Venous insufficiency occurs due to impaired venous return from the lower extremities. It can be caused by valvular dysfunction, obstruction, or both. The condition often begins silently, but over time, chronically elevated venous pressure can lead to advanced venous disease, causing tissue damage and significant complications if left unrecognized.1Patel SK, Surowiec SM. Venous Insufficiency. [Updated 2024 Feb 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430975/
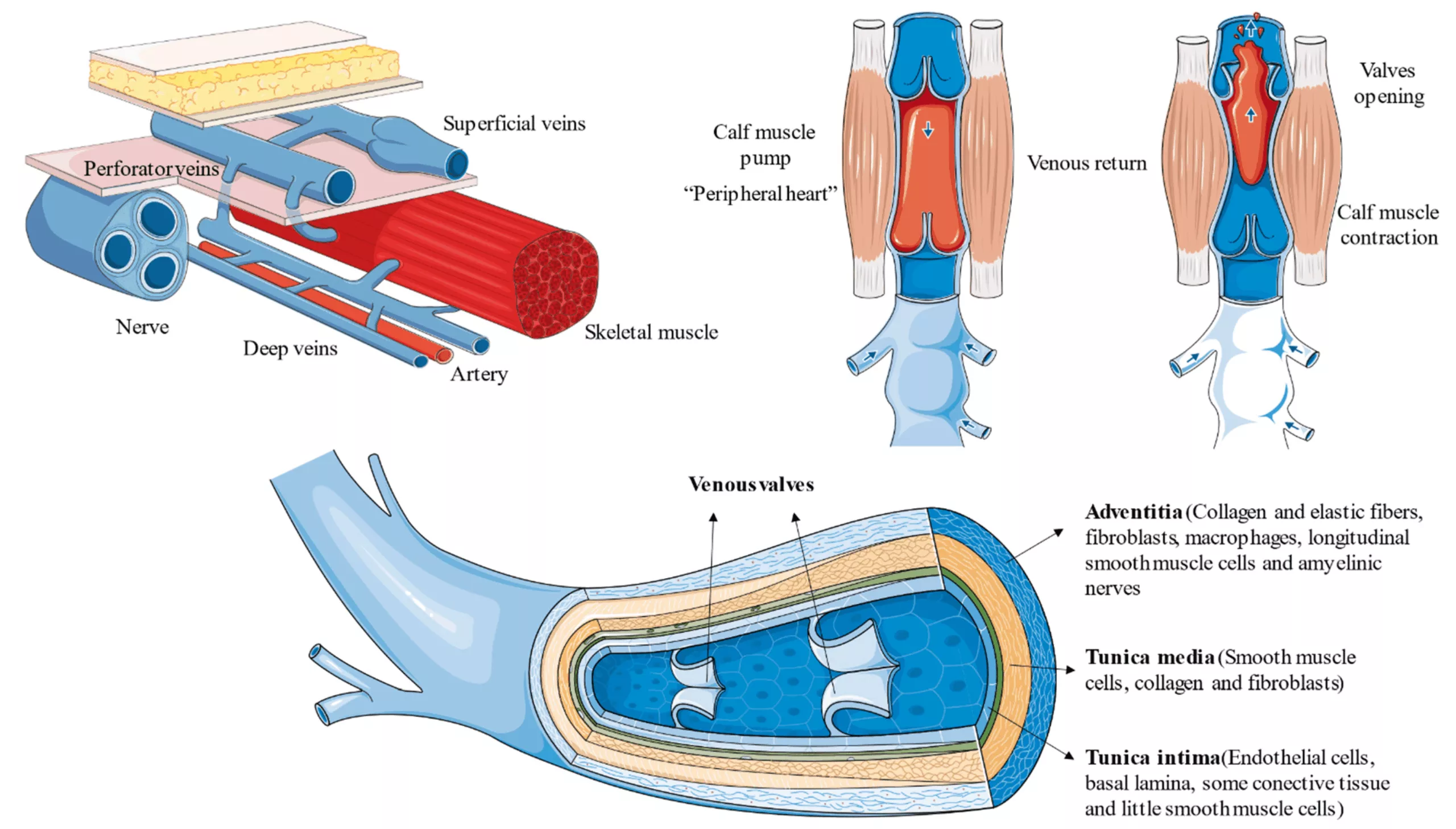
The leg muscles act as musculoskeletal pumps along with a system of veins with one-way valves. The purpose of valves is one-directional upward movement of de-oxygenated blood by overcoming the force of gravity. When one or more of these valves becomes weak and cannot help push the blood up, it pools in the legs. This raises the venous pressure, causes tissue damage and severe, crippling symptoms like pain, swelling, skin changes, and venous ulcers. However, with modern treatment options, it is easy to limit this progression.
Prevalence of Venous Insufficiency
It is very hard to determine the exact prevalence of venous insufficiency because there are too many differences in the study designs, diagnostic definitions, and population demographics of the studies. Still, the condition is more common than you think.
According to most global studies, we estimate the prevalence rate to be between <1% to 40% in women and <1% to 17% in men, depending on the particular population and definitions used.2 Beebe-Dimmer, J. L., Pfeifer, J. R., Engle, J. S., & Schottenfeld, D. (2005). The Epidemiology of Chronic Venous Insufficiency and Varicose Veins. Annals of Epidemiology, 15(3), 175-184. https://doi.org/10.1016/j.annepidem.2004.05.015 This rate rises sharply with age and is interestingly higher in developed or urbanized settings.3 Bawakid, K. O., Al-Raddadi, R. M., Sabban, S. S., Alturky, K. A., & Mohamed, M. S. (2005). Prevalence of chronic venous insufficiency in the Saudi adult population. Saudi medical journal, 26(2), 225–229. Sedentary habits and obesity are considered the causative factors. Even with this high rate, many early cases remain undiagnosed, particularly in resource-limited regions where nonspecific symptoms are attributed to aging or “poor circulation.”
Causes of Venous Insufficiency
At the heart of venous insufficiency is the dysfunction of the venous valves; however, there are several causes:
- Valvular Incompetence is the most common cause. The one-way valves don’t close fully, and blood refluxes and pools in the legs.
- Deep vein thrombosis (DVT) or external compression (as with pregnancy, tumors, or pelvic masses) can cause venous obstruction.
- Weakening of venous walls due to aging, an inherited disorder, or chronic venous pressure.
Risk Factors for Venous Insufficiency
Several factors increase the likelihood of developing one or more of the underlying causes listed above. Some of these factors are non-modifiable, but there are several modifiable factors as well.
Non-Modifiable Risk Factors:
- Age: Incidence rises notably after age 50 as vein walls and valves degenerate.
- Genetics (Family History): A strong family history can significantly raise individual’s risk.4 Ortega, M. A., Fraile-Martínez, O., García-Montero, C., Álvarez-Mon, M. A., Chaowen, C., Ruiz-Grande, F., Pekarek, L., Monserrat, J., Asúnsolo, A., García-Honduvilla, N., Álvarez-Mon, M., & Bujan, J. (2021). Understanding Chronic Venous Disease: A Critical Overview of Its Pathophysiology and Medical Management. Journal of Clinical Medicine, 10(15), 3239. https://doi.org/10.3390/jcm10153239
- Sex: Women are disproportionately affected, mainly due to hormonal influences, pregnancy, and hormone therapy.
Modifiable Risk Factors:
- Occupation: Prolonged standing or sitting in professions such as healthcare, teaching, or retail.
- Sedentary Lifestyle: Affects the pumping function of leg muscles, reducing venous return.
- Pregnancy: Increased blood volume, hormonal changes, and uterine pressure contribute to venous wall tone.
- Obesity: Increased intra-abdominal pressure makes venous return harder.
- Medical Comorbidities: Previous deep vein thrombosis (DVT), heart failure, or chronic constipation.
- Prolonged Immobility: Extended travel, postoperative recovery, or bed rest after an injury.
- Smoking: Promotes vascular inflammation and impairs circulation.
Symptoms of Venous Insufficiency
Venous insufficiency is a progressive disease. The symptoms are quite mild in the start, and then with disease progression, become more severe and more disabling. Symptoms typically worsen with standing, and patients often report improvement with leg elevation: this is practically diagnostic.
Early Symptoms:
- Heavy or tired legs typically worsen as the day drags on. It improves with rest or leg elevation.
- Swelling or edema usually occurs near the ankles. The swelling leaves deep sock marks and causes shoes to feel snug.
- Aching, throbbing, or burning pain, worse with prolonged standing, relieved with walking or elevating legs.
- Nighttime leg cramps or “Charlie horses” can be caused by a buildup of metabolic waste products in the muscles from being too inactive.5 B Abola, M. T., Evans, N. S., & Ratchford, E. V. (2022). Vascular Disease Patient Information Page: Leg cramps. Vascular Medicine. https://doi.org/10.1177/1358863X221088869
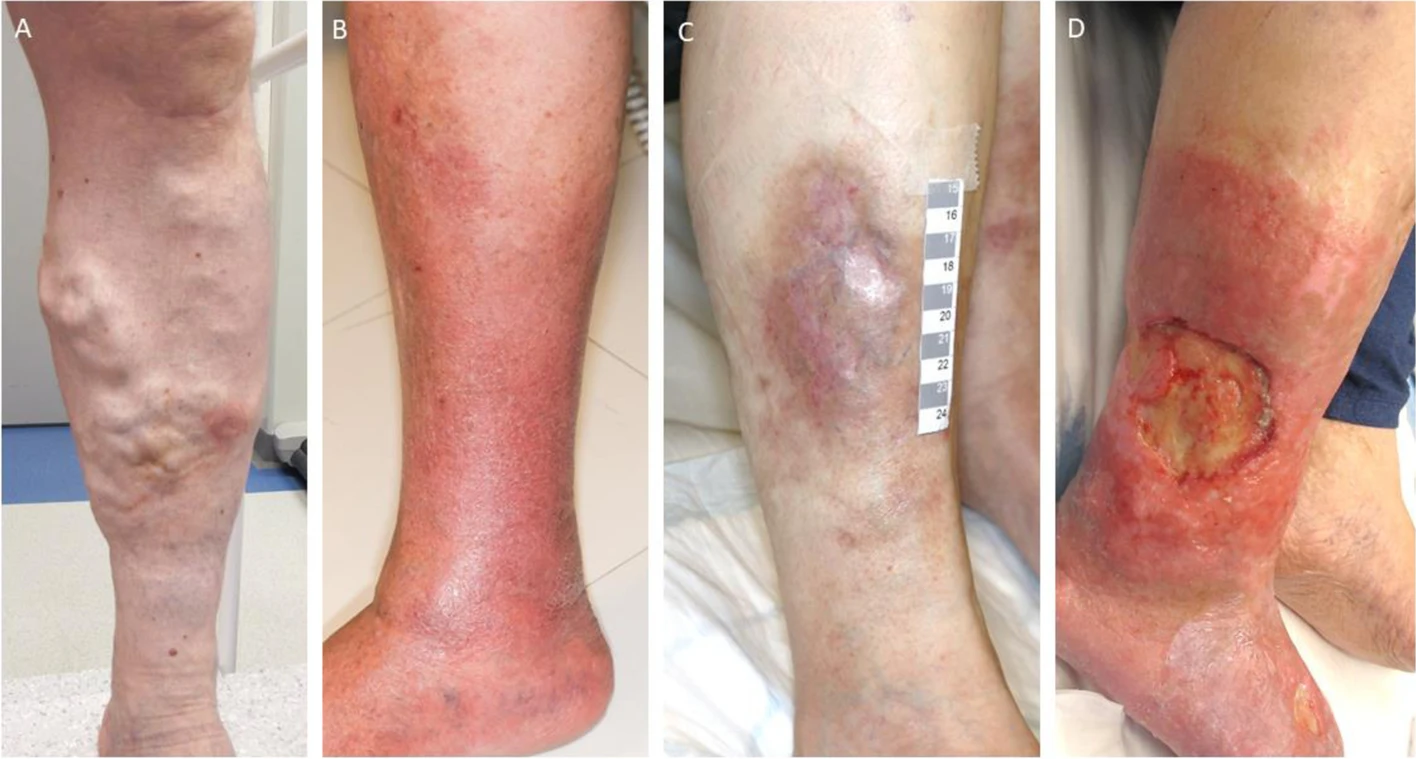
Progressive Visual Changes:
- Fine red or blue veins, spider veins.6 Beebe-Dimmer, J. L., Pfeifer, J. R., Engle, J. S., & Schottenfeld, D. (2005). The Epidemiology of Chronic Venous Insufficiency and Varicose Veins. Annals of Epidemiology, 15(3), 175-184. , that may appear like a spider’s web under the surface of the skin
- Bulging, twisted varicose veins under the skin that resemble a rope and may be dark purple or blue.
While many consider these cosmetic concerns, both spider and varicose veins can also be indicators of venous hypertension in the legs, which can progress.
Skin Changes:
- Brownish, reddish, or purplish discoloration around the ankles due to hemosiderin.
- Hard, leathery textured skin (lipodermatosclerosis), dryness, and eczema-like rashes.
- The skin shows slow healing, even for minor cuts or scratches, because of compromised circulation
Advanced Complications:
- Venous ulcers are open, often painful wounds that form near the ankles. These can become difficult to heal if underlying venous dysfunction isn’t addressed.
Stages of Venous Insufficiency
Venous insufficiency is a broad disease process that can involve a variety of symptoms and complications from mild to severe. To standardize the assessment, clinicians use the CEAP classification system.7Lurie F., Passman M., Meisner M., Dalsing M., Masuda E., Welch H., Bush R.L., Blebea J., Carpentier P.H., De Maeseneer M., et al. The 2020 update of the CEAP classification system and reporting standards. Journal of Vascular Surgery. Venous Lymphat. Disord. 2020;8:342–352. doi: 10.1016/j.jvsv.2019.12.075. It is used by practitioners internationally and guides diagnosis, treatment, and monitoring.
It actually has four primary elements: clinical (symptoms and signs), etiologic (reason for the disease), anatomic (site of involvement), pathophysiologic (site of disease), and clinical severity scale. For all practical purposes, the focus is on the clinical scale because it is the most relevant to patients and general care.
Clinical Classification (C):
This part of CEAP describes the visible and symptomatic stages of venous disease:
- C0: No visible or palpable signs of venous disease
- C1: Telangiectasias (spider veins) or reticular veins (small blue veins)
- C2: Varicose veins
- C3: Edema (swelling), usually around the ankles and lower leg
- C4: Skin changes such as: hyperpigmentation, eczema, lipodermatosclerosis (thickening and hardening of the skin)
- C5: Healed venous ulcers
- C6: Active venous ulcers
This grading system can help in planning care, studying how a condition will likely progress over time, and incorporating an array of treatments for research purposes.
| Clinical Classification | Etiologic Classification | Anatomic Classification | Pathophysiologic Classification | |
|---|---|---|---|---|
| C0 | No visible or palpable signs of venous disease | Ec: Congenital | As: Superficial veins | Pr: Reflux |
| C0s | C0 with minor symptoms | Ep: Primary | Ap: Perforator veins | Po: Obstruction |
| C1 | Telangiectasia or reticular veins | Es: Secondary (postthrombotic) | Ad: Deep veins | Pr,o: Reflux and obstruction |
| C2 | Varicose veins | En: No venous cause identified | An: No venous location identified | Pn: No venous pathophysiology identifiable |
| C3 | Edema | |||
| C4a | Pigmentation and/or eczema | |||
| C4b | Lipodermatosclerosis and/or atrophie blanche | |||
| C5 | Healed venous ulcer | |||
| C6 | Active venous ulcer | |||
| S | Symptomatic, including ache, pain, tightness, skin irritation, heaviness, and muscle cramps, and other complaints attributable to venous dysfunction | |||
| A | Asymptomatic |
The CEAP system (Clinical, Etiological, Anatomical, Pathophysiological) provides a standardized framework for evaluating chronic venous disorders. (Adapted from Mansilha, A., & Sousa, J. (2018). Pathophysiological Mechanisms of Chronic Venous Disease and Implications for Venoactive Drug Therapy. International Journal of Molecular Sciences, 19(6), 1669. Available from MDPI. Licensed under CC by 4.0)
Arterial vs. Venous Insufficiency
Because symptoms sometimes overlap, distinguishing venous insufficiency from arterial insufficiency is crucial.
| Feature | Venous Insufficiency | Arterial Insufficiency8Zemaitis MR, Boll JM, Dreyer MA. Peripheral Arterial Disease. [Updated 2023 May 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430745/ |
|---|---|---|
| Blood Flow Direction | Away from the heart (blocked supply) | Around the ankles, wet and irregular |
| Skin Color | Red/brown discoloration | Pale or bluish tint |
| Pain | Worse after standing | Worse during walking or exertion |
| Ulcers | Around ankles, wet and irregular | On toes/heels, dry and round |
| Pulses | Normal | Decreased or absent |
A misdiagnosis can cause problems because the treatment of venous disease is quite different from the treatment of an arterial disease. Venous disease management usually centers around improving return flow to the heart while reducing high pressures, but arterial disease may require revascularization or anticoagulants.
Diagnosis of Venous Insufficiency
The diagnosis of venous insufficiency requires a combination of a thorough physical examination and targeted imaging. Early and accurate treatment not only provides a diagnosis of the disease but also provides a more targeted plan for the treatment.
Initial Clinical Assessment:
The diagnosis starts by considering care providers exploring:
- Medical History: The timeline and chronicity of your symptoms, family history, occupations, history of previous clots or surgeries.
- Physical exam: Presence of leg swelling, warmth, tenderness, varicosities, skin discoloration, ulcers, and pulse checks in the peripheries.
Primary Diagnostic Test: Duplex Ultrasound:
Duplex ultrasound is the gold standard test for confirming venous insufficiency.9Necas, M. (2010). Duplex ultrasound in the assessment of lower extremity venous insufficiency. Australasian Journal of Ultrasound in Medicine, 13(4), 37-45. https://doi.org/10.1002/j.2205-0140.2010.tb00178.x The test is non-invasive, requires no downtime, and allows visualization of blood flowing through veins. Duplex ultrasound combines two techniques (traditional ultrasound imaging and Doppler imaging) for an accurate diagnosis.
The test takes 30-60 minutes to complete. It uses high-frequency sound waves, aka ultrasound, to study blood flowing through veins. Sound waves do not expose patients to radiation.
Valves in healthy veins close completely and prevent blood from flowing backward. The reflux time is only about 0.5 to 1 second. When valves fail, blood flows backward for a longer time, which confirms venous insufficiency. Duplex ultrasounds allow providers to see which vein segments are affected (superficial veins, deep veins, perforator veins).
Additional Diagnostic Tests (When Needed):
In certain complex cases where duplex ultrasound alone does not provide sufficient information, additional studies may be recommended.
- Air Plethysmography measures volume changes in the leg during different movements.
- MR Venography offers detailed visualization of central veins and congenital abnormalities.
- CT Venography is especially helpful for identifying deep pelvic vein obstructions or complex patterns of blockage.
- Intravascular Ultrasound (IVUS) provides highly detailed internal images of the vein lumen, typically used during endovascular interventions.
Treatment & Management of Venous Insufficiency
Venous insufficiency is usually a very treatable problem, especially when it’s caught in its early stages.
First-Line Conservative Treatments:
Compression Therapy
Compression stockings remain the gold standard for initial management. Medical-grade compression (typically 20–30 mmHg) applies graduated pressure (highest at the ankle and decreasing upward) to improve venous return and reduce swelling. Daily use is recommended, especially during active hours.10Shammeri, O. A., AlHamdan, N., Midhet, F., Hussain, M., & Al-Mohaimeed, A. (2014). Chronic Venous Insufficiency: Prevalence and effect of compression stockings. International Journal of Health Sciences, 8(3), 231. https://doi.org/10.12816/0023975
Lifestyle Modifications
- Regular exercise, like walking, swimming, or calf raises, to strengthen the calf muscles
- Elevate legs above heart level for 15–20 minutes, 3–4 times per day, to promote venous drainage.
- Maintain a healthy weight to reduce venous pressure.
- Avoid prolonged standing or sitting: take short walks or stretch every 30 minutes.
- Stay hydrated for optimal blood volume and circulation.
Occupational Strategies
When long periods of standing or sitting are inevitable (e.g., healthcare workers, teachers, retail employees), there are ways to improve symptoms without taking away from work: walk breaks throughout the day, foot exercises, wearing compression stockings, leg elevation when possible, and desk footrests.
Medical Therapies
Although not curative, certain medications are regularly used to provide symptom relief:
- Venoactive drugs (e.g., micronized purified flavonoid fraction – MPFF) can decrease leg pressure and reduce swelling.11Manjit S. Gohel, Alun H. Davies, Pharmacological Agents in the Treatment of Venous Disease: An Update of the Available Evidence, Current Vascular Pharmacology; Volume 7, Issue 3, Year 2009, doi: 10.2174/157016109788340758
- Anti-inflammatory medications for pain and discomfort.
- Diuretics may be prescribed in cases of extreme edema, though should not be taken long-term.
- Topical wound care products for managing complications like ulcers.
Specialized care is needed when treating open wounds in individuals with venous ulcers. This often includes:
- Advanced dressings to promote healing
- Compression bandaging systems
- Strict infection prevention
- Regular wound monitoring and follow-up
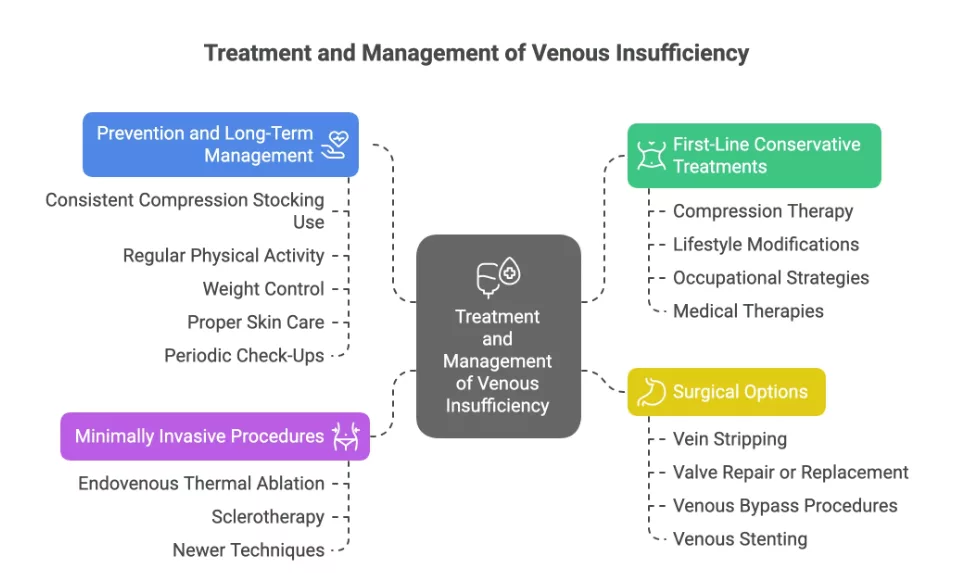
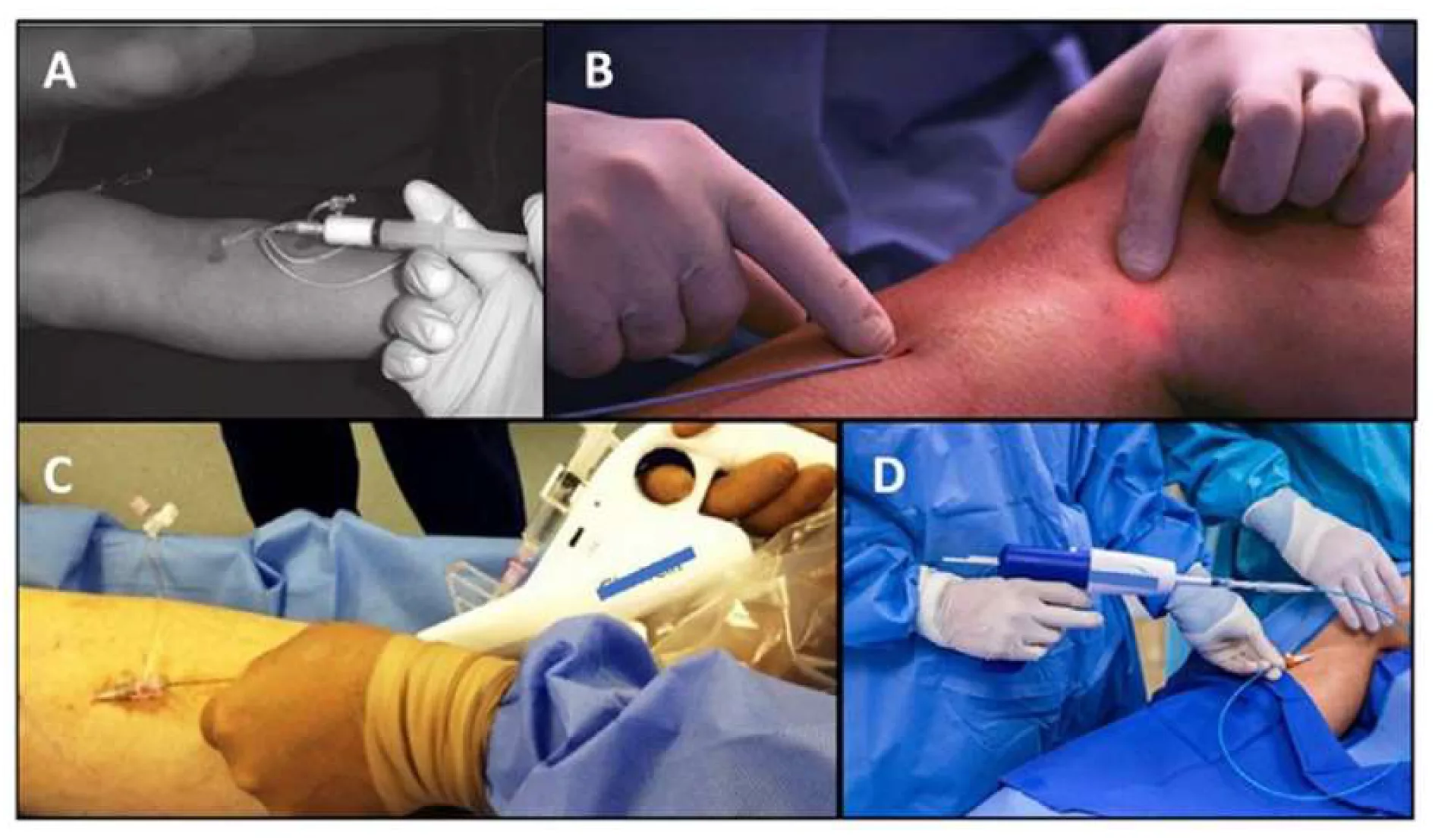
Minimally Invasive Procedures:
When conservative measures fail or varicose veins are more advanced, there are several minimally invasive options:
Endovenous Thermal Ablation
This includes:
- Radiofrequency ablation (RFA)
- Endovenous laser therapy (EVLT)
Both treatments use heat energy to close or “ablate” diseased veins, allowing blood to reroute through normal vessels. These procedures are performed in the office setting, under local anesthesia, and have high success rates (often >95%). Patients can resume normal activities within 24–48 hours.12Attaran, R. R. (2018). Latest Innovations in the Treatment of Venous Disease. Journal of Clinical Medicine, 7(4), 77. https://doi.org/10.3390/jcm7040077
Sclerotherapy
This procedure involves the injection of a sclerosing agent directly into the vein, causing it to collapse and be reabsorbed. It is particularly effective for spider veins and smaller varicose veins.
Newer Techniques
- Mechanochemical ablation is a combination of two techniques: mechanical disruption and sclerosing injection.13Razaque, A., Shazlee, M. K., Qamar, S., Hyder, S. M. S., & Adel, H. (2023). Early Results of Mechanochemical Ablation by Flebogrif and Radiofrequency Ablation in Treating Primary Varicose Veins of Lower Limb. Cureus, 15(9), e45874. https://doi.org/10.7759/cureus.45874
- Adhesive closure systems (cyanoacrylate embolization) seal veins using medical-grade glue with minimal discomfort.
- Ambulatory phlebectomy allows physical removal of veins through tiny skin incisions.
Surgical Options:
Though rarely needed today, surgery remains necessary in certain advanced or refractory cases:
- Vein stripping (largely outdated) involves the removal of the affected vein.
- Valve repair or replacement may be attempted in select patients with valve incompetence.
- Venous bypass procedures may be considered in cases of extensive blockage.
- Venous stenting can be used to address central venous obstruction.
Prevention & Long-Term Management
Even with treatment, venous insufficiency is chronic, but recurrence can be prevented through:
- Consistent compression stocking use
- Regular physical activity
- Weight control
- Proper care for skin changes or ulcers
- Periodic check-ups with a vascular specialist
- Avoiding prolonged standing or sitting
Importantly, awareness is key. Many people normalize leg discomfort as “part of getting older,” delaying treatment until serious complications develop. Culturally sensitive patient education is essential to promote earlier diagnosis and care.
Conclusion
Venous insufficiency is a slowly progressive condition. Fortunately, we can treat it and prevent complications with early detection and management by using simple compression therapy and patient education. For clinicians, especially in resource-limited settings, raising awareness and using cost-effective diagnostic tools like duplex ultrasound can help patients improve their quality of life to a significant extent.
If you notice leg fatigue, swelling, or visible vein changes, don’t wait for any complications to set in. Nowadays, most patients can manage chronic venous insufficiency and have an excellent quality of life taking advantage of the modern treatment options available.
Refrences
- 1Patel SK, Surowiec SM. Venous Insufficiency. [Updated 2024 Feb 14]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430975/
- 2Beebe-Dimmer, J. L., Pfeifer, J. R., Engle, J. S., & Schottenfeld, D. (2005). The Epidemiology of Chronic Venous Insufficiency and Varicose Veins. Annals of Epidemiology, 15(3), 175-184. https://doi.org/10.1016/j.annepidem.2004.05.015
- 3Bawakid, K. O., Al-Raddadi, R. M., Sabban, S. S., Alturky, K. A., & Mohamed, M. S. (2005). Prevalence of chronic venous insufficiency in the Saudi adult population. Saudi medical journal, 26(2), 225–229.
- 4Ortega, M. A., Fraile-Martínez, O., García-Montero, C., Álvarez-Mon, M. A., Chaowen, C., Ruiz-Grande, F., Pekarek, L., Monserrat, J., Asúnsolo, A., García-Honduvilla, N., Álvarez-Mon, M., & Bujan, J. (2021). Understanding Chronic Venous Disease: A Critical Overview of Its Pathophysiology and Medical Management. Journal of Clinical Medicine, 10(15), 3239. https://doi.org/10.3390/jcm10153239
- 5B Abola, M. T., Evans, N. S., & Ratchford, E. V. (2022). Vascular Disease Patient Information Page: Leg cramps. Vascular Medicine. https://doi.org/10.1177/1358863X221088869
- 6Beebe-Dimmer, J. L., Pfeifer, J. R., Engle, J. S., & Schottenfeld, D. (2005). The Epidemiology of Chronic Venous Insufficiency and Varicose Veins. Annals of Epidemiology, 15(3), 175-184.
- 7Lurie F., Passman M., Meisner M., Dalsing M., Masuda E., Welch H., Bush R.L., Blebea J., Carpentier P.H., De Maeseneer M., et al. The 2020 update of the CEAP classification system and reporting standards. Journal of Vascular Surgery. Venous Lymphat. Disord. 2020;8:342–352. doi: 10.1016/j.jvsv.2019.12.075.
- 8Zemaitis MR, Boll JM, Dreyer MA. Peripheral Arterial Disease. [Updated 2023 May 23]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK430745/
- 9Necas, M. (2010). Duplex ultrasound in the assessment of lower extremity venous insufficiency. Australasian Journal of Ultrasound in Medicine, 13(4), 37-45. https://doi.org/10.1002/j.2205-0140.2010.tb00178.x
- 10Shammeri, O. A., AlHamdan, N., Midhet, F., Hussain, M., & Al-Mohaimeed, A. (2014). Chronic Venous Insufficiency: Prevalence and effect of compression stockings. International Journal of Health Sciences, 8(3), 231. https://doi.org/10.12816/0023975
- 11Manjit S. Gohel, Alun H. Davies, Pharmacological Agents in the Treatment of Venous Disease: An Update of the Available Evidence, Current Vascular Pharmacology; Volume 7, Issue 3, Year 2009, doi: 10.2174/157016109788340758
- 12Attaran, R. R. (2018). Latest Innovations in the Treatment of Venous Disease. Journal of Clinical Medicine, 7(4), 77. https://doi.org/10.3390/jcm7040077
- 13Razaque, A., Shazlee, M. K., Qamar, S., Hyder, S. M. S., & Adel, H. (2023). Early Results of Mechanochemical Ablation by Flebogrif and Radiofrequency Ablation in Treating Primary Varicose Veins of Lower Limb. Cureus, 15(9), e45874. https://doi.org/10.7759/cureus.45874