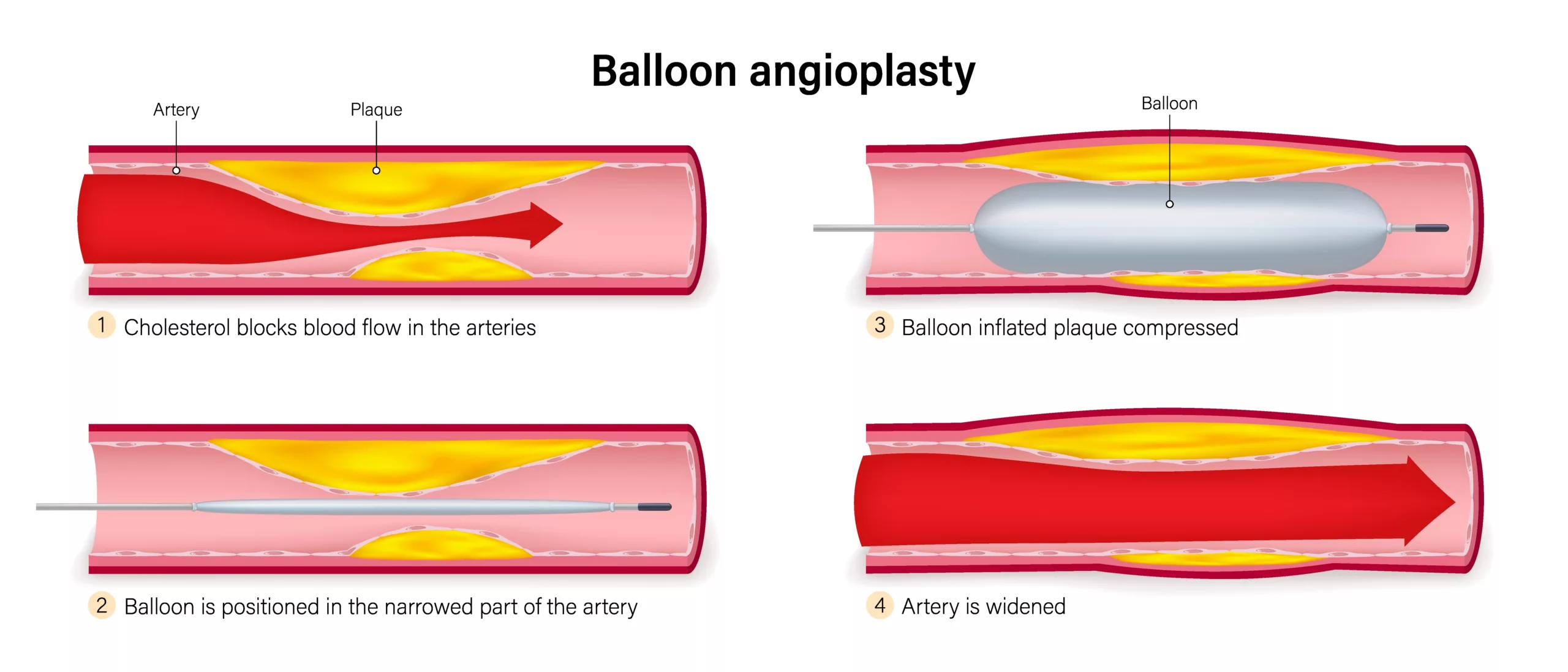
Angioplasty or balloon angioplasty is an advanced, minimally invasive procedure to clear obstructions in blocked or narrowed arteries. Mostly, coronary artery disease (CAD) patients undergo this non-surgical procedure in a catheter lab. In almost all cases, the interventionist places a stent after clearing the obstruction with a balloon and a catheter. Previously, the process of balloon angioplasty and stent placement was known as Percutaneous transluminal coronary angioplasty (PCTA), but now it is called Percutaneous coronary intervention (PCI).1Malik, T. F., & Tivakaran, V. S. (2023). Percutaneous transluminal coronary angioplasty. In StatPearls [Internet]. StatPearls Publishing. It is a common cardiac procedure, with over 965,000 angioplasty procedures performed yearly in the US alone.2iData Research. (n.d.). *Over 965,000 angioplasties are performed each year in the United States*. Retrieved from https://idataresearch.com/over-965000-angioplasties-are-performed-each-year-in-the-united-states/#:~:text=According%20to%20the%20latest%20interventional,open%20blocked%20or%20narrowing%20arteries. Balloon angioplasty improves vessel blood flow and helps alleviate symptoms caused by the blockage.
Balloon Angioplasty Vs. Stent
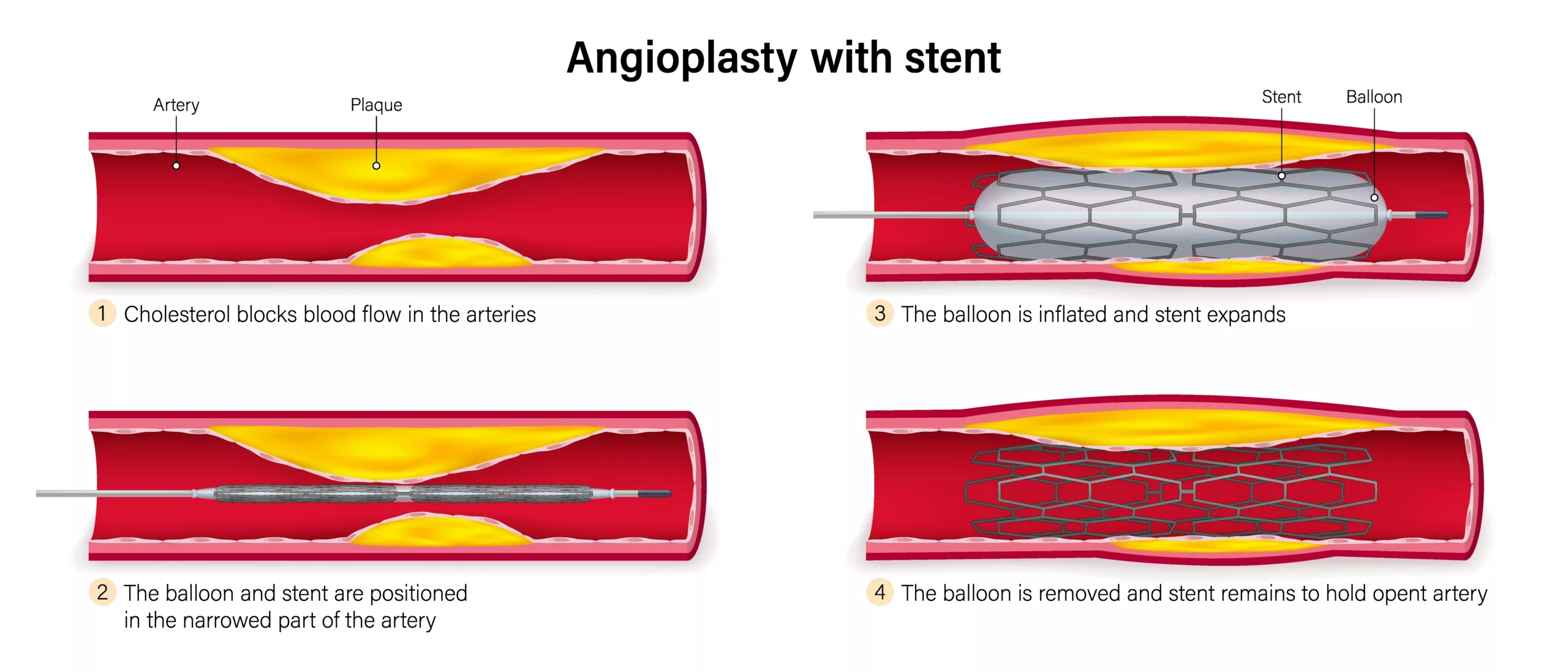
A coronary stent is a medical appliance that keeps the vessel lumen open. It is wire mesh in the form of a tube. Doctors place a stent after carrying out balloon angioplasty. This prevents the artery from collapsing again, i.e., restenosis.
Types Of Balloon Angioplasty
Based on the type of materials used, balloon angioplasty is divided into three types:3Mechanisms and Treatment of Femoropoplitealin-Stent Restenosis – Scientific Figure on ResearchGate. Available from: https://www.researchgate.net/figure/Types-of-balloon-angioplasty-a-conventional-balloon-b-cutting-balloon-and-c_fig4_339999736 [accessed 18 Sept 2024]
Conventional/Classic Balloon Angioplasty:
It is a highly prevalent method that utilizes a “simple” balloon to clear arterial occlusions.
Cutting Balloon Angioplasty:
It minimizes vessel injury and prevents excessive stretching by scoring the vessel in a longitudinal direction (instead of uncontrollably disrupting plaques).4Lee, M. S., Singh, V., Nero, T. J., & Wilentz, J. R. (2002). Cutting balloon angioplasty. The Journal of Invasive Cardiology, 14(9), 552-556. Studies show that the cutting balloon technique uses fewer balloons and has a lesser incidence of error (balloon slippage).5Albiero, R., Silber, S., Di Mario, C., Cernigliaro, C., Battaglia, S., Reimers, B., … & RESCUT investigators. (2004). Cutting balloon versus conventional balloon angioplasty for the treatment of in-stent restenosis: results of the restenosis cutting balloon evaluation trial (RESCUT). Journal of the American College of Cardiology, 43(6), 943-949.
Drug-Coated Balloon Angioplasty (DCB):
It is similar to the conventional balloon angioplasty. In this procedure, the balloon is coated with an anti-proliferative drug/agent that prevents post-operative reduction in arterial diameter, i.e., restenosis. Many cardiac interventionists prefer this technique due to its therapeutic benefits.6Lei, G. A. O., & Yun-Dai, C. H. E. N. (2016). Application of drug-coated balloon in coronary artery intervention: challenges and opportunities. Journal of Geriatric Cardiology: JGC, 13(11), 906.
Indications For Balloon Angioplasty
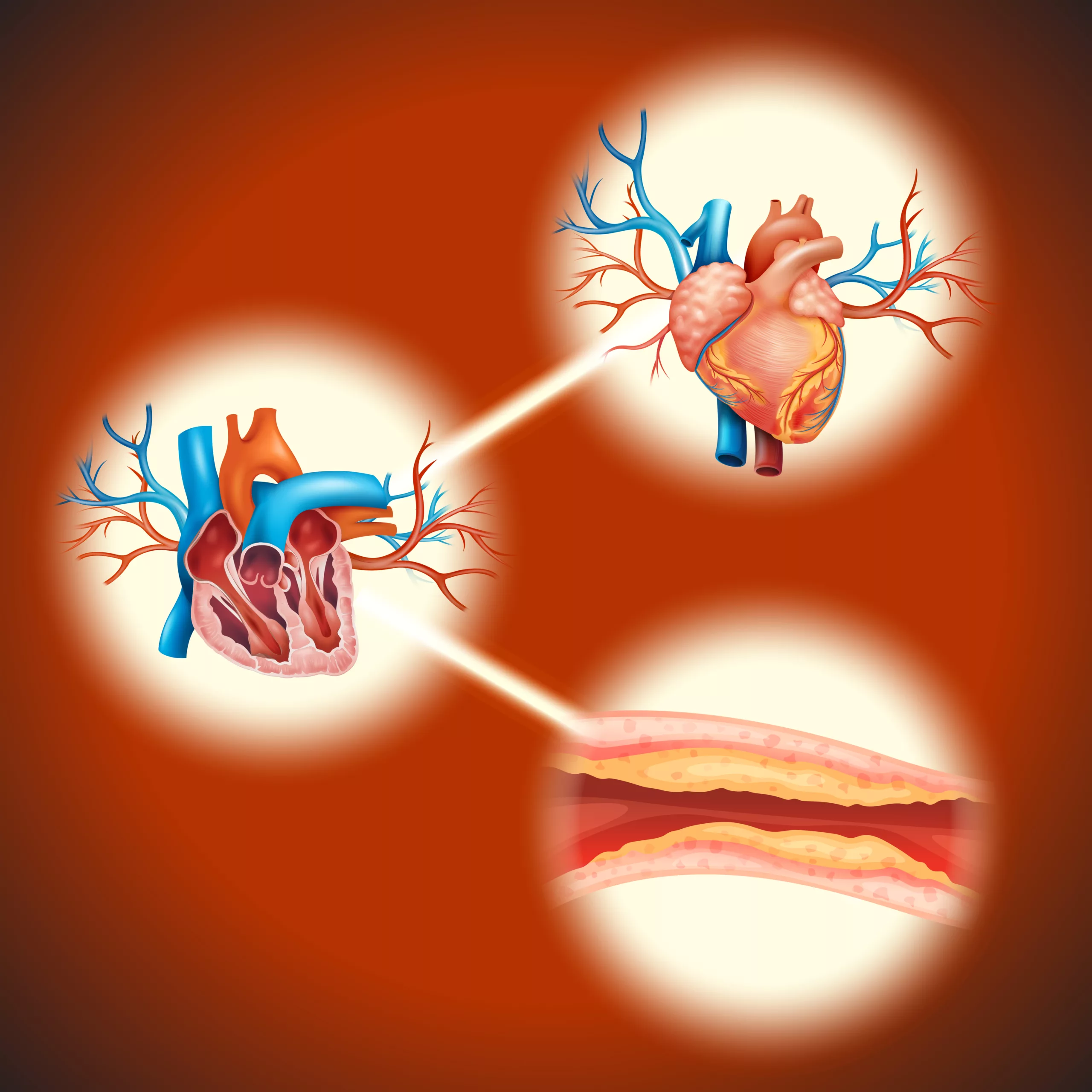
This interventional treatment strategy opens up clogged arteries. Atherosclerosis is the condition of plaque buildup in arteries that causes the narrowing of the vessels. Multiple factors cause fat molecules (cholesterol) deposition in your arteries (especially coronary arteries). The deposited materials harden over time, leading to reductions in blood flow and consequent complications. Angioplasty is a non-surgical solution to remove this buildup. The conditions in which angioplasty is indicated include:
Coronary Artery Disease (CAD)
The most common use of angioplasty is in coronary artery disease patients. Blockage in the heart’s arteries reduces blood flow to the heart muscle, weakening it. Therefore, a weak heart muscle is unable to pump blood optimally, leading to further consequences. According to a clinical study, percutaneous coronary intervention has 10-year follow-up results similar to surgery (Coronary artery bypass graft) patients.7Thuijs, D. J., Kappetein, A. P., Serruys, P. W., Mohr, F. W., Morice, M. C., Mack, M. J., … & Gershlick, A. (2019). Percutaneous coronary intervention versus coronary artery bypass grafting in patients with three-vessel or left main coronary artery disease: 10-year follow-up of the multicentre randomized controlled SYNTAX trial. The Lancet, 394(10206), 1325-1334.
Angina
A common consequence of CAD is angina, i.e., chronic chest pain due to compromised blood flow to the heart muscle. Coronary intervention is a suitable option for patients who do not respond to conventional anti-anginal medications. Angina can lead to myocardial infarction. Therefore, it is important to minimize the issue.
Heart Attack (Myocardial Infarction)
Doctors suggest performing an angioplasty within the first few hours after a heart attack to minimize complications. An emergency coronary angioplasty followed by stent placement can be life-saving for a heart attack patient. Balloon angioplasty of the culprit artery in acute ST-elevated myocardial infarction (STEMI) keeps cardiovascular complications at bay. Moreover, some researchers suggest to treat the non-infarct arteries as well.8Wald, D. S., Morris, J. K., Wald, N. J., Chase, A. J., Edwards, R. J., Hughes, L. O., … & Oldroyd, K. G. (2013). Randomized trial of preventive angioplasty in myocardial infarction. New England Journal of Medicine, 369(12), 1115-1123.
Peripheral Artery Disease (PAD)
When the arteries in the legs narrow, the condition is called peripheral artery disease. It is similar to coronary artery disease, as it is also characterized by the deposition of fats leading to blood flow obstruction. The disorder presents with multiple issues, but the most notable is claudication (leg pain during walking). Thus, restoring normal leg blood flow and alleviating symptoms is crucial.
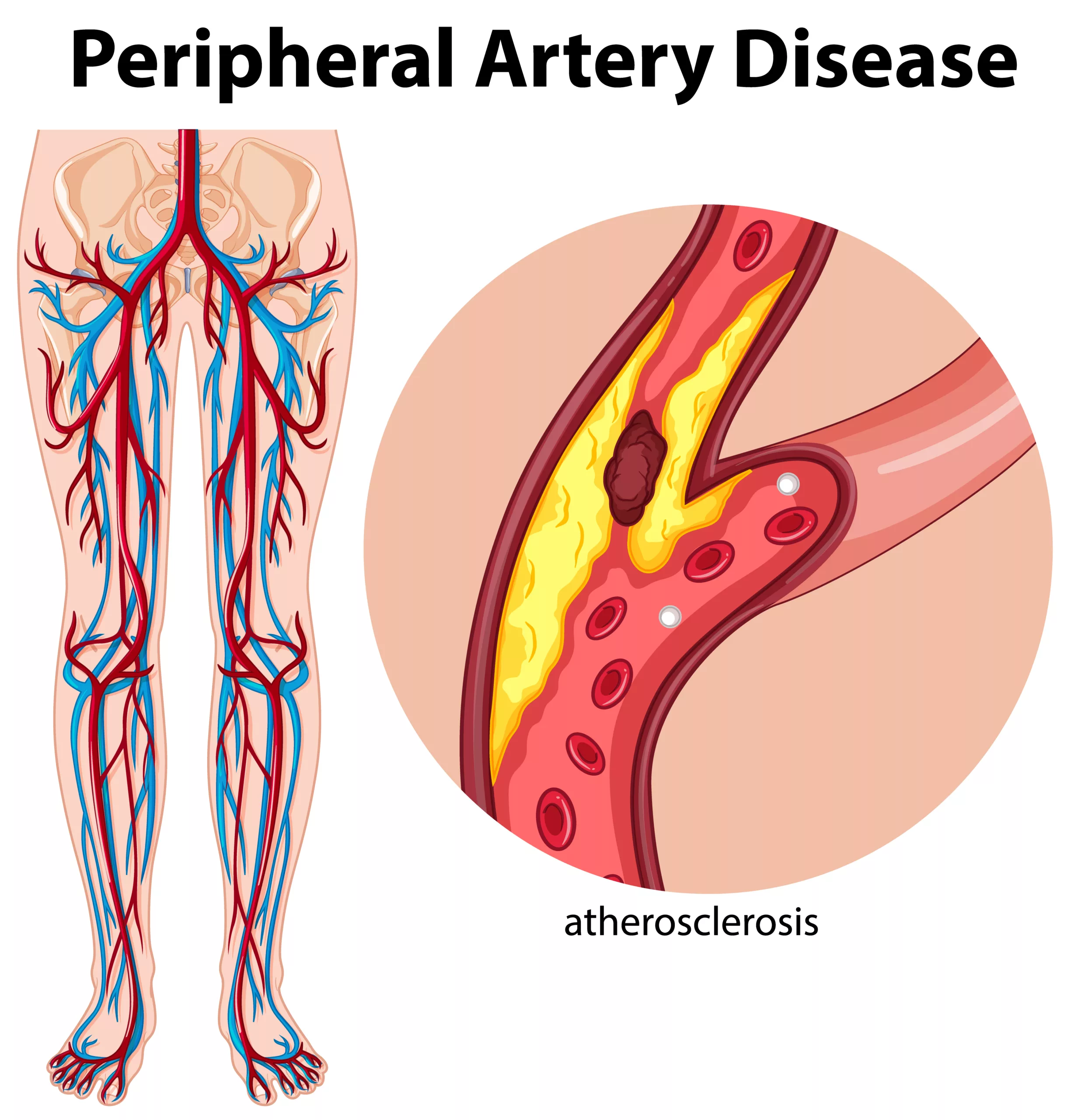
Interventionists perform balloon angioplasty to relieve symptoms of PAD. Drug-coated and standard percutaneous transluminal angioplasty procedures have positive outcomes when treating below-the-knee PAD cases.9Ipema, J., Huizing, E., Schreve, M. A., de Vries, J. P. P., & Ünlü, Ç. (2020). Editor’s Choice–Drug coated balloon angioplasty vs. standard percutaneous transluminal angioplasty in below-the-knee peripheral arterial disease: a systematic review and meta-analysis. European journal of vascular and endovascular surgery, 59(2), 265-275. Studies advocate drug-coated balloon angioplasty in peripheral artery disease treatment.10Colleran, R., Harada, Y., Cassese, S., & Byrne, R. A. (2016). Drug-coated balloon angioplasty in the treatment of peripheral artery disease. Expert review of medical devices, 13(6), 569-582.
Transluminal balloon angioplasty is a risky but effective treatment option for cerebral vasospasm. Other conditions that can benefit from angioplasty procedures include renal artery stenosis and subclavian vein stenosis.
Who is not Eligible for a Balloon Angioplasty
There are certain cases in which doctors can not perform a balloon angioplasty.
Thin Vessels
Doctors offer balloon angioplasty alternatives to patients with thin coronary arteries. The minimum safe vessel diameter for the procedure is 1.5mm. Balloon angioplasty entails a risk of vessel rupture in patients with thin arteries. Thus, it is avoided.
Completely Occluded Arteries
Patients with complete occlusion (chronic total occlusion) are candidates for bypass surgery i.e., Coronary artery bypass graft (CABG). Moreover, patients with triple-vessel disease can not undergo angioplasty. A conventional angioplasty can not open completely blocked arteries. Generally, severe calcifications contribute to hard blockage.
Underlying Health Issues
People who can’t tolerate antiplatelet therapy are not eligible for angioplasty. Interventionists avoid intervention procedures in patients with a high risk of bleeding and those who have recently suffered from a hemorrhagic stroke. Patients allergic to stents or X-ray dye also make it to the list of candidates ineligible for PCI.
Balloon Angioplasty Advantages
Alleviates Symptoms Of Angina
Balloon angioplasty significantly alleviates symptoms of angina. This allows the patient to resume normal activities and leads to evident improvements in quality of life. Clinical trials prove that balloon angioplasty and stent placement in stable angina patients lead to lower angina symptoms and better health status.11Rajkumar, C. A., Foley, M. J., Ahmed-Jushuf, F., Nowbar, A. N., Simader, F. A., Davies, J. R., … & Al-Lamee, R. K. (2023). A placebo-controlled trial of percutaneous coronary intervention for stable angina. New England Journal of Medicine, 389(25), 2319-2330.
Relieves Peripheral Artery Disease
Patients receiving medicinal drugs for PAD can get better results with adjunctive angioplasty therapy. Percutaneous transluminal angioplasty (balloons and stents) improves clinical outcomes in patients with peripheral artery disease.12Shamaki, G. R., Markson, F., Soji-Ayoade, D., Agwuegbo, C. C., Bamgbose, M. O., & Tamunoinemi, B. M. (2022). Peripheral artery disease: a comprehensive updated review. Current Problems in Cardiology, 47(11), 101082.
Improves Blood Flow
The main aim of angioplasty is to remove occlusions and enhance blood flow. The betterment in symptoms (of CAD, PAD, etc.) is attributed to enhancements in blood flow augmentation. Thus, patients experience boosts in generalized health following balloon angioplasty procedures.
Prevents Further Heart Damage
Percutaneous coronary intervention for ST-elevation myocardial infarction (STEMI) patients helps prevent further heart damage. PCI opens up the artery lumen to improve flow. The enhanced blood flow saves the heart from disintegration. Therefore, there are no significant major adverse cardiovascular events (MACE) after 1 year of treatment.13Hao, X., Huang, D., Wang, Z., Zhang, J., Liu, H., & Lu, Y. (2021). Study on the safety and effectiveness of drug-coated balloons in patients with acute myocardial infarction. Journal of Cardiothoracic Surgery, 16, 1-7.
Is Balloon Angioplasty a Safe Procedure?
Yes, balloon angioplasty is a safe procedure. Patients ineligible for balloon angioplasty are advised to have cardiac surgery, such as coronary artery bypass graft (CABG).
What To Do Before Balloon Angioplasty?
You need to follow specific instructions before undergoing angioplasty.
- Doctors advise patients to follow NPO, i.e., nothing by mouth. Patients should avoid eating or drinking a few hours before the procedure. You need to stop solid foods 6 hours before the procedure. However, you can take liquids till 2 hours before angioplasty.
- Stop anticoagulants (blood thinning medicines) and diabetes medications according to doctor’s guidelines. Most doctors advise avoiding anticoagulants 48 hours before the procedure. A list of drugs that need to be temporarily ceased includes aspirin, warfarin, clopidogrel, metformin, insulin, naproxen, celecoxib, ibuprofen, etc. (Note: Strictly follow your doctor’s guidelines regarding drug intake)
- Avoid smoking at least 24 hours before the angioplasty procedure.
- Wear easy clothes that are easy to take off and put back on. You will be given a hospital gown for the procedure. Therefore, easy clothes save time when changing.
- Leave metal items at home. You should not bring metallic appliances/devices such as wristwatches, eyeglasses, and smartphones with you. It is better to remove dental appliances and piercings before the procedure.
Balloon Angioplasty Preparation
Case Evaluation:
Imaging Studies
You will need to visit the doctor for pre-operative evaluation before angioplasty. After taking a complete patient history, doctors perform a physical examination. To get a clearer picture of the obstruction, your interventionist may order different imaging studies, including:
- CT scans
- MRI angiography
- Doppler ultrasound
- Ankle-brachial index test (for peripheral artery disease)
Determination of Entrance Point
This evaluation is also important to determine the entry path for the balloon/catheter, i.e., the femoral artery/vein in the leg or the radial artery in the forearm.
Balloon Angioplasty Procedure
Nurse Management
On the dee-day, you are given a hospital gown. The health staff starts by noting your vital signs (body temperature, heart rate, and blood pressure). Usually, a nurse clamps a pulse oximeter on your finger (to monitor blood oxygen levels) and electrocardiogram electrodes to your chest. An IV line is maintained in a vein to administer anesthesia, medications, etc.

In The Cath Lab
After the setup, the interventionist’s job starts, and the procedure is done in the following steps:
- The doctor gives anesthesia to make the procedure pain-free. Most professionals prefer local or regional anesthesia. General anesthesia is rarely used.
- Then, the doctor makes a small incision in the skin to access the artery/vein.
- The interventionist then guides an introducer sheath into the selected vessel, followed by a thin guidewire.
- A contrast dye is then injected into the body. This allows the doctor to view the catheter.
- Under video guidance, the guidewire and the sheath reach the heart via the selected vessel. The doctor then directs the catheter to the site of occlusion.
- Once at the site of the obstruction, the doctor slowly inflates the balloon (present at the tip of the catheter) at the center of the obstruction.
- The balloon is kept in the inflated position for a few minutes before being deflated. You might experience some discomfort during the inflation period, but it usually goes away when the balloon is deflated.
- Your doctor may opt for a drug-coated balloon to prevent artery collapse (restenosis). In case of multiple obstructions, the doctor repeats steps 5 and 6 for every blockage.
- In almost all procedures, the interventionist places a stent in the opened passageway. For this, the doctor inserts another catheter via the guidewire.
- After successful stent placement, the doctor fully expands the stent and locks it in position to keep the artery open.
- Additional X-rays (usually from different angles) are taken to ensure restoration of blood flow in the previously clogged region.
- The doctor then removes the catheter, guide wire, and the introducer sheath and closes the incision site with sutures.
How Long Does Balloon Angioplasty Take?
The procedure generally takes 1 to 2.5 hours to complete. The duration of angioplasty depends on the severity of the condition and the location of the blockage.
Post-Operative Procedures
The staff then moves the patient to the post-anesthetic care unit, where nurses monitor the patient carefully until the patient regains complete consciousness (for general anesthesia and conscious sedation patients).
Nurses take your vital signs, and if everything is normal, you are transferred to a hospital room. Most patients spend at least one night under observation (in the hospital). However, depending on your condition, you may need to stay longer.
Balloon Angioplasty Recovery & Healing
Most healthcare professionals remove bandages after 24 hours and instruct the patient to keep the wound clean and dry. To lower the wound inflammation, painkiller medications and cold compresses can be used.
You may feel nausea, fatigue, and headaches for a few hours after balloon angiography but don’t worry as these symptoms subsided within a few hours. Bruising on the incision site is also common. It will go away after ample rest.
Slight discomfort and fatigue are common after angioplasty. However, you should contact your health provider if you are experiencing any of the following:
- Chest pain
- Shortness of breath
- Fever (or chills)
- Dizziness/Fainting
Are there any risks involved?
Generally, balloon angioplasty is a safe procedure, and most patients have minimal balloon angioplasty risks. The procedure causes minimal pain. Bruising and soreness of the wound site are commonly seen. However, in some cases, balloon angioplasty can lead to artery blockage (in another location) and may induce severe bleeding. Blood clots can block the stents. Moreover, re-narrowing, i.e., restenosis of the artery can take place.
How to care for after Balloon Angioplasty?
- After discharge from the hospital, you must not bathe or expose the wound to excessive water (for 24 hours).
- Limit your activity for a few days and avoid lifting heavy objects.
- Drink ample amounts of water and follow the doctor’s instructions carefully.
- Take your medications regularly. Blood-thinning medicines like clopidogrel and ticagrelor are very important as they reduce the risk of blood clotting in the stent.
Final Word
Balloon angioplasty is a minimally invasive procedure to open narrowed/blocked blood vessels. It is most commonly used in coronary artery disease and peripheral artery disease. Mostly done under local anesthesia, angioplasty is a safe procedure that improves blood flow, alleviates symptoms and prevents further damage.
An interventionist inserts a catheter and sheath via an artery/vein in the arm or leg. He then inflates the balloon on the tip of the catheter to open up the vessel. The doctor gets a real-time feed of the process. Drug-coated balloons are frequently used to prevent the collapse of the artery. In almost all cases doctors place a mesh (stent) in place after removing the obstruction. This prevents restenosis. The procedure is carried out in a catheter lab, and the patient is observed overnight. After the process, you should avoid strenuous activities (for a few days), eat a healthy diet, and strictly follow your medicine regimen.
Refrences
- 1Malik, T. F., & Tivakaran, V. S. (2023). Percutaneous transluminal coronary angioplasty. In StatPearls [Internet]. StatPearls Publishing.
- 2iData Research. (n.d.). *Over 965,000 angioplasties are performed each year in the United States*. Retrieved from https://idataresearch.com/over-965000-angioplasties-are-performed-each-year-in-the-united-states/#:~:text=According%20to%20the%20latest%20interventional,open%20blocked%20or%20narrowing%20arteries.
- 3Mechanisms and Treatment of Femoropoplitealin-Stent Restenosis – Scientific Figure on ResearchGate. Available from: https://www.researchgate.net/figure/Types-of-balloon-angioplasty-a-conventional-balloon-b-cutting-balloon-and-c_fig4_339999736 [accessed 18 Sept 2024]
- 4Lee, M. S., Singh, V., Nero, T. J., & Wilentz, J. R. (2002). Cutting balloon angioplasty. The Journal of Invasive Cardiology, 14(9), 552-556.
- 5Albiero, R., Silber, S., Di Mario, C., Cernigliaro, C., Battaglia, S., Reimers, B., … & RESCUT investigators. (2004). Cutting balloon versus conventional balloon angioplasty for the treatment of in-stent restenosis: results of the restenosis cutting balloon evaluation trial (RESCUT). Journal of the American College of Cardiology, 43(6), 943-949.
- 6Lei, G. A. O., & Yun-Dai, C. H. E. N. (2016). Application of drug-coated balloon in coronary artery intervention: challenges and opportunities. Journal of Geriatric Cardiology: JGC, 13(11), 906.
- 7Thuijs, D. J., Kappetein, A. P., Serruys, P. W., Mohr, F. W., Morice, M. C., Mack, M. J., … & Gershlick, A. (2019). Percutaneous coronary intervention versus coronary artery bypass grafting in patients with three-vessel or left main coronary artery disease: 10-year follow-up of the multicentre randomized controlled SYNTAX trial. The Lancet, 394(10206), 1325-1334.
- 8Wald, D. S., Morris, J. K., Wald, N. J., Chase, A. J., Edwards, R. J., Hughes, L. O., … & Oldroyd, K. G. (2013). Randomized trial of preventive angioplasty in myocardial infarction. New England Journal of Medicine, 369(12), 1115-1123.
- 9Ipema, J., Huizing, E., Schreve, M. A., de Vries, J. P. P., & Ünlü, Ç. (2020). Editor’s Choice–Drug coated balloon angioplasty vs. standard percutaneous transluminal angioplasty in below-the-knee peripheral arterial disease: a systematic review and meta-analysis. European journal of vascular and endovascular surgery, 59(2), 265-275.
- 10Colleran, R., Harada, Y., Cassese, S., & Byrne, R. A. (2016). Drug-coated balloon angioplasty in the treatment of peripheral artery disease. Expert review of medical devices, 13(6), 569-582.
- 11Rajkumar, C. A., Foley, M. J., Ahmed-Jushuf, F., Nowbar, A. N., Simader, F. A., Davies, J. R., … & Al-Lamee, R. K. (2023). A placebo-controlled trial of percutaneous coronary intervention for stable angina. New England Journal of Medicine, 389(25), 2319-2330.
- 12Shamaki, G. R., Markson, F., Soji-Ayoade, D., Agwuegbo, C. C., Bamgbose, M. O., & Tamunoinemi, B. M. (2022). Peripheral artery disease: a comprehensive updated review. Current Problems in Cardiology, 47(11), 101082.
- 13Hao, X., Huang, D., Wang, Z., Zhang, J., Liu, H., & Lu, Y. (2021). Study on the safety and effectiveness of drug-coated balloons in patients with acute myocardial infarction. Journal of Cardiothoracic Surgery, 16, 1-7.