Brachytherapy is a special type of radiation therapy. It provides radiation to internal organs of the body through an internal device (radioactive source) placed in close proximity to the tumor. It is used to treat a variety of cancers.
What is Brachytherapy?
Brachytherapy refers to radiation therapy in which radioactive isotopes are placed in implants, which are then placed directly inside your body. These implants can include:
- Pellets
- Seeds
- Ribbons
- Wires
- Needles
- Capsules
These implants are positioned immediately into, next to, or near a tumor. They may remain placed for minutes, hours, or days.1Brachytherapy for Cancer. (2019, January 29). Cancer.gov. https://www.cancer.gov/about-cancer/treatment/types/radiation-therapy/brachytherapy
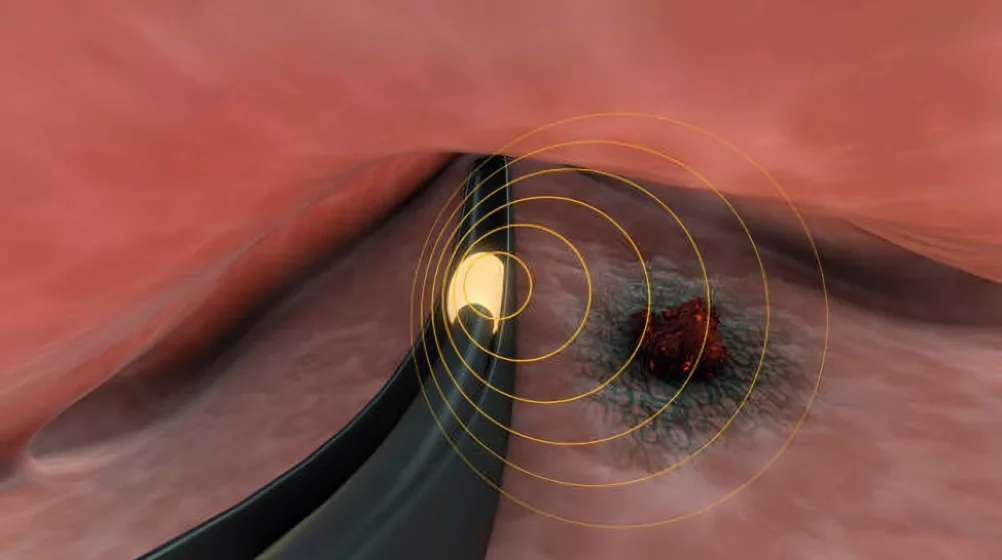
Principle of Brachytherapy
The principle of this therapy lies in delivering as high radiation doses as possible, as close to the tumor tissue as possible, without harming your normal nearby cells. This is ensured by first placing the radiation source inside your body instead of delivering it externally so that radiation will only target the tumor and not normal tissues.
In addition, sources are designed to make sure that their radiation dose greatly reduces as their distance from the source increases. Therefore, any potential damage to normal cells gets further minimized.
Types of Brachytherapy:
Depending on the location where brachytherapy implants are placed and the timing of radiation, this therapy can be divided into numerous types. Examples of these types include:
Interstitial Brachytherapy
Interstitial brachytherapy is called so because the implant is inserted into a space inside the tumor tissue itself — this space is referred to as the interstitium.
Intracavity Brachytherapy
In intracavity brachytherapy, brachytherapy implants are placed within the cavities of hollow organs in your body.
Episcleral Brachytherapy
During sessions of episcleral brachytherapy, brachytherapy implants are directly attached to the scleral portion of the eye. It is used to treat cancers of the eye.
Low Dose Rate Brachytherapy
In low-dose-rate brachytherapy, small amounts of radiation are delivered over days or weeks instead of one short session.
High Dose Rate Brachytherapy
High-dose radiation brachytherapy delivers a high dose of radiation to tumors on a temporary basis. Doctors use thin tubes or balloon catheters to administer this radiation. Since it is only inside your body for a short period of time, it causes much less damage to healthy organs than external radiation.
Permanent Brachytherapy
In permanent brachytherapy, numerous metal implants are placed inside a body organ to treat localized cancers. Their radiation dose reduces over time to match disease regression and avoid overexposure. These are usually used for prostate cancer. As the name suggests, they are placed for life and cannot be taken out.2Brachytherapy. (2024, October). Hopkinsmedicine.org. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/brachytherapy
What Isotopes are used in Brachytherapy?
Radioactive isotopes are substances that have radioactivity, i.e., they are known to emit waves of radiation. They are vital for the treatment of various cancers and other proliferative disorders. This therapy involves the use of radioactive isotopes inserted into implants, which are placed inside your body’s cancerous organs. This way, the radiation emitted by these isotopes gets directly absorbed by cancer cells, resulting in their destruction. Examples of radioactive isotopes used in this therapy are:3Strohmaier, S., & Grzegorz Zwierzchowski. (2011). Comparison of 60 Co and 192 Ir sources in HDR brachytherapy. Journal of Contemporary Brachytherapy, 4, 199–208. https://doi.org/10.5114/jcb.2011.26471
| Isotope | Type of brachytherapy | Half-Life |
| Iodine-125 | Low-dose radiation brachytherapy | 60 days |
| Palladium-103 | Low-dose radiation brachytherapy | 17 days |
| Cesium-131 | Low-dose radiation brachytherapy | 9.7 days |
| Iridium-192 | Low-dose radiation brachytherapy | 74 days |
| Strontium-90 | High-dose radiation brachytherapy | 29.1 years |
Advantages & Disadvantages of Brachytherapy
This therapy is different from traditional radiotherapy, which positions it as a unique cancer treatment. This gives it advantages as well as disadvantages:
| Advantages | Disadvantages |
| Brachytherapy delivers radiation directly to tumors. This makes it a more effective treatment for localized tumors than external radiation. | As it is a localized treatment, brachytherapy is not suitable for widespread tumors. It is also unsuitable for large, diffuse, and metastatic tumors. |
| Brachytherapy treatment regimens are often shorter than external radiation therapy, as a higher dose of radiation gets absorbed by tumors in a much shorter duration of time. | Implantation of radioactive material can pose some surgical risks and discomfort |
| During brachytherapy, normal tissues come into much less contact with radiation than tumor tissues. This greatly reduces the side effects and discomfort caused by radiation itself. | Patients with implants could need to avoid contact with pregnant and young people to avoid accidental exposure to radiation. |
| Brachytherapy poses much fewer occupational hazards to medical professionals than traditional radiation. | Brachytherapy requires thorough planning and specialized expertise. It requires a highly trained team of brachytherapists, as well as technologically advanced equipment to carry out the procedure. |
Indications of Brachytherapy
This is a type of radiation treatment that is indicated for many kinds of cancers. It works best for tumors that need localized and targeted therapy, where external radiation can harm the healthy tissue nearby. With new technology, doctors are finding more ways to use it in cancer management, such as palliative care, to improve the quality of life of even terminal cancer patients. Some of the indications are:
Gynecological Cancers
The female pelvis has an extremely confined anatomy, where a variety of cancers can occur, such as:
- Cervical cancer
- Endometrial cancer
- Uterine cancer
- Vaginal cancer
This therapy is much more effective in treating these cancers and for boosting tumor control in comparison with external radiation.
Both high and low-dose radiation therapy can be used — isotopes employed for these include Iridium-192 and Cesium-137, respectively.
Prostate Cancer
Permanent seed implantation is often used for treating prostate cancer. This implantation of radioactive seeds allows for the continuous delivery of radiation into the prostate gland. It also spares surrounding structures such as the bladder and rectum from widespread radiation exposure and side effects. The isotopes used for this purpose are often Iodine-125, Palladium-103, and Iridium-192.
Breast Cancer
Breast cancer is of many types and comes in many grades. This therapy is used during the various stages of breast cancer treatment. Early-stage breast cancer, post-lumpectomy as partial breast irradiation.
It is an excellent treatment modality for early-stage breast cancer. It is particularly used for patients with low-risk, localized tumors.
Head & Neck Cancers
This therapy is especially helpful in treating cancers of the head and neck region — this region hosts delicate structures, such as:
- Salivary glands
- Tongue
- Throat
- Larynx
All of these structures are sensitive and can easily get damaged by external radiation. It also preserves functions like speaking, swallowing, and saliva production. This helps maintain the patient’s quality of life during and after treatment.
Eye Cancer
The eye consists of several sensitive structures, such as the retina and the optic nerve. These structures require special measures for conservation. Episcleral brachytherapy places radioactive plaques directly on the eye. This way, only eye tumors are exposed to high radiation, such as:
- Retinoblastoma
- Uveal melanoma
- Intraocular lymphoma
- Conjunctival melanoma
- Choroidal nevus
- Iris melanoma
- Retinal angiomas
- Squamous cell carcinoma of the conjunctiva
- Medulloepithelioma
- Basal cell carcinoma of the eyelid
The radioactive isotopes used in episcleral brachytherapy are used for Iodine-125 and Ruthenium-106.
Skin Cancers
The skin is another sensitive organ that can easily get damaged by widespread external radiation. This therapy is applied to the skin surface and implanted near the lesion. It offers a non-invasive treatment option for skin lesions that are unsuitable for surgery. Examples include:
- Basal cell carcinoma
- Squamous cell carcinoma
- Merkel cell carcinoma
- Kaposi’s sarcoma
- Melanoma
Isotopes like Strontium-90 and Iridium-192 are often used for skin cancer.
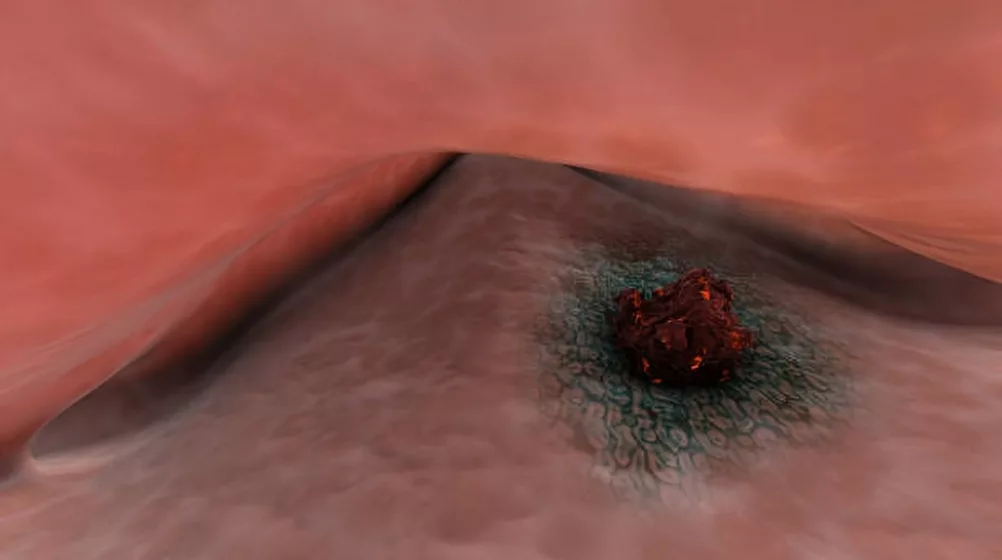
Gastrointestinal Cancers
It is also used to treat gastrointestinal cancers of different kinds:
- Esophageal cancer
- Rectal cancer
- Anal cancer
Abdominal organs are closely knit anatomically, so they minimize exposure to surrounding tissues. For esophageal cancer, implants are positioned inside the esophagus using an endoscope or catheter. This is usually done as palliative care to relieve symptoms such as difficulty swallowing. Sometimes, it is also used for localized or recurrent tumors. For anal and facial cancers, brachytherapy is delivered via a rectal applicator placed close to the tumor.
In addition, contact X-ray brachytherapy is a specially devised brachytherapy used for small tumors of the rectum that are less than 3 cm in size, and are only confined to the rectal area.4Clinic, C. (2023, August 25). Brachytherapy, or internal radiation therapy, treats prostate, breast, head and neck, and other cancers. It’s an effective treatment for tumors that haven’t spread. Cleveland Clinic. https://my.clevelandclinic.org/health/treatments/16500-brachytherapy
What makes you a good candidate for Brachytherapy?
There are several factors that determine if you are a good candidate for this therapy or not. You might be a good candidate in the case:
- The kind of cancer you have is localized to a specific region of your body, such as gynecological and prostate cancers confined to the abdomen and/or pelvis.
- You are already undergoing chemotherapy or external beam radiotherapy and could benefit from a complementary treatment.
- Your personal preferences include a treatment that does not cause generalized side effects of radiation therapy.
- If the kind of cancer you have requires preservation of functionality, such as normal functioning of the bowel, bladder, or sexual organs. 5Park, D. S. (2012). Current Status of Brachytherapy for Prostate Cancer. Korean Journal of Urology, 53(11), 743–743. https://doi.org/10.4111/kju.2012.53.11.743
Contraindications of Brachytherapy
It is an effective treatment for cancer, but it is not advisable in numerous cases. Examples of such contraindications include:
- Having an expected life expectancy of less than five years, even with treatment
- Pregnancy due to potential harm to the developing fetus
- Being unfit for anesthesia
- Active infections near or in the treatment area can lead to sepsis
- Uncontrolled bleeding disorders and anticoagulant therapy can cause hemorrhage during or after the procedure
- Tumors located near vital organs like the spinal cord or major blood vessels may cause severe damage. Severe skin disorders near the treatment site pose risks for implants applied to the skin.
Steps of Brachytherapy Procedure
The steps can vary depending on the type of brachytherapy you choose to undergo. Steps common to most brachytherapy procedures include:
- Your doctor will ask you to stop eating and drinking four to six hours before your procedure. They will also ask you to stop taking certain medications like clopidogrel, which increases the chances of your bleeding during the procedure.
- The target organs of your body will be prepared for brachytherapy. For instance, if you are getting an implant in your gastrointestinal tract, you will be given an enema to clean up your bowels first.
- You will be given sedation, local anesthesia, or general anesthesia. This therapy is mostly performed under general anesthesia.
- Once you are numb to pain and discomfort, your doctor will insert a placement device into your body, e.g. a catheter or an applicator. This helps make sure that the implant will be attached to the right area, and will not move from its place. Sometimes, imaging such as ultrasound, CT, and MRI is used to guide this process.
- Next, the radioactive implant is administered. This can be done manually or with a robot controlled by your doctor.
- Once the implant is fixed in place, the application device is removed if it is not permanent.
- The insertion site will be closed and cleaned
- You will be monitored closely for any short-term complications in the recovery room.6Mayer, C., Gasalberti, D. P., & Kumar, A. (2023, June 15). Brachytherapy. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK562190/
Side Effects of Brachytherapy
The side effects are mostly limited to the implant site. These include:
- Pain
- Irritation
- Swelling
- Redness
- Tissue fibrosis
- Bleeding
- Sometimes, when nearby tissues get harmed, this therapy may result in dysfunction of the organs it gets administered to, e.g., bowel and sexual dysfunction.7Majeed, H., & Gupta, V. (2023, August 14). Adverse Effects of Radiation Therapy. StatPearls. https://www.statpearls.com/point-of-care/28189
Recovery Time
It is usually done as an outpatient procedure and you can usually go home the same day. If general anesthesia is used, you may be hospitalized for a day or two. You can be expected to make a full recovery within a few weeks as long as you follow instructions given by your doctor.
Precautions for Brachytherapy
Adopting precautions before and after this therapy can greatly speed up your recovery as well as reduce your risk of complications. These include:
- Keep the area of your brachytherapy implant site clean and dry in order to avoid infections.
- Avoid strenuous activities which can put pressure on the implant site for as long as your doctor advises.
- Keep a medical card on you with details about the specific kind of implant you have. This way, in case of emergencies, you will be given the appropriate treatment with respect to your condition.
- If you have an implant that makes you emit radiation, stay away from pregnant and young people in order to keep them safe.
- Regularly go to appointments and follow your doctor’s advice in terms of medication, lifestyle changes, and switching up treatment regimens.8Brachytherapy – what patients need to know | IAEA. (2017, July 26). Iaea.org. https://www.iaea.org/resources/rpop/patients-and-public/brachytherapy
Brachytherapy vs. Proton Therapy
Brachytherapy and proton therapy are both emerging cancer treatments. It involves the placement of a radioactive isotope inside your body, meanwhile, proton therapy utilizes positively charged Hydrogen atoms or protons to target tumors near sensitive organs such as the brain and heart.
Conclusion
Brachytherapy is an important modality in cancer management. It can be used as a standalone and complementary therapy for both curative and palliative care. It is ideal for cancers localized to certain body areas. Even though it is an invasive procedure, it has less overall side effects than external radiation therapy.
Refrences
- 1Brachytherapy for Cancer. (2019, January 29). Cancer.gov. https://www.cancer.gov/about-cancer/treatment/types/radiation-therapy/brachytherapy
- 2Brachytherapy. (2024, October). Hopkinsmedicine.org. https://www.hopkinsmedicine.org/health/treatment-tests-and-therapies/brachytherapy
- 3Strohmaier, S., & Grzegorz Zwierzchowski. (2011). Comparison of 60 Co and 192 Ir sources in HDR brachytherapy. Journal of Contemporary Brachytherapy, 4, 199–208. https://doi.org/10.5114/jcb.2011.26471
- 4Clinic, C. (2023, August 25). Brachytherapy, or internal radiation therapy, treats prostate, breast, head and neck, and other cancers. It’s an effective treatment for tumors that haven’t spread. Cleveland Clinic. https://my.clevelandclinic.org/health/treatments/16500-brachytherapy
- 5Park, D. S. (2012). Current Status of Brachytherapy for Prostate Cancer. Korean Journal of Urology, 53(11), 743–743. https://doi.org/10.4111/kju.2012.53.11.743
- 6Mayer, C., Gasalberti, D. P., & Kumar, A. (2023, June 15). Brachytherapy. Nih.gov; StatPearls Publishing. https://www.ncbi.nlm.nih.gov/books/NBK562190/
- 7Majeed, H., & Gupta, V. (2023, August 14). Adverse Effects of Radiation Therapy. StatPearls. https://www.statpearls.com/point-of-care/28189
- 8Brachytherapy – what patients need to know | IAEA. (2017, July 26). Iaea.org. https://www.iaea.org/resources/rpop/patients-and-public/brachytherapy

