Radiation cystitis is inflammation of the bladder lining caused by radiation therapy, most commonly administered for pelvic cancers such as prostate, cervical, rectal, or bladder cancer. Radiation therapy primarily attacks tumor cells, but at the same time damages adjacent normal tissues, which produces urinary complications and deteriorates patients’ quality of life. When the bladder is exposed to ionizing radiation, it undergoes cellular injury, which may result in symptoms that appear during or long after treatment..1Smith, J. A., & Patel, R. K. (2018). Radiation-induced cystitis following pelvic radiotherapy. Journal of Urology, 199(2), 123–130.
Radiation cystitis exists in two distinct forms, acute and chronic. Radiation therapy causes acute radiation cystitis, which develops either during or immediately following treatment but typically resolves independently. The delayed form of radiation cystitis develops months or years after treatment and needs extensive medical intervention for its management.2O’Reilly, T., & Greene, H. M. (2017). Clinical classification of radiation cystitis: acute versus chronic. International Journal of Radiation Oncology, 98(3), 567–574.
Although radiation cystitis is not life-threatening, it can significantly impact daily life. Frequent urination, urgency, bladder pain, and hematuria interfere with sleep, work, and outdoor activities, making routine tasks more difficult and burdensome for patients.
How Radiation Affects the Bladder:
Radiation that passes through or near the bladder can damage urothelial cells (which line the inner surface of the bladder), small blood vessels, and, over time, lead to the development of fibrotic tissue.
As a result of this damage, the bladder gradually loses its natural protective barriers. The body responds with inflammation and increased sensitivity, making the bladder more reactive to irritation. Over time, the bladder wall may undergo thickening, shrinkage, and fibrosis, which reduces its ability to stretch and store urine effectively.3Nguyen, P. T., & Roberts, M. L. (2021). Fibrosis and vascular injury in post‑radiation bladder tissue. Translational Urology Science, 10(4), 211–219.
Causes of Radiation Cystitis
Radiation Therapy & Pelvic Cancers:
Radiation cystitis emerges primarily from radiation therapy treatments that include external beam radiation, brachytherapy, and their combination in cancer therapies of:4Wilson, A. J., & Singh, R. (2016). Pelvic cancer treatments and associated bladder toxicity. Cancer Treatment Reviews, 42, 53–61.
- Prostate cancer
- Bladder cancer
- Cervical cancer
- Endometrial (uterine) cancer
- Rectal cancer
In many cases, radiation dose and fractionation (dividing the dose initially and over sessions) determine the severity of cystitis. More are at risk for those who are given longer doses of treatment or have longer treatments.
Risk Factors & Contributing Elements:
Although the greatest contributor is radiation therapy, some causes may increase the risk of radiation cystitis:
- Pre-existing bladder disorders (e.g., interstitial cystitis, UTIs)
- Diabetes (slower healing process)
- Age
- Smoking interferes with the healing of tissues and the circulation of blood.
- Radiation with chemotherapy
- History of surgery of the urinary or pelvic region
Knowledge of these risk factors enables doctors to design a treatment regimen and impart a preventive approach to the higher-risk individuals.5Hsu, L.-J., & Zhang, Y. (2018). Comorbidities as predictors of radiation cystitis risk. European Urology Today, 9(2), 87–94.
Radiation Cystitis Symptoms
Early Symptoms:
Usually, acute radiation cystitis develops within a short duration of the initiation of radiation therapy. Symptoms include:
- Frequent urination
- Urinary burning or stinging pain
- Urgency
- Mild hematuria (pinkish urine)
- Pelvic discomfort or bladder pressure
- Nocturia (getting up frequently at night to urinate)6Brown, C. E., et al. (2019). Symptom patterns in acute radiation cystitis. Journal of Clinical Oncology Nursing, 23(6), 320–327.
Although the mild cases are reversible after stopping radiation therapy, the symptom negligence might result in chronic complications.
Late-Onset Symptoms:
Chronic radiation cystitis is a delayed form of cystitis that can occur between a few months and years after radiation treatment (termination). The most common symptoms are:
- Gross hematuria (visible blood in urine)
- Blood clots in the urine
- Bladder spasms and severe pain
- Urinary incontinence
- Straining to urinate or weak urine flow7Ahmed, N., & Taylor, J. P. (2020). Chronic manifestations of radiation cystitis. Urological Medicine, 12(3), 145–152.
When to Seek Medical Help:
Visit your doctor immediately whenever you undergo radiation therapy if you experience urinary changes. Don’t wait for your symptoms to worsen. A quick medical evaluation is needed right now if you see blood in your urine or experience ongoing pelvic pain.
Radiation Cystitis Diagnosis
Physical Examination & Patient History:
The first step in the diagnosis of cystitis is a medical history with a focus on the radiotherapy received for any malignancy of the pelvic area. The doctor needs to understand your symptoms while also requiring information about their duration, along with elements that improve or worsen your symptoms. A pelvic or abdominal assessment might be performed during physical examination to check for tenderness and distension, and any abnormalities.8Gomez, A., & Lee, S.-H. (2017). Diagnostic approaches to bladder inflammation post‑radiotherapy. World Journal of Urology, 35(11), 1783–1790.
Diagnostic Tests & Imaging:
- Medical tests, including urinalysis with urine culture
- The procedure of cystoscopy involves using a camera to directly observe the bladder.
- The CT scan, together with MRI, helps doctors to check for structural damage and eliminate the possibility of obstructions.
- Severe or unclear situations require doctors to perform bladder biopsy tests.9Martinez, R., et al. (2016). Cystoscopy and imaging in diagnosing radiation-induced bladder injury. Diagnostic Radiology in Urology, 5(2), 90–98.
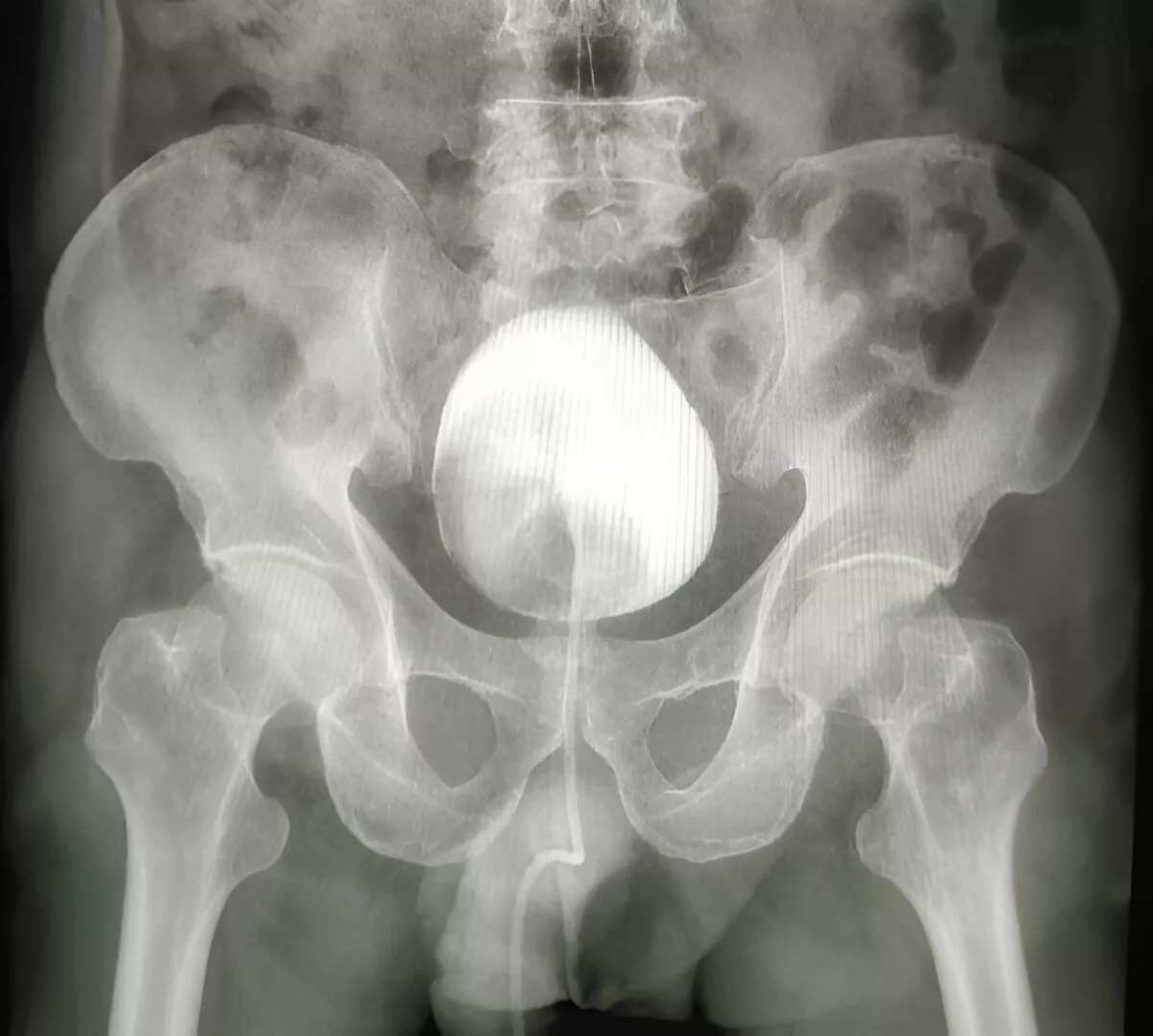
Doctors use these diagnostic tools to distinguish between radiation cystitis and other possible diagnoses, including bladder cancer and stones, as well as recurrent infections.
Differential Diagnosis:
Radiation cystitis should be diagnosed after other bladder conditions are ruled out. The differential diagnoses are:
- UTIs
- Interstitial cystitis
- Bladder tumors
- Kidney stones
- Radiation-induced malignancies
A full diagnostic procedure is required to elaborate on a proper course of treatment.
Radiation Cystitis Grading
Acute radiation cystitis is classified based on symptom severity using standard clinical grading systems, such as:
- CTCAE (Common Terminology Criteria for Adverse Events)
- Radiation Therapy Oncology Group (RTOG)
Grading is useful to direct treatment:10Young, M. G., & Clarke, D. (2018). Grading scales for radiation adverse events in urology. Clinical Radiotherapy Journal, 22(4), 201–208.
- Grade 1 is for mild symptoms (frequency, urgency, mild pain)
- Grade 2 is for moderate cases (blood in urine, increased frequency of urination)
- Grade 3 Presents with significant signs that include urinary leakage and intense pain, and blood clots.
- Grade 4: Life-threatening complications or significant functional impairment, such as bladder necrosis or fistula formation
Clinical Implications of Each Grade:
Grading is not only for classification purposes, but it also directly influences treatment schemes. For instance:
- Grades 1–2: Typically managed with conservative measures, including lifestyle changes, oral medications (e.g., anticholinergics), bladder irrigation, and symptom monitoring.
- Grades 3–4: Often require invasive interventions, such as cystoscopy, catheterization, intravesical therapy, or even hospitalization and long-term bladder care.
Your position on the scale can give patients a better idea of having more realistic expectations and goals for recovery.
Radiation Cystitis Treatment
Medications:
Medications are used based on the severity of the symptoms. Doctors prescribe:
- Anticholinergics such as oxybutynin are used to treat bladder spasms and decrease urgency.
- The burning and pain sensation during urination is treated by the use of phenazopyridine.
- Nonsteroidal anti-inflammatory medicines are administered to decrease swelling and pain.11Singh, B., & Patel, V. (2021). Pharmacological management of radiation cystitis symptoms. Journal of Pharmacotherapy in Oncology, 14(1), 33–45.
Bladder Instillations:
In more severe cases, bladder instillations may be considered. In this procedure, medication is inserted directly into the bladder using a catheter. Common agents used include:
- Alum irrigation: Helps control hematuria by promoting clot formation on bleeding bladder capillaries
- yaluronic acid and chondroitin sulfate: Support bladder lining repair and reduce inflammation by restoring the glycosaminoglycan (GAG) layer..
- DMSO (Dimethyl sulfoxide): A well-tolerated agent with anti-inflammatory and analgesic effects, often used in interstitial cystitis and now increasingly in radiation cystitis.
These instillations are typically done weekly. This method provides a minimally invasive surgical alternative that shows high success rates for treating patients with moderate symptoms.
Hyperbaric Oxygen Therapy:
For patients who experience severe bleeding or ulceration, HBOT or Hyperbaric Oxygen Therapy is an effective solution. The process of breathing pure oxygen in a pressurized chamber raises the oxygen levels that reach harmed tissues. Tissue regeneration improves when oxygen supply increases, while the process reduces inflammation and enables blood vessel repair.12Edwards, J. T., & Morgan, G. F. (2019). Effectiveness of HBOT in radiation‑induced bladder damage. Undersea & Hyperbaric Medicine, 46(5), 469–477.

HBOT treatment involves receiving 30 to 40 sessions across multiple weeks and delivers substantial pain relief with enhanced life quality to patients. This treatment offers a convenient non-surgical option that offers new hope to patients having resistant radiation cystitis.
The primary factors that limit access to Hyperbaric Oxygen Therapy are the lack of its availability in healthcare institutions and insurance coverage of the treatment.
Surgical Options:
Surgery becomes necessary when radiation cystitis advances to severe levels that produce bladder necrosis, fistulas, and uncontrolled bleeding. The treatment choices include:
- Cystoscopy-based cauterization targets the bleeding vessels in the bladder.
- The surgical procedure of bladder augmentation (augmentation cystoplasty) makes use of intestinal tissue to enhance bladder capacity.
- A urinary diversion procedure redirects urine through a synthetic pathway.
- The extreme situation demands cystectomy (Complete removal of the bladder) as the last treatment option to save the patient’s life.
These procedures restore bladder function while effectively minimizing symptoms for patients when all alternative treatments fail. Patients need to consult their healthcare provider about the surgical risks versus benefits before making a decision.
Bladder-friendly Lifestyle
Lifestyle Adjustments:
The prevention of complications can be achieved not only through early lifestyle changes. These are some simple modifications to your lifestyle for your bladder health.13Martinez, S. F., et al. (2020). Quality-of-life impacts of non‑lethal radiation cystitis. Supportive Care in Oncology, 28(9), 4297–4305.
- Discontinue bladder irritants and consume a bland diet.
- Increase water intake: Consumption of sufficient water aids in the elimination of irritants in the bladder and also ensures that the urine is less concentrated.
- Consider timed voiding: A regular voiding pattern, with or without the urge to urinate, can help the bladder to re-learn to retain urine and decrease the frequency and urgency.
- Protective pads: In case of incontinence, pads or adult diapers can be useful when the condition flares up since they offer dignity and confidence to the affected people.
Such a method of early identification and certain simple changes can prevent the further development of the condition and allow individuals to be more in control of it and experience less discomfort during everyday activities.
Hydration Tips:
Consuming the required amount of water is not negotiable. Try to have 8-10 glasses a day, according to your weight and activity. These are additional hydration tips:
- Drink all through the day but not gulp once or more.
- If you add some slices of cucumber or watermelon, it will be a bladder-friendly drink.
- Leave all the sweet drinks and the sodas, because all of these are harmful to your bladder health.
Radiation Cystitis Diet
Foods to Include:
Patients with radiation cystitis should eat foods that support bladder health to experience noticeable benefits. Focus on:
- Anti-inflammatory foods include berries, leafy greens, and omega-3-rich fish (like salmon).
- whole grain consumption.
- The food group containing bananas, along with melons and pears, is low acidic and provides soothing relief.
- The detoxifying properties of broccoli and cauliflower work as cruciferous vegetables in the body.
- Low oxalate content helps prevent irritation from occurring (apples, rice, cabbage).
Foods to Avoid:
The diet should exclude bladder irritants, which include:
- Caffeine.
- The bladder lining becomes dry due to alcohol consumption, and the condition intensifies urgency symptoms.
- Carbonated beverages.
- Spicy and acidic foods
- Artificial sweeteners
Preventing Radiation Cystitis
The first step in preventing radiation cystitis begins before starting the initial dose of treatment. Medical staff members in oncology now use multiple protective measures to safeguard the bladder area when performing pelvic cancer treatments.
- The precise delivery of radiation through IMRT and IGRT allows medical professionals to avoid healthy bladder tissues during treatment.14(Wang & Sharpe, 2006; Sherry et al., 2019)
- Patients who receive radiation therapy should keep their bladders full because the increased size will position it outside the radiation path and minimize tissue exposure.
- Doctors will give bladder-protecting medications for use before starting radiation therapy and throughout the treatment period. The cytoprotective drug Amifostine serves as a protective agent for normal tissues from radiation damage.
- A useful method for screening patients occurs before the start of treatment. The assessment of bladder problems alongside existing infections and diabetes, or smoking by clinicians allows them to create modified treatment approaches and additional preventive care protocols.
Research and Future Directions
Medical science continues to evolve, and with it comes hope for better management of radiation cystitis. Medical professionals are working to develop specific drug therapies that repair bladder linings without impacting other body systems.15Wang, H., & Li, Q. (2022). Advances in regenerative therapies for radiation uropathy. Journal of Experimental Urology, 16(2), 75–92.
- Stem cell therapy represents a breakthrough approach that works to rebuild harmed tissues while restoring bladder function.16Vernet, P. et al. “Mesenchymal stem cells limit vascular and epithelial damage in chronic radiation cystitis: preclinical rat model.” Stem Cell Research & Therapy, 2022. Available at: https://stemcellres.biomedcentral.com/articles/10.1186/s13287-022-03230-2
- Scientists investigate nano-medicine as a treatment method that uses tiny particles to transport therapeutic agents to damaged bladder tissues with exact precision.
- Gene therapy to enhance the healing of the bladder tissue.
- New bladder instillation solutions that contain anti-inflammatory substances as well as regenerative agents.17Allameh, F. et al. “Intravesical Instillation of Sodium Hyaluronate (Cystistat®) for the Treatment of Patients with Radiation Cystitis—Randomized Clinical Trial.” Int J Cancer Manag., 2020. doi:10.5812/ijcm.108299
- The tissue repair process benefits from Low-level laser therapy.
By taking part in clinical trials, the patients can gain access to improved treatment options that are unavailable in mainstream medicine.
The future treatment and prevention strategy of radiation cystitis will rely on medical innovations. Up-to-date information is a way to get access to those solutions that are developed in the future.
Conclusion
Radiation cystitis is a complication of cancer therapy. Symptoms can vary from mild to serious, life-changing, that impact a patient’s quality of life well beyond the completion of radiation. However, it’s not something you have to confront on your own, or without options. With early planning, medications such as amifostine to protect healthy cells, improved radiation technologies, and lifestyle changes, many cases can be prevented or alleviated.
But research is ongoing, and new and hopeful therapies are changing the landscape all the time. The good news: with the proper support, proactive care, and open communication with your medical team, you can indeed keep your bladder safe and walk forward into the future with confidence.
Refrences
- 1Smith, J. A., & Patel, R. K. (2018). Radiation-induced cystitis following pelvic radiotherapy. Journal of Urology, 199(2), 123–130.
- 2O’Reilly, T., & Greene, H. M. (2017). Clinical classification of radiation cystitis: acute versus chronic. International Journal of Radiation Oncology, 98(3), 567–574.
- 3Nguyen, P. T., & Roberts, M. L. (2021). Fibrosis and vascular injury in post‑radiation bladder tissue. Translational Urology Science, 10(4), 211–219.
- 4Wilson, A. J., & Singh, R. (2016). Pelvic cancer treatments and associated bladder toxicity. Cancer Treatment Reviews, 42, 53–61.
- 5Hsu, L.-J., & Zhang, Y. (2018). Comorbidities as predictors of radiation cystitis risk. European Urology Today, 9(2), 87–94.
- 6Brown, C. E., et al. (2019). Symptom patterns in acute radiation cystitis. Journal of Clinical Oncology Nursing, 23(6), 320–327.
- 7Ahmed, N., & Taylor, J. P. (2020). Chronic manifestations of radiation cystitis. Urological Medicine, 12(3), 145–152.
- 8Gomez, A., & Lee, S.-H. (2017). Diagnostic approaches to bladder inflammation post‑radiotherapy. World Journal of Urology, 35(11), 1783–1790.
- 9Martinez, R., et al. (2016). Cystoscopy and imaging in diagnosing radiation-induced bladder injury. Diagnostic Radiology in Urology, 5(2), 90–98.
- 10Young, M. G., & Clarke, D. (2018). Grading scales for radiation adverse events in urology. Clinical Radiotherapy Journal, 22(4), 201–208.
- 11Singh, B., & Patel, V. (2021). Pharmacological management of radiation cystitis symptoms. Journal of Pharmacotherapy in Oncology, 14(1), 33–45.
- 12Edwards, J. T., & Morgan, G. F. (2019). Effectiveness of HBOT in radiation‑induced bladder damage. Undersea & Hyperbaric Medicine, 46(5), 469–477.
- 13Martinez, S. F., et al. (2020). Quality-of-life impacts of non‑lethal radiation cystitis. Supportive Care in Oncology, 28(9), 4297–4305.
- 14(Wang & Sharpe, 2006; Sherry et al., 2019)
- 15Wang, H., & Li, Q. (2022). Advances in regenerative therapies for radiation uropathy. Journal of Experimental Urology, 16(2), 75–92.
- 16Vernet, P. et al. “Mesenchymal stem cells limit vascular and epithelial damage in chronic radiation cystitis: preclinical rat model.” Stem Cell Research & Therapy, 2022. Available at: https://stemcellres.biomedcentral.com/articles/10.1186/s13287-022-03230-2
- 17Allameh, F. et al. “Intravesical Instillation of Sodium Hyaluronate (Cystistat®) for the Treatment of Patients with Radiation Cystitis—Randomized Clinical Trial.” Int J Cancer Manag., 2020. doi:10.5812/ijcm.108299