What is Bilateral Tubal Ligation?
Bilateral tubal ligation, also known as ‘female sterilization’ or ‘getting your tubes tied,’ is a method of permanent contraception. This procedure involves blocking or sealing both fallopian tubes to prevent eggs from meeting sperm, thereby eliminating the possibility of fertilization and pregnancy. It is one of the most widely used forms of birth control globally, with approximately 220 million couples relying on it.1American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Gynecology (2019). ACOG Practice Bulletin No. 208: Benefits and Risks of Sterilization. Obstetrics and Gynecology, 133(3), e194–e207. https://doi.org/10.1097/AOG.0000000000003111
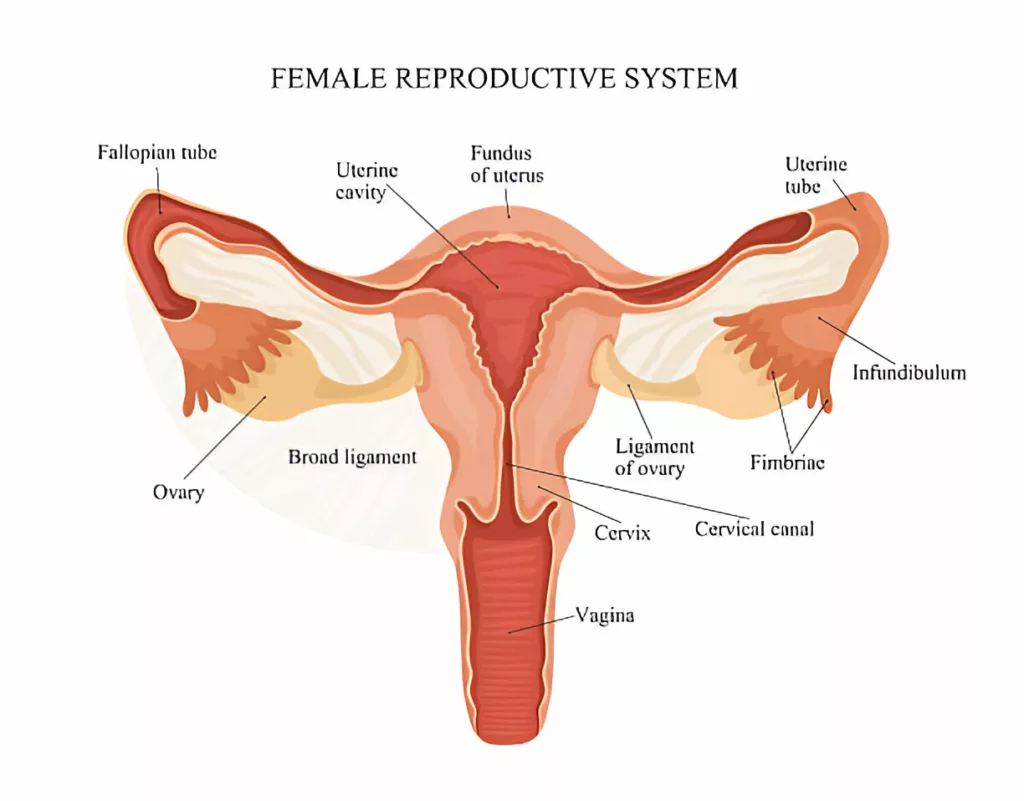
Anatomy & Physiology of the Female Reproductive System
The female reproductive system consists of external and internal genitalia.
The labia, clitoris, urethral and vaginal openings make up the external genitalia. The external genitalia allows the sperm to reach the internal part of the female reproductive system.
The vagina, cervix, uterus, a pair of fallopian tubes, and a pair of ovaries constitute the internal genitalia.
The vagina leads to the cervix, which opens into the lowest part of the uterus. The uterus has two ovaries on either of its sides and two fallopian tubes arising from its superior aspect.
In a normal reproductive cycle, what happens is that the ovaries release eggs, in the process termed ovulation, once every month. The fallopian tubes take up these eggs via their fimbria (finger-like projections at the terminal portions of fallopian tubes). The sperms that enter the internal genitalia travel up through the uterus to the fallopian tubes and fertilize these eggs, producing an embryo that then implants inside the uterus.
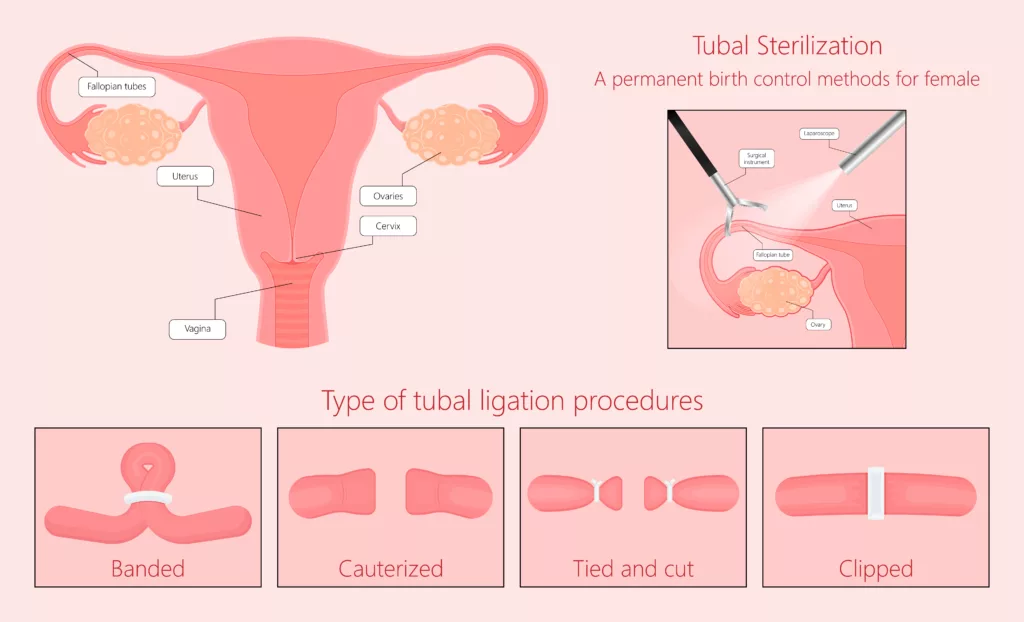
How does Bilateral Tubal Ligation work?
In bilateral tubal ligation, both of the fallopian tubes are occluded using special threads, clips, bands, or an electric current. This obstructs the passage of sperm through the fallopian tubes to mate with the egg, preventing fertilization and offering couples peace of mind regarding pregnancy.
From 2006-2010, almost half of the married couples in the US chose tubal ligation for permanent contraception. It is 99% effective in preventing pregnancy. Apart from its contraceptive benefit, it also has an established role in preventing ovarian cancer, when coupled with salpingectomy.2ACOG Committee Opinion No. 774: Opportunistic Salpingectomy as a Strategy for Epithelial Ovarian Cancer Prevention. (2019). Obstetrics and Gynecology, 133(4), e279–e284. https://doi.org/10.1097/AOG.0000000000003164
Who is an Ideal Candidate?
Indications for bilateral tubal ligation include:
- A desire for permanent birth control
- Having completed child-bearing
- Having contraindications to other methods of contraception
- Having a high risk of ovarian cancer, such as carrying a mutated BRCA gene3Practice Bulletin No 182: Hereditary Breast and Ovarian Cancer Syndrome. (2017). Obstetrics and Gynecology, 130(3), e110–e126. https://doi.org/10.1097/AOG.0000000000002296
Contraindications for Bilateral Tubal Ligation
The absolute contraindication to bilateral tubal ligation is the desire to have children in the future. It’s because even though procedures to reverse tubal ligation exist, they might be out of option for many, owing to their higher costs and comparatively lower success rates.
Relative contraindications include conditions like:
- Uncontrolled diabetes, hypertension, and other medical co-morbidities.
- Obesity
- Adhesive diseases, such as those resulting from previous pelvic or abdominal surgeries, can increase the risk of complications.
- Active pelvic infection
- Any other condition that renders one unfit for undergoing any surgery or anesthesia
Before going for Bilateral Tubal Ligation
Almost a quarter of the women getting tubal ligation express regret later on in life.4Shreffler KM, Greil AL, McQuillan J, Gallus KL. Reasons for tubal sterilization, regret, and depressive symptoms. J Reprod Infant Psychol. 2016;34(3):304-313. doi: 10.1080/02646838.2016.1169397. Epub 2016 May 13. PMID: 28133405; PMCID: PMC5267553 Therefore, weigh all the pros and cons before you make this decision. You need to give it a second thought if you are:
- Young: less than 30 years of age5Danvers, A. A., & Evans, T. A. (2022). Risk of Sterilization Regret and Age: An Analysis of the National Survey of Family Growth, 2015-2019. Obstetrics and Gynecology, 139(3), 433–439. https://doi.org/10.1097/AOG.0000000000004692
- Unmarried
- Uncertain regarding irreversible contraception
- Under pressure from your partner or any other family member
- Haven’t acquired sufficient information about the procedure and alternative options
If you are a healthcare professional, know that counseling your patients adequately is of utmost significance in preventing post-sterilization regret.
- Make sure your patient understands that this procedure is permanent and irreversible – they won’t be able to have children ever again.
- Discuss with your patient their contraceptive needs, maybe they don’t need permanent birth control at all, they are just seeking long-acting reversible contraception.
- Offer alternative methods like IUCDs(Intra-uterine contraceptive devices) and hormonal implants.
- In case your patient’s reproductive need can only be met by tubal ligation, tell them everything about the procedure: its types, associated risks, complications, recovery, and of course, the costs.
Types of Bilateral Tubal Ligation
Bilateral tubal ligation can be categorized into two main approaches:
- Postpartum Tubal Ligation: Performed during or immediately following childbirth, typically after a cesarean section or within 24–48 hours after vaginal delivery.
- Interval Tubal Ligation: Planned and performed at any time unrelated to childbirth or pregnancy, often using laparoscopic techniques.
Depending upon how it is performed, the following are some of the popular types of bilateral tubal ligation:
Bipolar Coagulation:
This is a popular type of tubal ligation that is performed using laparoscopy. In bipolar coagulation, the surgeon holds the fallopian tube between the paddles of a cautery instrument. He then applies an electric current to desiccate and seal the tube (the process is referred to as electrocauterization)
Pomeroy Tubal Ligation:
It is carried out soon after childbirth. The surgeon sutures the tube so that it forms a loop. He then cuts this loop and burns the exposed ends using an electric current.
Fimbriectomy:
It involves excising the terminal portion of fallopian tubes that have the fimbria or the finger-like projections, that catch the eggs.
Irving Procedure:
The surgeon ties the fallopian tube at two points and then resects the segment in between.
Hulka or Filshie Clip Tubal Ligation:
The surgeon clips the fallopian tubes using a Hulka or Filshie clip.
Fallope Ring or Rubber Band Tubal Ligation:
A silastic ring or small rubber band is applied to looped segments of the fallopian tube, blocking the lumen and preventing fertilization.
Essure & Adiana:
These hysteroscopic methods, no longer widely available due to safety concerns, involved placing devices (metal or fiber coils in Essure and silicon inserts in Adiana) into the fallopian tubes to induce scarring and block the tubes.
Bilateral Tubal Ligation: The Whole Process
Booking the Surgery:
After signing the consent form and completing the required documentation, your gynecologist will advise you on some lab tests and check for your anesthesia fitness.
If you are on anti-coagulant or anti-platelet medications, the doctor will ask you to discontinue them temporarily. The doctor will advise you to quit smoking as well.
On the day of Surgery:
As with any other surgery, arrive at the hospital in a state of overnight fasting. After that, you will probably go through a sensitive pregnancy test to make sure you are not pregnant.
Bilateral Tubal Ligation Procedure:
The procedure of tubal ligation is performed under general or spinal anesthesia. Depending upon your preferences and circumstances, the surgeon will choose any of the following techniques:
Laparoscopy
Laparoscopic tubal ligation is one of the most popular techniques for sterilization nowadays, with a success rate of up to 99%.6Gariepy, A. M., Creinin, M. D., Schwarz, E. B., & Smith, K. J. (2011, August). Reliability of Laparoscopic Compared With Hysteroscopic Sterilization at 1 Year. Obstetrics & Gynecology, 118(2), 273–279. https://doi.org/10.1097/aog.0b013e318224d4d2 It’s a minimally invasive surgery in which the surgeon operates through small incisions without opening any of the patient’s body cavities.
The advantages of laparoscopy include speedy recovery, small incisions, and better visibility of the pelvic and abdominal organs.
Laparotomy
Laparotomy is a conventional technique which is a lot more intensive than laparoscopy. In laparotomy, the surgeon opens your abdominal cavity through a 2-5 inches long incision. He then identifies the uterus, traces the fallopian tubes, and ligates them using any of the means mentioned earlier.
Owing to its longer recovery, risks from a bigger incision, and availability of modern and safer alternatives, this technique is not much used these days. Surgeons prefer it only when the patient delivers via a C-section, i.e., the surgeon performs sterilization through the same incision he gives to deliver the baby, saving the patient time, cost, and the physiological stress of having gone under the knife another time.
Mini-Laparotomy
A mini-laparotomy involves a relatively smaller incision. It is performed under a spinal or epidural anesthesia.
This technique is lower-risk than a laparotomy and is usually performed in the first 48 hours after a vaginal delivery.
Hysteroscopy
A hysteroscopy is a non-surgical, minimally invasive technique, being used as an alternative to laparoscopy.
In hysteroscopy, the gynecologist uses a hysteroscope to visualize the tubes through the vaginal route. Then, the gynecologist places micro-inserts or coils inside that cause inflammation and closes off the fallopian tubes over a few months. By the time sterilization is achieved, the patient is instructed to keep using other methods of contraception.
Hysteroscopy can easily be performed in an outpatient setting, without general or spinal anesthesia. In addition to providing a quicker recovery, this technique is safer, more convenient, suitable, and cost-effective compared to laparoscopy.7Ouzounelli, M., & Reaven, N. L. (2015, March). Essure Hysteroscopic Sterilization Versus Interval Laparoscopic Bilateral Tubal Ligation: A Comparative Effectiveness Review. Journal of Minimally Invasive Gynecology, 22(3), 342–352. https://doi.org/10.1016/j.jmig.2014.12.002
After the Procedure:
After your tubal ligation, the doctor will either allow you to go home within a few hours or ask you to stay in the hospital overnight, depending upon the technique used and your previous health status. Before you leave for home, your doctor will advise you to take care of a few things:
- Avoid lifting heavy objects for the next few weeks.
- Avoid engaging in intercourse, to avoid discomfort.
- Keep the incision site dry. Take special precautions while taking a shower.
- It’s okay to experience vaginal bleeding for up to one month after the surgery. You might also experience painful or heavier periods once your normal cycle resumes.
- Use painkillers to manage pain, tenderness, and discomfort.
- You might experience shoulder pain due to the gas filled in your abdomen during laparoscopy. You can relieve this pain by applying warm compressors, taking a hot shower, or a light walk.
Side-effects of Bilateral Tubal Ligation
Some of the side effects of BTL include:
- Regret
- Failure
- Ectopic pregnancy: In case of failure and pregnancy, it is more likely for the patient to have an ectopic pregnancy, i.e., the embryo implants somewhere outside the uterus. This type of pregnancy is a health hazard: it may cause the tubes to rupture resulting in life-threatening bleeding.
- Risks related to the surgical technique/anesthesia used
- Susceptibility to Sexually Transmitted Infections(STDs): BTL does not protect against STDs like HIV. So, despite having your tubes tied, you will still have to use barrier methods. While some older studies suggest that BTL may offer protection against pelvic inflammatory disease (PID), more recent evidence contradicts this notion.8Abbuhl, S. B., Muskin, E. B., & Shofer, F. S. (1997). Pelvic inflammatory disease in patients with bilateral tubal ligation. The American journal of emergency medicine, 15(3), 271–274. https://doi.org/10.1016/s0735-6757(97)90012-7
Recovery after Bilateral Tubal Ligation
The recovery after bilateral tubal ligation depends upon the patient’s age, co-morbidities, the type of surgery performed, the standard of care provided, and compliance of the patient to the doctor’s advice.
You will recover a lot quicker from laparoscopic and hysteroscopic procedures, where you return to your normal routine within days, as compared to a laparotomy or a mini-lap, where healing takes weeks to complete.
Similarly, if you have had a puerperal or a postpartum BTL, then your recovery period will extend up to six or more weeks, as you will also be healing from birth.
Moreover, poor provision of care or adherence to medical advice lands the patient in complications, prolonging the usual course of recovery.
Make sure you follow your doctor’s guidelines and attend your follow-up appointments.
Importantly, if you experience any of these, seek medical assistance immediately:
- Fever above 100 degrees Fahrenheit, that persists for more than 24 hours.
- Nausea and vomiting that don’t go away within a day.
- Heavy vaginal bleeding
- Any swelling, discharge, redness, or bleeding from the incision. These signs are usually indicative of a surgical site infection.
- Signs of pregnancy, including those of an ectopic pregnancy, e.g., amenorrhea (missing your period), pain in the bottom right or left corner of your abdomen, pelvic pain, vaginal bleeding outside of periods, lightheadedness, nausea, vomiting, etc.
Bilateral Salpingectomy Vs. Tubal Ligation
Another method of permanent birth control is bilateral salpingectomy. In salpingectomy, both the fallopian tubes are removed either partially or completely. It is similar to tubal ligation in many terms, except that, a salpingectomy cannot be reversed at all while a ligation can be.
As the idea of salpingectomy being protective against ovarian cancer is gaining popularity, more people are now opting for it to achieve permanent birth control.9Hicks-Courant, K. D. (2016, November). Growth in salpingectomy rates in the United States since 2000. American Journal of Obstetrics and Gynecology, 215(5), 666–667. https://doi.org/10.1016/j.ajog.2016.07.055 However, due to its potential to induce early menopause and subsequent hormonal imbalances, health authorities recommend it primarily for high-risk groups rather than the general population.
Bilateral Tubal Ligation Reversal
Although tubal ligation is meant to be permanent, options are available for its reversal. The success rates of these procedures vary from 40-85% depending upon several factors such as:
- Age of the patient
- Type of tubal ligation done
- Length of functional fallopian tubes
- Scar tissue in the pelvis
- The skill of the operating surgeon
While pregnancy is possible after undergoing a reversal surgery, the associated costs remain a limiting factor for many. The surgery alone costs several thousand dollars, which mostly doesn’t fall under insurance coverage.
Take-Home Message
Bilateral tubal ligation is a safe and effective procedure for life-long birth control, which also reduces the risk of gynecological cancers. Modern healthcare offers multiple techniques and types of procedures to ligate the tubes. As reversal surgeries are not for everyone, one must consider all the pros and cons before opting for them.
Refrences
- 1American College of Obstetricians and Gynecologists’ Committee on Practice Bulletins—Gynecology (2019). ACOG Practice Bulletin No. 208: Benefits and Risks of Sterilization. Obstetrics and Gynecology, 133(3), e194–e207. https://doi.org/10.1097/AOG.0000000000003111
- 2ACOG Committee Opinion No. 774: Opportunistic Salpingectomy as a Strategy for Epithelial Ovarian Cancer Prevention. (2019). Obstetrics and Gynecology, 133(4), e279–e284. https://doi.org/10.1097/AOG.0000000000003164
- 3Practice Bulletin No 182: Hereditary Breast and Ovarian Cancer Syndrome. (2017). Obstetrics and Gynecology, 130(3), e110–e126. https://doi.org/10.1097/AOG.0000000000002296
- 4Shreffler KM, Greil AL, McQuillan J, Gallus KL. Reasons for tubal sterilization, regret, and depressive symptoms. J Reprod Infant Psychol. 2016;34(3):304-313. doi: 10.1080/02646838.2016.1169397. Epub 2016 May 13. PMID: 28133405; PMCID: PMC5267553
- 5Danvers, A. A., & Evans, T. A. (2022). Risk of Sterilization Regret and Age: An Analysis of the National Survey of Family Growth, 2015-2019. Obstetrics and Gynecology, 139(3), 433–439. https://doi.org/10.1097/AOG.0000000000004692
- 6Gariepy, A. M., Creinin, M. D., Schwarz, E. B., & Smith, K. J. (2011, August). Reliability of Laparoscopic Compared With Hysteroscopic Sterilization at 1 Year. Obstetrics & Gynecology, 118(2), 273–279. https://doi.org/10.1097/aog.0b013e318224d4d2
- 7Ouzounelli, M., & Reaven, N. L. (2015, March). Essure Hysteroscopic Sterilization Versus Interval Laparoscopic Bilateral Tubal Ligation: A Comparative Effectiveness Review. Journal of Minimally Invasive Gynecology, 22(3), 342–352. https://doi.org/10.1016/j.jmig.2014.12.002
- 8Abbuhl, S. B., Muskin, E. B., & Shofer, F. S. (1997). Pelvic inflammatory disease in patients with bilateral tubal ligation. The American journal of emergency medicine, 15(3), 271–274. https://doi.org/10.1016/s0735-6757(97)90012-7
- 9Hicks-Courant, K. D. (2016, November). Growth in salpingectomy rates in the United States since 2000. American Journal of Obstetrics and Gynecology, 215(5), 666–667. https://doi.org/10.1016/j.ajog.2016.07.055





