Renal Tubular Acidosis (RTA) is a condition in which the kidneys fail to properly regulate the body’s acid-base balance despite normal blood filtration. This results from defects in the renal tubules, where acid excretion or bicarbonate reabsorption is impaired. The primary outcome of this dysfunction is metabolic acidosis, an excess buildup of acid in the body that can lead to symptoms such as muscle weakness, fatigue, bone demineralization, kidney stones, or growth retardation in children. RTA can affect individuals of all ages and, if untreated, may result in significant complications, including chronic kidney disease.
What is Renal Tubular Acidosis?
Renal tubular acidosis, often referred to as RTA, is a group of kidney disorders that impact the kidney’s ability to maintain the body’s acid-base balance effectively. Your kidneys hold a crucial role in preserving this delicate equilibrium, ensuring that your blood’s pH levels stay within a healthy range. Renal tubular acidosis (RTA) happens when the kidneys fail to eliminate acids from the blood as they should. This leads to an excessive level of acid in the blood, a condition known as acidosis. While some level of acidity is typical in the blood, an excess of it can disrupt numerous bodily functions.
Understanding Acid-Base Balance:
The body’s acid-base balance refers to the equilibrium between acids and bases in bodily fluids. It’s regulated by the kidneys, which filter out excess acids and help maintain the right pH level. When this balance is disrupted, it can cause diverse health issues.1Laing, C. M., & Unwin, R. J. (2006). Renal tubular acidosis. Journal of Nephrology, 19, S46-52. Disruptions in the acid-base balance can significantly affect overall health, and prompt management can maintain bodily functions in optimal conditions.
Understanding the Role of Kidneys in Acid-Base Balance:
The kidneys play a pivotal role in n regulating the body’s acid-base stability by excreting extra acids and reabsorbing bicarbonate to neutralize acids.
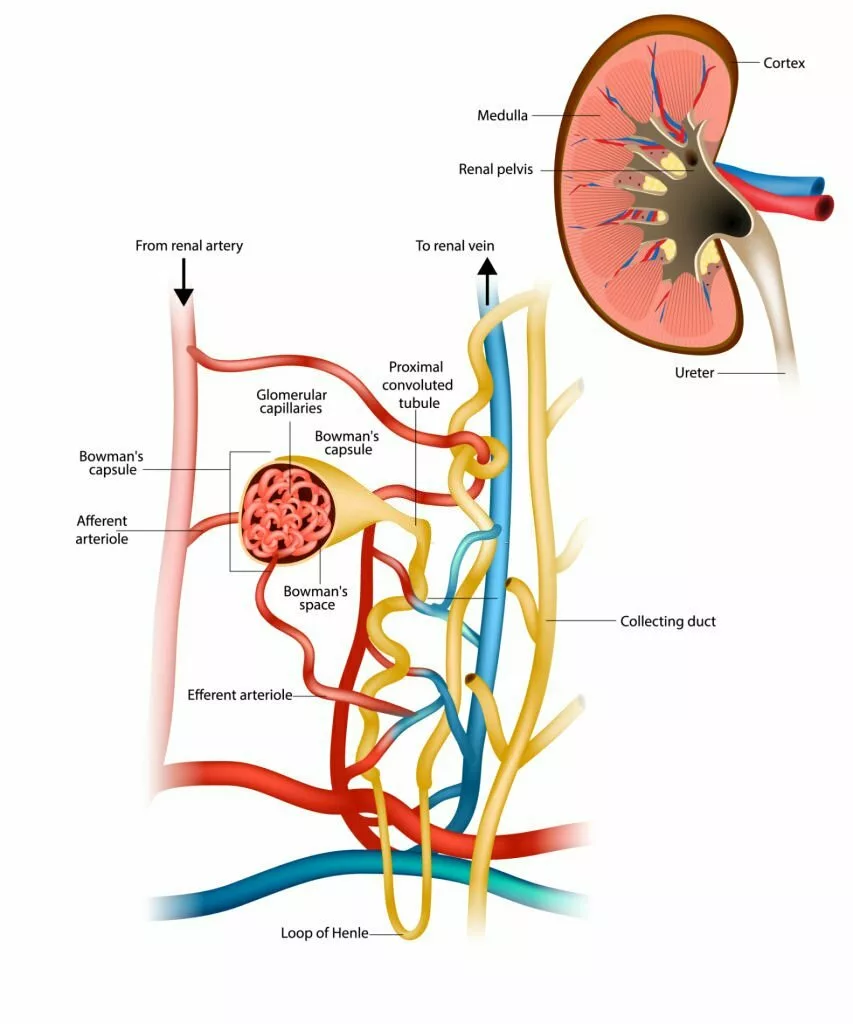
The Role of Renal Tubules
The renal tubules are intricate structures within the kidneys that are responsible for regulating the acid-base balance.2Rajkumar P, Pluznick JL. Acid-base regulation in the renal proximal tubules: using novel pH sensors to maintain homeostasis. Am J Physiol Renal Physiol. 2018 Nov 1;315(5):F1187-F1190. doi: 10.1152/ajprenal.00185.2018. Epub 2018 Aug 1. PMID: 30066586; PMCID: PMC6293293. Any dysfunction in these tubules can contribute to RTA.
When the kidneys filter the blood, the liquid part, called filtrate, travels through tiny tubules in nephrons. Along this journey, there’s an exchange of salts, acidic substances, and other particles before it ultimately becomes urine and heads to the bladder.
Now, when someone has RTA, their kidney either doesn’t release enough acidic hydrogen ions (found in the distal tubule, the latter part of the nephron), or it fails to hold onto enough alkaline bicarbonate ions (found in the proximal tubule, the early part of the nephron), leading to a specific type of metabolic acidosis known as hyperchloremic metabolic acidosis. In this condition, there’s a noticeable decrease in the levels of bicarbonate in the bloodstream, but the anion gap remains within the normal range. Anion Gap essentially measures the difference between the positively charged ions (cations), like sodium and potassium, and the negatively charged ions (anions), including chloride and bicarbonate, present in the blood.
While metabolic acidosis (an acid-related issue) can happen in people with chronic kidney disease, we use the term RTA for individuals whose kidneys work well but struggle to make their urine acidic enough. There are several types of RTA, each with its own set of symptoms and underlying causes.
Types of Renal Tubular Acidosis
There are four main types of RTA.
Distal Renal Tubular Acidosis (Type 1 RTA):
Distal RTA occurs when the kidneys can’t effectively acidify urine in the distal tubules.3Karet, F. E. (2002). Inherited distal renal tubular acidosis. Journal of the American Society of Nephrology, 13(8), 2178-2184. This can result in a higher blood pH stage, inflicting signs consisting of fatigue, muscle weak spots, and a gradual boom in kids.
Proximal Renal Tubular Acidosis (Type 2 RTA):
Proximal RTA involves the impaired reabsorption of bicarbonate in the proximal tubules.4Sebastian, A., McSherry, E., & Morris, R. C. (1971). On the mechanism of renal potassium wasting in renal tubular acidosis associated with the Fanconi syndrome (type 2 RTA). The Journal of Clinical Investigation, 50(1), 231-243.
Additionally, in some cases, proximal RTA can be associated with a condition called Fanconi syndrome. Fanconi syndrome is characterized by the loss of various substances, including bicarbonate, glucose, amino acids, and crucial vitamins, into the urine. This can lead to a range of symptoms, including weakness and bone issues, as essential vitamins and minerals are excreted from the body rather than being absorbed and utilized properly.5Kashoor I, Batlle D. Proximal renal tubular acidosis with and without Fanconi syndrome. Kidney Res Clin Pract. 2019 Sep 30;38(3):267-281. doi: 10.23876/j.krcp.19.056. PMID: 31474092; PMCID: PMC6727890.
Combined Proximal & Distal RTA (Type 3 RTA):
Type 3 RTA is a rare form that combines characteristics of both Type 1 and Type 2. It presents with a mixed set of symptoms and challenges in acid-base regulation. This rare combination can be caused by carbonic anhydrase II deficiency and the use of carbonic anhydrase inhibitors, which block the metabolism of bicarbonate and carbonic acid.
Hyperkalemic or Hyporeninemic Hypoaldosteronism (Type 4 RTA):
This kind is associated with low ranges of the hormone aldosterone. This deficiency can result in elevated blood potassium levels, metabolic acidosis, and disruptions in electrolyte balance. Individuals diagnosed with Type 4 RTA may experience elevated blood potassium levels, which can result in symptoms like muscle weakness and heart issues, including bradycardia, arrhythmias, and even cardiac arrest.6Montford JR, Linas S. How dangerous is hyperkalemia? Journal of the American Society of Nephrology. 2017;28:3155–3165. doi: 10.1681/ASN.2016121344
Renal Tubular Acidosis Causes
The primary causes of RTA involve the following:
Genetic Factors:
Genetic mutations7 Batlle, D., & Haque, S. K. (2012). Genetic causes and mechanisms of distal renal tubular acidosis. Nephrology Dialysis Transplantation, 27(10), 3691-3704. can predispose individuals to inheritable forms of RTA, highlighting the significance of family history in diagnosis. Type 1 RTA is usually inherited.
Autoimmune Diseases:
Conditions like Sjögren’s syndrome and lupus can trigger autoimmune responses that damage the renal tubules, leading to RTA.
Medications and Toxins:
Certain medications and toxins, such as ifosfamide and heavy metals, can interfere with renal tubular function and cause acidosis. Type 2 RTA can be caused by acute lead poisoning and chronic exposure to cadmium.
Chronic Kidney Disease:
Underlying chronic kidney disease can compromise the kidneys’ ability to regulate acid-base balance, culminating in RTA.
Symptoms of Renal Tubular Acidosis
Let’s discuss symptoms of RTA, shedding light on the various signs that indicate an underlying issue with the body’s pH regulation.8Harrington, T. M., Bunch, T. W., & Van Den Berg, C. J. (1983, June). Renal tubular acidosis. A new look at the treatment of musculoskeletal and renal disease. In Mayo Clinic Proceedings (Vol. 58, No. 6, pp. 354-360). Understanding these symptoms can lead to early diagnosis and better management of the condition.
Thirst and Frequent Urination:
One of the initial signs that might raise suspicion of RTA is an unquenchable thirst and frequent urination. This symptom results from the kidneys’ inability to reabsorb water effectively, which leads to the excretion of more fluid in the urine.
As a result, the body compensates by triggering the thirst mechanism, prompting the individual to consume more fluids and eventually leading to more frequent urination.

Electrolyte Imbalance: Weakness and Fatigue:
The disruption in the acid-base balance caused by RTA can lead to an electrolyte imbalance, particularly in the levels of potassium and sodium. This imbalance can result in weakness, fatigue, and even muscle cramps. These symptoms can drastically impact an individual’s daily functioning.
Bone Pain and Osteoporosis:
RTA can also impact the body’s ability to absorb calcium, a vital mineral for maintaining strong bones. Over time, this can lead to bone pain, an increased risk of fractures, and the development of osteoporosis. Individuals with RTA may suffer from bone and joint discomfort due to disruptions in calcium balance.
Acidic Blood pH and Respiratory Distress:
As the name suggests, RTA disturbs the body’s acid-base balance. This disruption can result in a lower-than-normal blood pH, known as acidemia.
Acidemia can lead to respiratory distress, characterized by symptoms such as shortness of breath, rapid breathing, and confusion. This is the body’s attempt to compensate for increased acidity by expelling excess carbon dioxide through rapid respiration.
Growth Impairment in Children:
Untreated RTA can lead to growth impairment in children. The imbalanced acid-base levels can affect the body’s growth hormone production and overall development, resulting in delayed growth milestones and shorter stature.
Kidney Stones and Calcium Deposits:
RTA can increase the danger of kidney stones due to the presence of excess calcium in the urine. These kidney stones may be painful and may require clinical intervention for elimination.9Magni G, Unwin RJ, Moochhala SH. Renal tubular acidosis (RTA) and kidney stones: Diagnosis and management. Arch Esp Urol. 2021 Jan;74(1):123-128. English, Spanish. PMID: 33459628. Additionally, calcium deposits may form in other parts of the body, potentially leading to complications.
Muscle Weakness and Paralysis:
Potassium plays a crucial role in maintaining healthy muscle function, including the muscles responsible for the heart’s contractions. In RTA cases, reduced potassium levels can lead to muscle weakness and, in severe instances, even paralysis. This highlights the significance of timely diagnosis and effective management of RTA.
Visual Disturbances:
In some instances, RTA can lead to disturbances in vision. These disturbances might include blurred vision, sensitivity to light, and even difficulty focusing. These signs may be unsettling and require clinical attention to cope with the underlying acid-base imbalance.
Nausea, Vomiting, and Loss of Appetite:
Gastrointestinal signs and symptoms, along with nausea, vomiting, and lack of appetite, can also be connected to RTA. The imbalanced acid tiers can affect the digestive system, leading to uncomfortable symptoms.
Diagnosing Renal Tubular Acidosis
Medical professionals should contemplate the potential existence of RTA when faced with a patient displaying unexplained metabolic acidosis characterized by a normal anion gap with increased chloride levels. Differentiating between the types of RTA is essential for accurate diagnosis. Distal RTA is characterized by reduced hydrogen ion secretion in the distal tubules, while proximal RTA involves impaired bicarbonate reabsorption in the proximal tubules.
Laboratory Tests:
Medical professionals may recommend blood tests to assess electrolyte levels, kidney function, and acid-base balance. Elevated potassium levels are typically associated with Type 4 RTA, while reduced potassium levels (hypokalemia) are more common in Type 1 (distal) and Type 2 (proximal) RTA. Reduced bicarbonate and a low blood pH (indicating metabolic acidosis) are hallmark findings in all types of RTA.
Urine pH & Electrolyte Levels:
Measuring urine pH and electrolyte concentrations can provide valuable insights into the type of RTA. Distal RTA typically has a higher urine pH, while proximal RTA may lead to excessive electrolyte loss.
Type 1 RTA is diagnosed through a urine pH that stays above 5.5 during systemic acidosis. This acidosis can occur naturally or be triggered by an acid load test involving the oral administration of ammonium chloride at a dose of 100 mg/kg. In contrast, normal kidneys typically lower urine pH to below 5.2 within 6 hours of acidosis onset. This unique urine pH response serves as a distinguishing characteristic of Type 1 RTA.10Renal Tubular Acidosis By L. Aime’e Hechanova, MD, Texas Tech University Health Sciences Center, El Paso Reviewed/Revised May 2022 | Modified Sep 2022 MSD Manual Professional Edition. (n.d.). Retrieved from https://www.msdmanuals.com/professional/genitourinary-disorders/renal-transport-abnormalities/renal-tubular-acidosis#:~:text=Type%202%20RTA%20is%20diagnosed,of%20bicarbonate%20is%20%3E%2015%25.”
Blood Gas Analysis:
Arterial blood gas analysis helps evaluate the body’s acid-base status. A low blood pH and bicarbonate level confirm the presence of acidosis.
Genetic Testing (If Applicable):
In some cases, genetic testing may be recommended, particularly if there is a family history of RTA. Identifying genetic mutations can assist in confirming the diagnosis.
Renal Tubular Acidosis Treatment
Managing a condition like RTA can be challenging, but the good news is that it can be effectively treated by addressing the root cause.11Palmer BF, Kelepouris E, Clegg DJ. Renal Tubular Acidosis and Management Strategies: A Narrative Review. Adv Ther. 2021 Feb;38(2):949-968. doi: 10.1007/s12325-020-01587-5. Epub 2020 Dec 26. PMID: 33367987; PMCID: PMC7889554.
Alkali Supplementation:
For patients with Type 1 RTA, alkali supplementation is a cornerstone of treatment. This involves providing substances like sodium bicarbonate or sodium citrate to neutralize excess acid and restore normal bicarbonate concentration (22 to 24 mEq/L). This alkali therapy serves a dual purpose: it can prevent the formation of kidney stones and promote improved kidney function, ultimately mitigating the progression of kidney failure.
Electrolyte Replenishment:
In cases of Type 2 RTA, replacing lost electrolytes is paramount. Oral supplements or intravenous administration may be recommended to address deficiencies and maintain electrolyte equilibrium. In the case of infants with Type 1 RTA, potassium supplements may be necessary, although older children and adults typically don’t require them because alkali therapy inhibits the kidneys from expelling potassium into the urine.
Vitamin D Supplementation:
Adults with Proximal or Type 2 RTA need vitamin D supplementation to preserve bone health. Supplementary measures may include the administration of vitamin D (e.g., ergocalciferol at a daily oral dose of 800 IU) and oral calcium supplements (e.g., elemental calcium at a dosage of 500 mg orally three times a day, such as calcium carbonate at 1250 mg orally three times a day). These interventions help in preventing the skeletal deformities that can arise due to conditions like osteomalacia or rickets.12Renal Tubular Acidosis By L. Aime’e Hechanova, MD, Texas Tech University Health Sciences Center, El Paso Reviewed/Revised May 2022 | Modified Sep 2022 MSD Manual Professional Edition. (n.d.). Retrieved from https://www.msdmanuals.com/professional/genitourinary-disorders/renal-transport-abnormalities/renal-tubular-acidosis#:~:text=Type%202%20RTA%20is%20diagnosed,of%20bicarbonate%20is%20%3E%2015%25.”
Managing Hyperkalemia:
People with type 4 RTA may need other medicines to lower the potassium levels in their blood. Treating these conditions can alleviate RTA symptoms.
Fludrocortisone at a daily dose of 0.1 mg can effectively address hyperkalemia resulting from aldosterone deficiency. However, it is not commonly prescribed due to the risk of worsening hypertension, heart failure, and edema in individuals with renal insufficiency. In most cases, effective management can be achieved through dietary potassium restriction, typically limiting intake to 40 to 60 mEq per day, and, if required, the use of diuretics such as loop or thiazide diuretics.13Dobbin SJH, Petrie JR, Lean MEJ, McKay GA. Fludrocortisone therapy for persistent hyperkalemia. Diabet Med. 2017 Jul;34(7):1005-1008.
Managing Underlying Conditions:
Addressing the underlying causes of RTA is vital. Medical conditions such as autoimmune disorders or genetic predisposition might contribute to RTA, and treating these conditions can alleviate symptoms.
Lifestyle Adjustments for RTA Patients:
In addition to medical interventions, certain lifestyle changes can support RTA treatment:
- Hydration:
Staying adequately hydrated helps maintain kidney function and prevent electrolyte imbalances. - Diet Modifications:
Opting for a diet primarily consisting of plant-based foods like alkali-producing fruits and vegetables can prove to be effective in RTA management. It’s recommended to consult with a dietitian for personalized dietary guidance. - Medication Adjustments:
For individuals taking medications that exacerbate RTA, close monitoring and potential adjustments are essential to prevent further complications.
Conclusion
In conclusion, renal tubular acidosis is a complicated kidney ailment that could significantly affect acid-base stability. Understanding the types, causes, symptoms, and treatment processes is vital for handling this situation effectively and preventing long-term complications.
Refrences
- 1Laing, C. M., & Unwin, R. J. (2006). Renal tubular acidosis. Journal of Nephrology, 19, S46-52.
- 2Rajkumar P, Pluznick JL. Acid-base regulation in the renal proximal tubules: using novel pH sensors to maintain homeostasis. Am J Physiol Renal Physiol. 2018 Nov 1;315(5):F1187-F1190. doi: 10.1152/ajprenal.00185.2018. Epub 2018 Aug 1. PMID: 30066586; PMCID: PMC6293293.
- 3Karet, F. E. (2002). Inherited distal renal tubular acidosis. Journal of the American Society of Nephrology, 13(8), 2178-2184.
- 4Sebastian, A., McSherry, E., & Morris, R. C. (1971). On the mechanism of renal potassium wasting in renal tubular acidosis associated with the Fanconi syndrome (type 2 RTA). The Journal of Clinical Investigation, 50(1), 231-243.
- 5Kashoor I, Batlle D. Proximal renal tubular acidosis with and without Fanconi syndrome. Kidney Res Clin Pract. 2019 Sep 30;38(3):267-281. doi: 10.23876/j.krcp.19.056. PMID: 31474092; PMCID: PMC6727890.
- 6Montford JR, Linas S. How dangerous is hyperkalemia? Journal of the American Society of Nephrology. 2017;28:3155–3165. doi: 10.1681/ASN.2016121344
- 7Batlle, D., & Haque, S. K. (2012). Genetic causes and mechanisms of distal renal tubular acidosis. Nephrology Dialysis Transplantation, 27(10), 3691-3704.
- 8Harrington, T. M., Bunch, T. W., & Van Den Berg, C. J. (1983, June). Renal tubular acidosis. A new look at the treatment of musculoskeletal and renal disease. In Mayo Clinic Proceedings (Vol. 58, No. 6, pp. 354-360).
- 9Magni G, Unwin RJ, Moochhala SH. Renal tubular acidosis (RTA) and kidney stones: Diagnosis and management. Arch Esp Urol. 2021 Jan;74(1):123-128. English, Spanish. PMID: 33459628.
- 10Renal Tubular Acidosis By L. Aime’e Hechanova, MD, Texas Tech University Health Sciences Center, El Paso Reviewed/Revised May 2022 | Modified Sep 2022 MSD Manual Professional Edition. (n.d.). Retrieved from https://www.msdmanuals.com/professional/genitourinary-disorders/renal-transport-abnormalities/renal-tubular-acidosis#:~:text=Type%202%20RTA%20is%20diagnosed,of%20bicarbonate%20is%20%3E%2015%25.”
- 11Palmer BF, Kelepouris E, Clegg DJ. Renal Tubular Acidosis and Management Strategies: A Narrative Review. Adv Ther. 2021 Feb;38(2):949-968. doi: 10.1007/s12325-020-01587-5. Epub 2020 Dec 26. PMID: 33367987; PMCID: PMC7889554.
- 12Renal Tubular Acidosis By L. Aime’e Hechanova, MD, Texas Tech University Health Sciences Center, El Paso Reviewed/Revised May 2022 | Modified Sep 2022 MSD Manual Professional Edition. (n.d.). Retrieved from https://www.msdmanuals.com/professional/genitourinary-disorders/renal-transport-abnormalities/renal-tubular-acidosis#:~:text=Type%202%20RTA%20is%20diagnosed,of%20bicarbonate%20is%20%3E%2015%25.”
- 13Dobbin SJH, Petrie JR, Lean MEJ, McKay GA. Fludrocortisone therapy for persistent hyperkalemia. Diabet Med. 2017 Jul;34(7):1005-1008.