Actinomycosis is a rare, granulomatous infection of the skin characterized by the formation of multiple pus-filled abscesses (or bumps) in different body regions. The abscesses can become large and induce localized swelling. They also often form sinus tracts that drain yellowish pus, known as sulfur granules (typical of actinomyces infection). The pus is composed of clumps of dead bacteria and combating immune cells (neutrophils), which impart the yellow color.
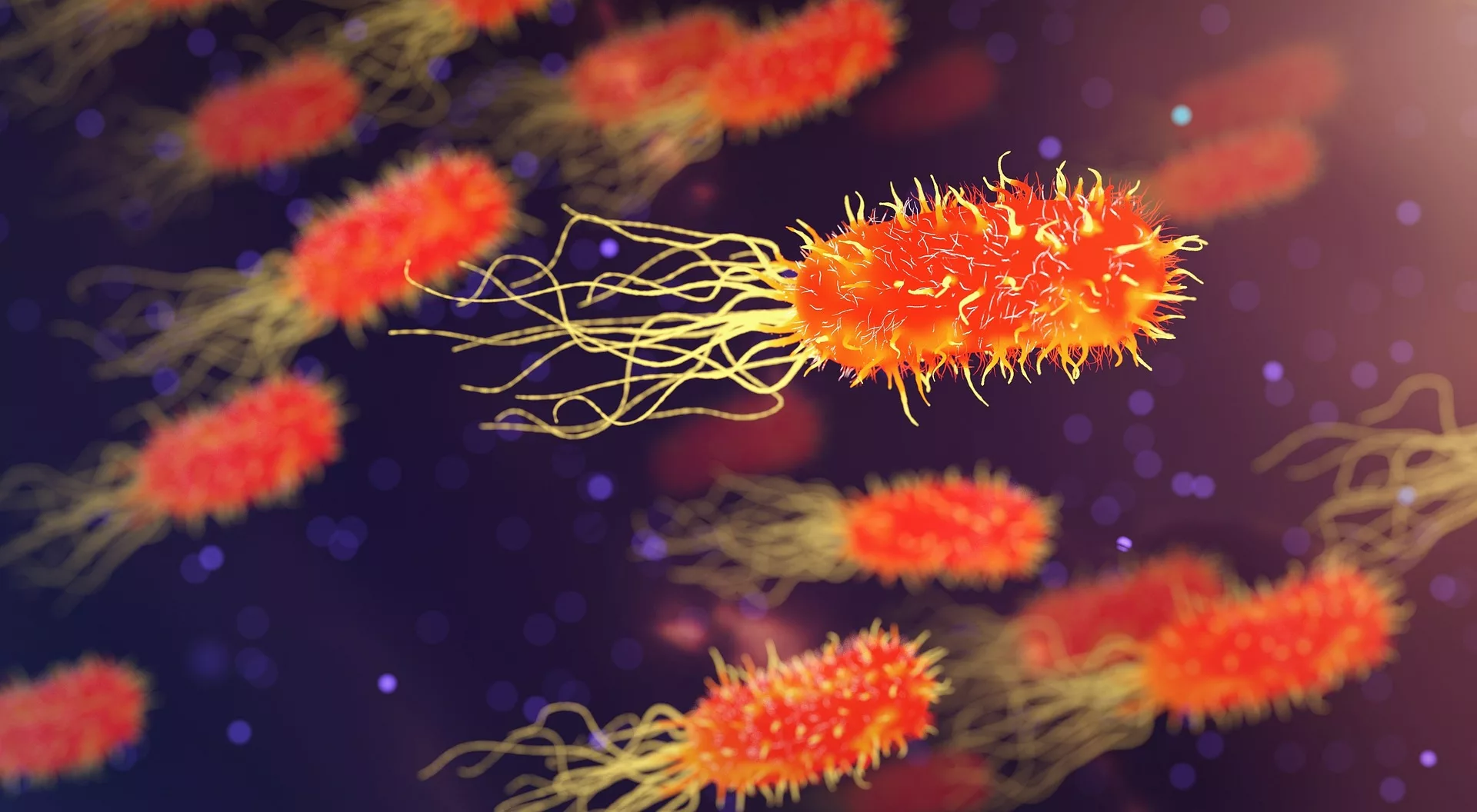
The disease is caused by infection of Actinomyces bacteria. Numerous members of the filamentous actinomycosis family have been identified, but Actinomycosis israelii, A. meyerii, and A. odontolyticus are notorious for causing disease in humans. Classification of the disease is done based on the region involved. The most common site of infection is the orofacial region, i.e., oral-cervicofacial actinomycosis. However, the bacteria may infest other regions like the lungs (thoracic/pulmonary actinomycosis), genitals (pelvic actinomycosis), and abdomen (abdominal actinomycosis), etc. Dental and abdominal surgeries and intra-uterine devices (IUDs) can trigger an infection in prone patients. Treatment requires heavy doses of antibiotics for long periods.
Types Of Actinomycosis
An abscess is a pocket or collection of pus which can be painful. A sinus tract is a passageway or a tunnel that opens into the skin and discharges pus. Based on the region involved, actinomycosis is divided into different types:
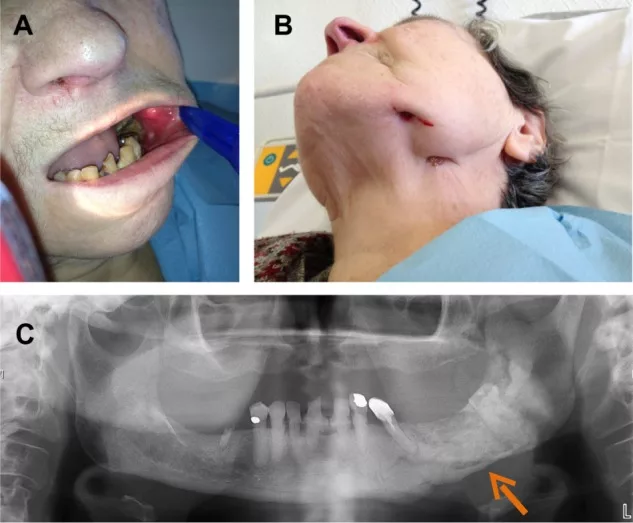
Oral-Cervicofacialal Actinomycosis
The most common types of actinomycosis are oral and cervicofacial. According to estimates, 50-70% of all actinomycosis infections are cervicofacial. It develops in the mouth, nose, face, and jaw region. Therefore, it is also referred to as lumpy jaw syndrome. Cervicofacial actinomycosis gradually spreads to neighboring tissues and lays the foundation for pleural and vocal cord infection. In this type, you will find an abundance of abscesses, fistulous tracts, and draining sinuses. The invasive bacteria eventually lead to tissue fibrosis. Maxillofacial trauma or a recent dental extraction/oral surgery is the most common trigger for a lumpy jaw.1Vandeplas, C., Politis, C., Van Eldere, J., & Hauben, E. (2021). Cervicofacial actinomycosis following third molar removal: case-series and review. Oral and Maxillofacial Surgery, 25, 119-125.
Thoracic/Pulmonary Actinomycosis
Another type is the thoracic or pulmonary actinomycosis. The disease was rare in the pre-antibiotic era but became very rare after the advent of efficient antibiotics. Reports suggest that it affects only 1 in every 3,000,000 people annually. In rare instances, it can cause serious complications like emphysema, pericardial effusion, sepsis, etc.2Boot, M., Archer, J., & Ali, I. (2023). The diagnosis and management of pulmonary actinomycosis. Journal of Infection and Public Health, 16(4), 490-500. As the name indicates, it affects the lungs and the chest region.
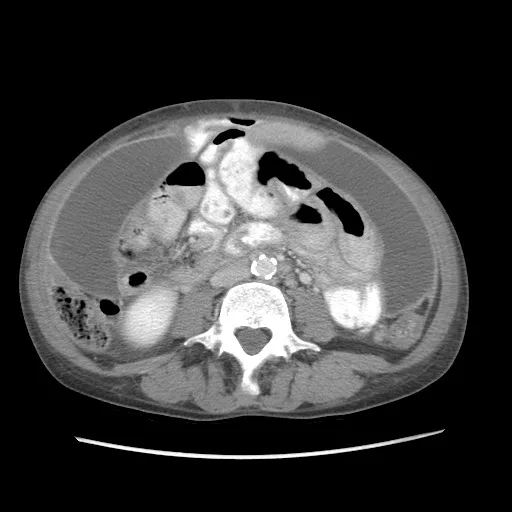
Abdominal Actinomycosis
As the name suggests, this type affects the abdominal organs and the intestines. It is not a common infirmity; therefore, diagnosis may take time and effort. The generalized symptoms of fever, weight loss, and abdominal pain in abdominal actinomycosis patients coincide with other serious complications like colon cancer.3Târcoveanu, E., Vasilescu, A., Andronic, D., Lupaşcu, C., Ciobanu, D., Vlad, N., & Bradea, C. (2019). Abdominal actinomycosis mimicking colon cancer. Chirurgia (Bucur), 114(2), 251-8. It generally affects the ileum (terminal end), cecum and the appendix. Actinomyces israelii is the main culprit.
Uterine/Pelvic Actinomycosis
The second most common form of actinomycosis infection is the genitourinary tract actinomycosis. Many women develop the infection after the placement of an intrauterine device (IUD). Uterine/pelvic actinomycosis can spread far and lead to extensive pelvic involvement. The abscesses may convert into a large infiltrating mass that looks like a tumor radiographically.4Agrawal, A., & Huang, K. G. (2020). A Uterine Actinomycosis with Extensive Pelvic Involvement. Journal of Gynecologic Surgery, 36(4), 214-216. The symptoms and extent of organ involvement (proliferation) can mimic uterine cancer.5Shin, D., Hwang, J., Hong, S. S., Lee, E. J., & Kim, Y. H. (2019). Pelvic actinomycosis mimicking malignancy of the uterus: a case report. Investigative Magnetic Resonance Imaging, 23(2), 136-141.
Actinomycosis Symptoms
The disease can develop on both sides of the body i.e., bilateral actinomycosis. The following symptoms are most commonly seen in actinomycosis infections:
Fluid-Filled Bumps
In oral-cervicofacial actinomycosis, raised bumps/pus-filled areas develop in the mouth, face, jaw, and neck regions. The bumps are frequently present, along with chronic tissue swelling. Generally, the swellings are firm and may mimic malignancy. You may also notice woody fibrosis of the facial lesions.
Yellow Discharge
The abscesses on the face and mouth ooze out granules, which are called sulfur granules based on their yellow color. The yellow granules form when actinomyces bacteria invade healthy tissues. However, the name sulfur granules is only because of the color; there is no sulfur in the pus. The infection may also involve sinuses.
Pain
The region of pain differs with the type of actinomycosis.
Jaw Pain & Tightness
Oral-cervicofacial actinomycosis causes significant pain, swelling, and jaw stiffness. Many patients report mandibular swelling and pain when chewing. The intense pain often interferes with swallowing. Most patients with oral-cervicofacial type have poor oral hygiene, promoting bacteria growth. Prior dental treatment or direct trauma can lead to actinomyces infection and subsequent pain/swelling.6Stájer, A., Ibrahim, B., Gajdács, M., Urbán, E., & Baráth, Z. (2020). Diagnosis and management of cervicofacial actinomycosis: lessons from two distinct clinical cases. Antibiotics, 9(4), 139 However, in a few cases, doctors have noted a pain-free swelling that causes osteomyelitis of the jaw.7Valour, F., Chidiac, C., & Ferry, T. (2015). A 22-year-old woman with right lumpy jaw syndrome and fistula. Case Reports, 2015, bcr2014206557.

Chest Pain
Though rare, the disease can seriously compromise general health. Patients present with severe chest pain that hinders breathing. A study reported chest pain to be the major symptom of pulmonary actinomyces infection, followed by blood vomit (hemoptysis), dyspnea, excessive sputum production, and cough.8Kim, S. R., Jung, L. Y., Oh, I. J., Kim, Y. C., Shin, K. C., Lee, M. K., … & Lee, Y. C. (2013). Pulmonary actinomycosis during the first decade of 21st century: cases of 94 patients. BMC Infectious Diseases, 13, 1-8.
Abdominal Pain
The most common presenting feature of abdominal actinomyces is abdominal pain. As abdominal pain is common to various pathologies, diagnosing actinomycosis is an arduous task. Stomach ache usually coexists with other symptoms such as weight loss, anemia, and anorexia.9Alawainati, M., Al-Khawaja, S., Shawqi, Z., & Alshaikh, S. (2020). Disseminated actinomycosis a rare cause of abdominal pain: a case report. Oman Medical Journal, 35(2), e117.
Anorexia & Weightloss
Accurately known as anorexia nervosa, anorexia is an eating disorder in which patients restrict food intake. Unintended weight loss and anorexia are common in most gastric and liver disorders. Healthcare providers do not get to see many patients with hepatic actinomycosis. However, studies show that hepatic actinomycosis (HA) can present with symptoms like fever, weight loss, anorexia, and abdominal pain.10Chegini, Z., Didehdar, M., Tabaeian, S. P., Khoshbayan, A., & Shariati, A. (2021). A systematic review of case reports of hepatic actinomycosis. Orphanet Journal of Rare Diseases, 16, 1-13.
Fever
A low-grade fever is seen in actinomycosis patients. It is a nonspecific symptom of the disorder. Most patients present to the healthcare setups with mild fever and weight loss complaints.
Vaginal Discharge & Bleeding
Pelvic infection promotes vaginal discharge and even bleeding. Abnormal vaginal discharge is one of the most frequently present symptoms of pelvic actinomycosis, the other two being weight loss and abdominal pain.11Han, Y., Cao, Y., Zhang, Y., Niu, L., Wang, S., & Sang, C. (2020). A case report of pelvic actinomycosis and a literature review. The American Journal of Case Reports, 21, e922601-1. The infection’s sinus tracts can lead to solid masses forming with unclear boundaries. Rarely, this effect can cause a frozen pelvis (tethering together of various structures in the pelvis including the rectum, bladder, and uterus).12Neblett II, M. F., Youssef, Y., & Khan, Z. (2023). A step-by-step approach to a frozen pelvis. Fertility and Sterility, 119(1), 153-154.
Actinomycosis Causes
The bacteria belonging to the genus Actinomycosis are commensal organisms which means that this group of microbes resides within the human body without causing any harm. They are part of the normal flora of the mucosal linings of the mouth/throat, gut and vagina. However, a break in the skin/mucosa can cause entry of the bacteria into the body and cause disease.
More than 30 Actinomyces species have been identified, but Actinomyces israelii is the most common type of bacteria infecting humans. However, another type, i.e., Actinomycosis odontolyticus, is responsible for oral-cervicofacial infection following dental surgery. Other types of bacteria in the group are:
- A. meyeri
- A. naeslundii
- A. viscosus
- A. gerencseriae
How do you get infected when the Bacteria is part of the body?
Infection ensues when the bacteria reach body parts where they don’t belong. Multiple activities can cause a breach in the mucous membranes (of the mouth, vagina, and gut). This allows the bacteria to infect other body parts and replicate. The following procedures are the most frequent causes of bacterial transfer:
Dental Extraction
Extraction of a carious tooth in poor oral hygiene patients can promote actinomycosis infection.13Valour, F., Sénéchal, A., Dupieux, C., Karsenty, J., Lustig, S., Breton, P., … & Ferry, T. (2014). Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infection and drug resistance, 183-197.
Abdominal Surgery
Very rarely, abdominal interventional procedures like cholecystectomy (gall bladder removal) can lay the foundation for abdominal actinomycosis.14Vanoeteren, X., Devreese, K., & De Munter, P. (2014). Abdominal actinomycosis: a rare complication after cholecystectomy. Acta Clinica Belgica, 69(2), 152-156.
Intrauterine Device
Research shows that prolonged use of intrauterine devices can trigger the development of pelvic and abdominal actinomycosis.15Saad, A. A., Ragab, Y., Ahmed, E. S., Emad, Y., Alghamdi, F. A., Taha, I., … & Saad, A. A. (2022). Pelvi-abdominal ACTINOMYCOSIS as a complication of long-term use of intrauterine device (IUD). The important role of imaging in diagnosis and follow-up. Radiology Case Reports, 17(11), 4286-4290.
Aspiration
When a food bolus/liquid gets into your lungs (via the trachea) instead of the esophagus, the condition is called aspiration. It allows oral bacteria (actinomyces) and foreign bodies to reach the lungs and cause pulmonary actinomycosis.16Sobajima, T., Asano, F., Tsuzuku, A., Murakami, A., Masuda, A., Matsuno, Y., & Matsumoto, S. (2015). A case of pulmonary actinomycosis associated with aspiration of cedar leaves. Journal of Bronchology & Interventional Pulmonology, 22(3), 259-262.
Abdominal Pathologies
Diseases like appendicitis and peptic ulcers may also increase the risk of this granulomatous disease.
Risk Groups
The infectivity of actinomyces is pretty low. Therefore, in most cases, infection develops only in specific groups. Per experts, the following is a list of the risk factors:
- Diabetes
- Alcoholism
- Weak immune system (AIDS, etc.)
- Malnutrition
- Immunosuppressants
- Malignancies
- Smoking
Is Actinomycosis Contagious?
No, the disease is not transmissible from an infected to a healthy person. There are no reported cases of human-to-human transmission of actinomycosis. However, an infected person can transfer the bacterial colonies from one body part to another, causing infection of more than one type. Oral-cervicofacial patients frequently suffer from thoracic actinomycosis.
Actinomycosis Diagnosis
Actinomycosis infection is called the “great masquerade.” This is because these bacteria show symptoms similar to a fungal infection and, thus, disguise or masquerade as fungal infections. This quality of the infection makes diagnosis difficult.17Sullivan, D. C., & Chapman, S. W. (2010). Bacteria that masquerade as fungi: actinomycosis/nocardia. Proceedings of the American Thoracic Society, 7(3), 216-221.
Healthcare professionals take a sample of the fluid/tissue from the affected region for diagnostic purposes. This sample may be a collection of sputum, pus, or biopsy specimens, depending on the region involved. The samples are sent to a pathologist for microscopic analysis of the contents. Under the microscope, you will find scores of filamentous gram-positive bacteria and necrosis of sulfur granules (yellowish).
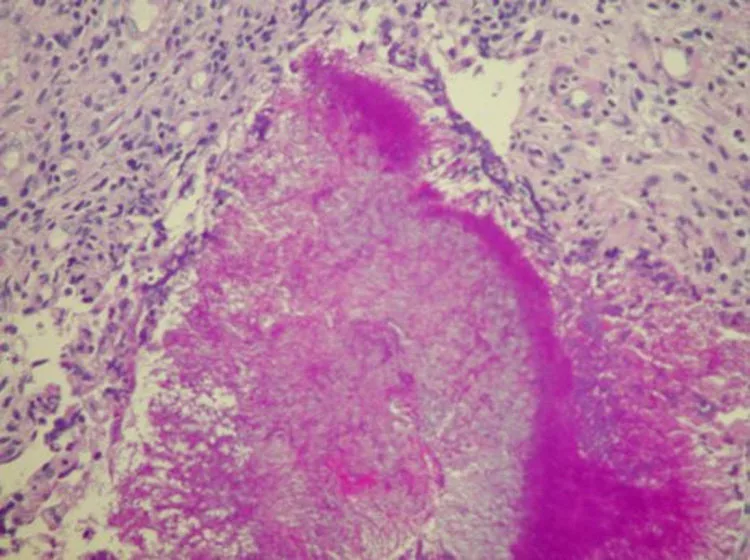
The lesion is surrounded by an outer layer of granulation tissues with collagen fibers and fibroblasts. It is a purulent (discharging pus) lesion that generally contains the following cells:
- Neutrophils
- Lymphocytes
- Plasma cells
Bacterial culture helps reveal strains of infection-causing bacteria such as Actinomycosis israelii. Therefore, it is a crucial diagnostic test for actinomycosis.
Your doctor may also advise an MRI or a CT scan to differentiate the granulomatous mass of actinomycosis from malignancy.
Actinomycosis Treatment
The mainstay of the treatment is antibiotic therapy. Different classes of antibiotic drugs are effective in completely resolving infection. Initially, heavy doses of antibiotics are delivered intravenously (IV) for a few days to weeks (depending on the severity of the disease). However, you may also need antibiotic pills after the acute phase management is over.
The first choice of most doctors is amoxicillin or penicillin G.18Smith, A. J., Hall, V., Thakker, B., & Gemmell, C. G. (2005). Antimicrobial susceptibility testing of Actinomyces species with 12 antimicrobial agents. Journal of Antimicrobial Chemotherapy, 56(2), 407-409. Third-generation cephalosporins are rarely used because actinomyces (some species) can develop resistance against ceftriaxone. Similarly, doctors prescribe broad-spectrum antibiotics (meropenem, tazobactam, etc.) with caution to prevent resistant flora. Macrolides and clindamycin are effective in halting bacterial growth and providing relief.
Frequently, doctors drain the abscesses and remove dead tissues from the infected site (especially in oral actinomycosis). Incision and drainage are followed by debridement of the wound.
Complications Associated With Actinomycosis
If left untreated, the infection can lay the foundation for serious complications. A 55-year-old woman developed a brain abscess following a dental extraction. Actinomyces meyeri was the culprit behind the cerebral abscess.19Clancy, U., Ronayne, A., Prentice, M. B., & Jackson, A. (2015). Actinomyces meyeri brain abscess following dental extraction. Case Reports, 2015, bcr2014207548. Similarly, it can also lead to infection of the jaws, i.e., osteomyelitis.20Sezer, B., Akdeniz, B. G., Günbay, S., Hilmioğlu-Polat, S., & Başdemir, G. (2017). Actinomycosis osteomyelitis of the jaws: report of four cases and a review of the literature. Journal of Dental Sciences, 12(3), 301-307. Additionally, you may also fall prey to tissue necrosis and organ failure. Therefore, timely diagnosis and treatment is a must.
Final Word
Actinomycosis is a rare, granulomatous bacterial infection that affects individuals with weak immunity (diabetes, immunosuppressants, alcoholics, etc.). Actinomyces bacteria are a part of the normal mucosal flora (of the mouth and vagina), but a breach in the lining leads to the transfer of bacteria to unwanted destinations. Actinomyces israelii is the main causative agent that causes actinomycosis in different regions, such as the cervicofacial, abdominal, pelvic, and thoracic.
Patients experience painful abscesses and sinus tracts that drain out yellow sulfur granules. Surgeries (abdominal, dental), trauma, and intrauterine devices can trigger actinomycosis. Antibiotics like penicillin G and amoxicillin effectively treat the disease. However, untreated actinomycosis can lead to serious consequences such as brain abscess and organ failure.
Refrences
- 1Vandeplas, C., Politis, C., Van Eldere, J., & Hauben, E. (2021). Cervicofacial actinomycosis following third molar removal: case-series and review. Oral and Maxillofacial Surgery, 25, 119-125.
- 2Boot, M., Archer, J., & Ali, I. (2023). The diagnosis and management of pulmonary actinomycosis. Journal of Infection and Public Health, 16(4), 490-500.
- 3Târcoveanu, E., Vasilescu, A., Andronic, D., Lupaşcu, C., Ciobanu, D., Vlad, N., & Bradea, C. (2019). Abdominal actinomycosis mimicking colon cancer. Chirurgia (Bucur), 114(2), 251-8.
- 4Agrawal, A., & Huang, K. G. (2020). A Uterine Actinomycosis with Extensive Pelvic Involvement. Journal of Gynecologic Surgery, 36(4), 214-216.
- 5Shin, D., Hwang, J., Hong, S. S., Lee, E. J., & Kim, Y. H. (2019). Pelvic actinomycosis mimicking malignancy of the uterus: a case report. Investigative Magnetic Resonance Imaging, 23(2), 136-141.
- 6Stájer, A., Ibrahim, B., Gajdács, M., Urbán, E., & Baráth, Z. (2020). Diagnosis and management of cervicofacial actinomycosis: lessons from two distinct clinical cases. Antibiotics, 9(4), 139
- 7Valour, F., Chidiac, C., & Ferry, T. (2015). A 22-year-old woman with right lumpy jaw syndrome and fistula. Case Reports, 2015, bcr2014206557.
- 8Kim, S. R., Jung, L. Y., Oh, I. J., Kim, Y. C., Shin, K. C., Lee, M. K., … & Lee, Y. C. (2013). Pulmonary actinomycosis during the first decade of 21st century: cases of 94 patients. BMC Infectious Diseases, 13, 1-8.
- 9Alawainati, M., Al-Khawaja, S., Shawqi, Z., & Alshaikh, S. (2020). Disseminated actinomycosis a rare cause of abdominal pain: a case report. Oman Medical Journal, 35(2), e117.
- 10Chegini, Z., Didehdar, M., Tabaeian, S. P., Khoshbayan, A., & Shariati, A. (2021). A systematic review of case reports of hepatic actinomycosis. Orphanet Journal of Rare Diseases, 16, 1-13.
- 11Han, Y., Cao, Y., Zhang, Y., Niu, L., Wang, S., & Sang, C. (2020). A case report of pelvic actinomycosis and a literature review. The American Journal of Case Reports, 21, e922601-1.
- 12Neblett II, M. F., Youssef, Y., & Khan, Z. (2023). A step-by-step approach to a frozen pelvis. Fertility and Sterility, 119(1), 153-154.
- 13Valour, F., Sénéchal, A., Dupieux, C., Karsenty, J., Lustig, S., Breton, P., … & Ferry, T. (2014). Actinomycosis: etiology, clinical features, diagnosis, treatment, and management. Infection and drug resistance, 183-197.
- 14Vanoeteren, X., Devreese, K., & De Munter, P. (2014). Abdominal actinomycosis: a rare complication after cholecystectomy. Acta Clinica Belgica, 69(2), 152-156.
- 15Saad, A. A., Ragab, Y., Ahmed, E. S., Emad, Y., Alghamdi, F. A., Taha, I., … & Saad, A. A. (2022). Pelvi-abdominal ACTINOMYCOSIS as a complication of long-term use of intrauterine device (IUD). The important role of imaging in diagnosis and follow-up. Radiology Case Reports, 17(11), 4286-4290.
- 16Sobajima, T., Asano, F., Tsuzuku, A., Murakami, A., Masuda, A., Matsuno, Y., & Matsumoto, S. (2015). A case of pulmonary actinomycosis associated with aspiration of cedar leaves. Journal of Bronchology & Interventional Pulmonology, 22(3), 259-262.
- 17Sullivan, D. C., & Chapman, S. W. (2010). Bacteria that masquerade as fungi: actinomycosis/nocardia. Proceedings of the American Thoracic Society, 7(3), 216-221.
- 18Smith, A. J., Hall, V., Thakker, B., & Gemmell, C. G. (2005). Antimicrobial susceptibility testing of Actinomyces species with 12 antimicrobial agents. Journal of Antimicrobial Chemotherapy, 56(2), 407-409.
- 19Clancy, U., Ronayne, A., Prentice, M. B., & Jackson, A. (2015). Actinomyces meyeri brain abscess following dental extraction. Case Reports, 2015, bcr2014207548.
- 20Sezer, B., Akdeniz, B. G., Günbay, S., Hilmioğlu-Polat, S., & Başdemir, G. (2017). Actinomycosis osteomyelitis of the jaws: report of four cases and a review of the literature. Journal of Dental Sciences, 12(3), 301-307.