial effusion typically by reducing inflammation and improving heart function. These medications may include:
- Aspirin
- NSAIDs (nonsteroidal anti-inflammatory drugs)
- Corticosteroids
Surgical Treatments Of Pericardial Effusion
This treatment modality is reserved for very large effusions, cardiac tamponade, or effusions not responding to medical treatment. These include the following drainage procedures:
Pericardiocentesis:
A procedure in which a needle is inserted into the chest area to remove the excess fluid in the pericardial sac.
Pericardiectomy:
A part or whole of the pericardium may also be removed to drain the recurrent effusions and to explore the underlying cause.
What Happens if a Pericardial Effusion is Left Untreated?
Various complications can arise if you leave effusions untreated. Complications can include:
- Cardiac Tamponade (an abnormal buildup of pressure in the pericardial space accompanied by decreased BP and engorged neck veins)
- Recurrent Effusions requiring further medical intervention.
- Constrictive Pericarditis (repeated inflammation leading to contraction and narrowing of pericardial sac)
- Pleural Effusions (collection of excessive amounts of fluid in a sac around the lungs)
- Pulmonary Edema (collection of fluid in lung tissues)
- Arrhythmias (abnormal heart electrical activity; may as well be fatal)
- Heart Failure (due to the inability to pump blood because the heart cannot relax enough to allow sufficient filling due to external pressure caused by fluid buildup)
- Sudden Death
How to Prevent this Condition?
Pericardial effusion is not always preventable, as it can occur due to trauma or difficult-to-prevent infections. However, reducing the risk factors for developing pericardial effusion can help to reduce the likelihood of developing it. These risk factors can include:
- Avoiding exposure to infections such as HIV, tuberculosis, or fungal infections.
- Avoiding physical and emotional stressors.
- Avoid over-the-counter or prescription medications known to have cardiac side effects.
- Controlling underlying conditions, such as hypertension, diabetes, or heart failure.
- Avoiding excessive alcohol consumption or tobacco use.
- Getting regular checkups with a doctor to diagnose and treat any underlying medical conditions.
What is the Outlook for Pericardial Effusion?
The prognosis for pericardial effusion varies based on the underlying etiology. Most cases are mild and can be resolved with medical treatment. Little collections also resolve spontaneously or with the treatment of the underlying etiology. However, serious cases, or those with very large collections, may require surgery to remove fluid or repair the pericardium. Overall, the prognosis is generally good with appropriate treatment.
Conclusion
Pericardial effusions are fluid collections in the pericardial sac that may be deadly if not recognized and treated promptly. Multiple etiologies are reported, and a thorough workup helps in diagnosis. Nonetheless, if the aforementioned symptoms are experienced for longer durations, you should rush to your Doctor to rule out a (possibly) deadly disease.
Refrences
- 1Willner DA, Goyal A, Grigorova Y, et al. Pericardial Effusion. [Updated 2024 Jul 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK431089/
- 2Corey, G. R., Campbell, P. T., Van Trigt, P., Kenney, R. T., O’Connor, C. M., Sheikh, K. H., … & Wall, T. C. (1993). Etiology of large pericardial effusions. The American journal of medicine, 95(2), 209-213.
- 3Vakamudi, S., Ho, N., & Cremer, P. C. (2017). Pericardial effusions: causes, diagnosis, and management. Progress in cardiovascular diseases, 59(4), 380-388.
- 4Malouf JF, Alam S, Gharzeddine W, Stefadouros MA. The role of anticoagulation in the development of pericardial effusion and late tamponade after cardiac surgery. Eur Heart J. 1993 Nov;14(11):1451-7. doi: 10.1093/eurheartj/14.11.1451. Erratum in: Eur Heart J 1994 Apr;15(4):583-4. PMID: 8299624.
- 5Hori K, Kato Y, Suzuki S, Hirota N, Arita T, Yagi N, Kishi M, Kano H, Matsuno S, Otsuka T, Hori T, Matsuhama M, Iida M, Yajima J, Yamashita T, Uejima T, Oikawa Y. Descriptions of Etiology, Clinical Course, and Prognosis of Patients Presenting with Pericardial Effusion. Int Heart J. 2024 May 31;65(3):452-457.
- 6Sagristà-Sauleda, J., Mercé, A. S., & Soler-Soler, J. (2011). Diagnosis and management of pericardial effusion. World journal of cardiology, 3(5), 135.
- 7Imazio, M., & Adler, Y. (2013). Management of pericardial effusion. European Heart Journal, 34(16), 1186-1197.
- 8Soler-Soler, J., Sagristà-Sauleda, J., & Permanyer-Miralda, G. (2001). Management of pericardial effusion. Heart, 86(2), 235-240.