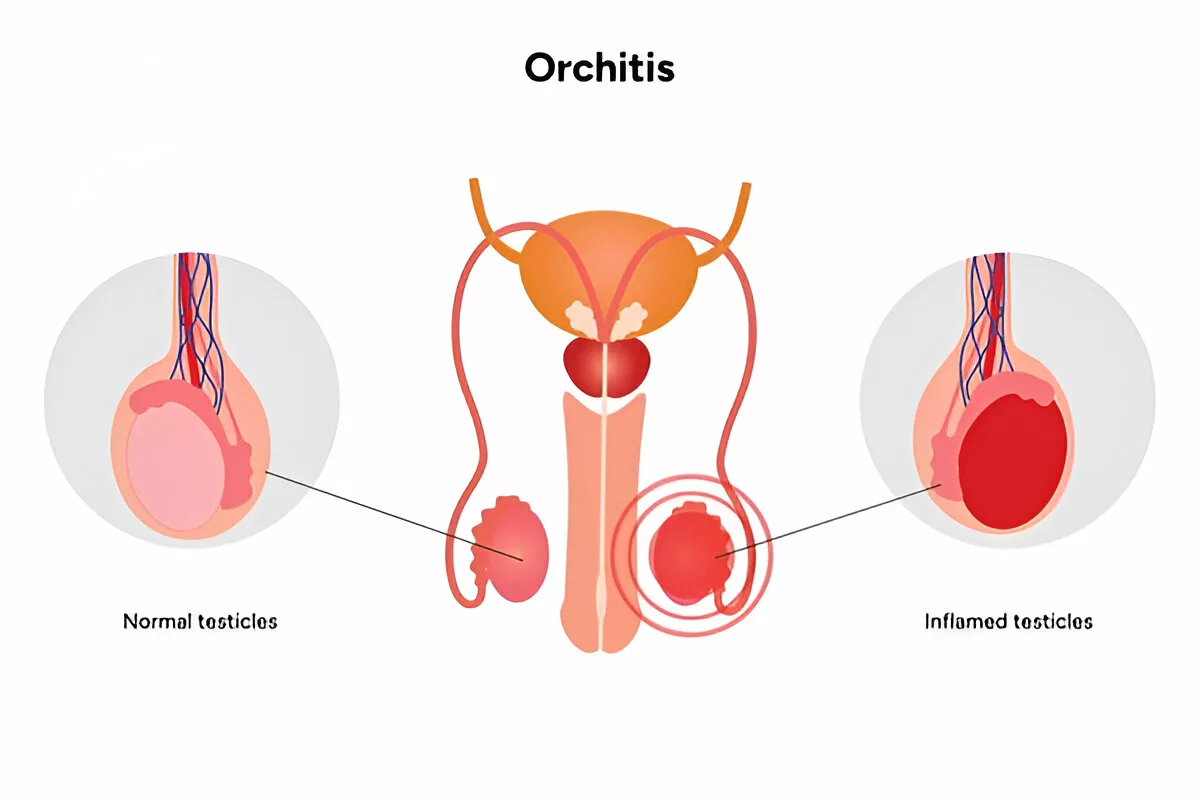
Orchitis is a medical condition characterized by the inflammation of one or both testicles. It’s a painful condition that may result from viral or bacterial infections. You should be vigilant of the symptoms and seek medical attention early because if orchitis is not treated timely, it can cause complications such as damage to the testes or even infertility.1Harvey T. Crook and A. Wayne Aldred — “Orchitis.” StatPearls [NCBI Bookshelf], 2023. This source describes orchitis as inflammation of one or both testicles often due to viral or bacterial infections
Prevalence:
It mostly appears in men who are between 15 to 35 years old, particularly among those who are sexually active. It can also occur in younger boys who have been affected by the mumps virus. About 1 in 3 males who get mumps after puberty will develop orchitis as a complication.2Mun‐Ho Jin and Seung‐Jae Park — “Clinical Features of Mumps Orchitis in Vaccinated Postpubertal Males.” Korean Journal of Urology, 2012. Reports orchitis in 15–40% (approx. 1 in 3) post‑pubertal mumps cases
Orchitis Symptoms
The symptoms can vary depending on whether the cause is viral or bacterial.
Common Symptoms:
The following are the most common signs and symptoms that tend to appear:
- Swelling in one or both testicles: Along with a bulging, heavy scrotum.
- A mild ache or sharp pain that can spread to the groin or the abdomen. Pain with a burning sensation may occur during urination or ejaculation.3Harvey T. Crook et al. — “Epididymitis and Orchitis: An Overview.” American Family Physician, 2009. Offers detailed symptom descriptions including scrotal swelling, fever, and pain on palpation
- Painful testes upon palpation, and this is true even with the slightest touch.
- Usually, in bacterial cases, fever with chills is seen.
- Semen with blood: This is possible, although it is unusual.
- Redness and warmth of the scrotum: It can look inflamed and can be hot to the touch.
- In more severe cases, nausea or general fatigue occurs.
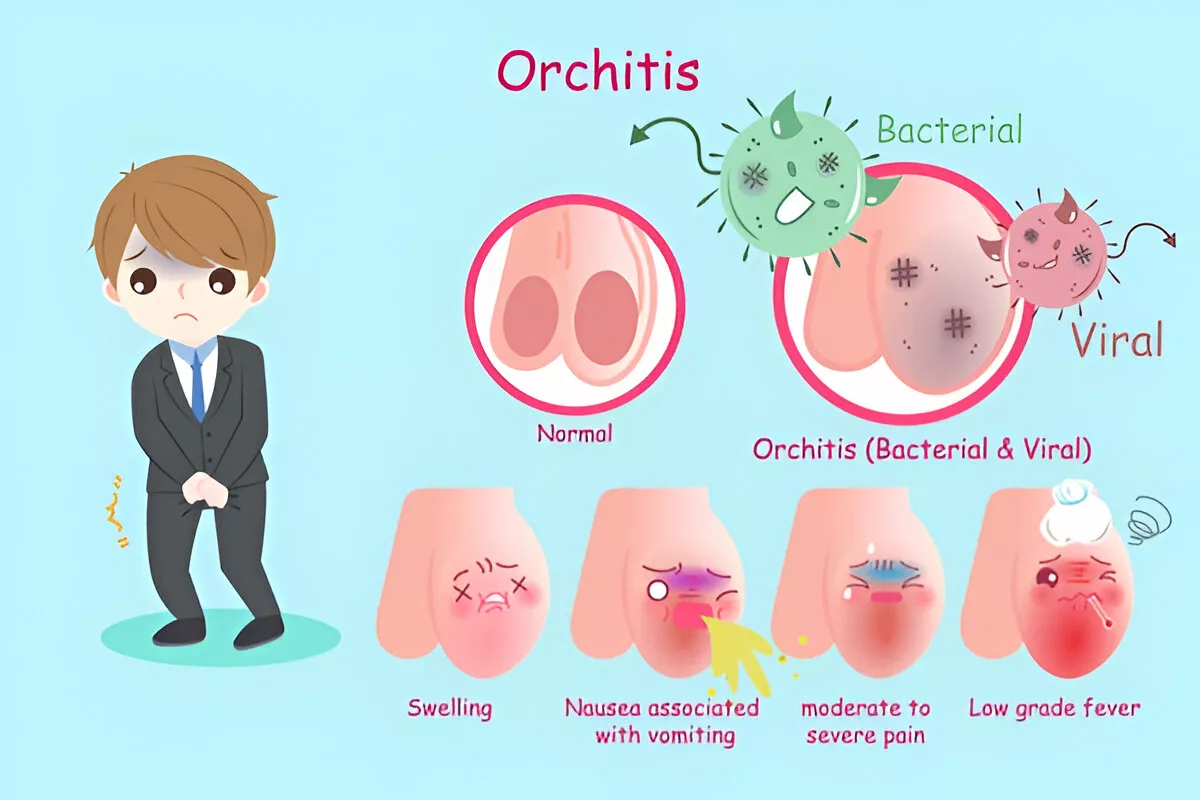
Severe vs Mild Symptoms:
Not all orchitis cases are the same. In the mild forms of the virus (such as in mumps), the symptoms may be confined to swelling and pain. Bacterial orchitis, in turn, is more likely to be accompanied by systemic manifestations, including high fever, nausea, and painful urination.
When to Go to a Doctor?
And at what point is it time to consult a medical practitioner? In case you are feeling:
- Severe pain in the testes with a sudden onset
- Swelling that gets worse within hours
- High fever (over 101°F)
- Pus or unusual discharge from the penis
- Blood in your semen or urine.4Orchitis entry — Wikipedia (April 2025). Lists blood in semen/urine, and scrotal erythema/warmth
The orchitis may not be life-threatening, yet late treatment leads to complications, such as the formation of an abscess or loss of fertility.
Causes & Types of Orchitis
This condition is categorized, in general, into three main categories: viral, bacterial, and non-infectious.
Viral Orchitis:
The most infamous cause of viral orchitis is the mumps virus. Mumps orchitis was a common cause of inflammation of the testes before the era of mumps vaccines. Even today, in unvaccinated populations, this is a real concern.5Zhao et al. — “Mumps Orchitis: Clinical Aspects and Mechanisms.” Frontiers in Immunology, 2021. Highlights mumps, coxsackievirus, echovirus, and CMV as viral agents
Usually, viral orchitis develops 4–7 days after mumps onset, affecting one testicle in most cases.6.StatPearls: Orchitis — Crook & Aldred (2023). Notes orchitis typically begins 4–8 days after parotitis These other viruses are causing orchitis:
- Coxsackievirus
- Echovirus
- Cytomegalovirus (CMV)
The symptoms of viral orchitis are usually mild, and there is no effective antiviral medication other than symptomatic treatment.
Bacterial Orchitis:
This occurs more frequently in sexually active men, mostly in the age group of 19-35 years. The culprits are:7Medscape – Practice Essentials, Etiology of Orchitis (2022). Details bacterial pathogens including Chlamydia, Gonorrhea, and E. coli ascending via urinary tract
- Chlamydia
- Gonorrhea
- Escherichia coli (E. coli) in older men or those having UTIs
In such instances, the infection often spreads to the testicles through the vas deferens from the urethra, bladder, or prostate. The symptoms are severe and need antibiotic therapy.
The risk is much higher for men who have unprotected intercourse or with a history of STIs.
Non-Infectious Causes:
Not all cases of this condition are infection-based. Some rare causes include:8Crook & Aldred — StatPearls (2023). Discusses non‑infectious etiologies such as trauma, autoimmune orchitis, and reflux
- Trauma to the groin area
- Autoimmune attacks in which the body targets its testicular tissue
- The chemical/irritant inflammation may be from urine reflux into the reproductive tract
Those types are rare, but they trigger great discomfort and should be identified and treated.
How is Orchitis Diagnosed?
The diagnosis of this condition is a combination of examination and ruling out other possibilities, such as testicular torsion, a medical emergency.
Medical History & Physical Examination:
Your doctor will begin with an inquiry about the nature of your symptoms, when they started, and how severe they are, and whether you have had any simple infections or sexual activities lately. Physical exam will be checked to include:9Crook & Aldred — StatPearls (2023); American Family Physician, 2009. Emphasizes history, physical findings, and distinction from torsion
- Tenderness or swelling of the testicles
- Scrotal redness
- Temperature and overall condition
Diagnostic Tests:
A physical examination that indicates orchitis, the following tests help to confirm it:10Medscape (2022); StatPearls (2023). Lists diagnostic modalities including urine analysis, STI panels, Doppler ultrasound, and blood tests for leukocytosis and mumps antibodies
- Urine Test: Helps in finding bacteria or white blood cells, which means an infection.
- STI Screenings: Chlamydia and gonorrhea tests, particularly on younger men.
- Scrotal Ultrasound: This is a non-invasive test that determines the blood flow, inflammation, or torsion using sound waves.
- Blood Test: Can show the presence of high levels of white blood cells (infection indicator) or mumps antibodies.
Orchitis Treatment
Once diagnosed, treatment focuses on relieving symptoms and eliminating the infection if one is present. The treatment approach will depend on whether the condition is viral or bacterial.
Medical Treatment:
The cornerstone of orchitis treatment lies in accurately identifying the cause, whether bacterial or viral. If the inflammation is due to bacterial orchitis, antibiotics are a must. Commonly prescribed antibiotics include:11Crook & Aldred — StatPearls (2023). Indicates use of doxycycline, azithromycin, ciprofloxacin, levofloxacin for bacterial causes
- Ciprofloxacin
- Doxycycline
- Azithromycin
- Levofloxacin
These drugs are used for 10-14 days, and improvement of the symptoms is normally started within the first few days of treatment. One must ensure the course of antibiotics is completed, despite the symptoms going away early. This may enable a relapse of infection that is stronger and may be resistant.
In contrast, viral orchitis (most often from mumps) doesn’t respond to antibiotics. In such cases, there is no direct antiviral therapy for orchitis. Instead, it focuses on reducing the pain and inflammation until the body eliminates the virus. Nonsteroidal anti-inflammatory drugs (NSAIDs) are typically prescribed either ibuprofen or naproxen.12Frontiers in Immunology — Zhao et al. (2021); StatPearls (2023). Advise NSAIDs like ibuprofen and rest/supportive care
More complicated cases may occasionally require hospitalization, and such is the case where the pain is too unbearable to manage, or there is the presence of an abscess that requires appropriate incision and drainage.13Medscape (2022). Supports hospitalization for abscess drainage or severe pain .
Home Remedies & Supportive Care:
When you’ve got orchitis, you’re going to want immediate relief. These are some of the tried-and-tested home-care measures that can be helpful in managing the symptoms. Please note that these supportive measures are not substitutes for professional care but can complement prescribed treatment:
- Ice packs: Put a cold compress or ice pack on the scrotum several times a day, 15-20 minutes each time. This helps reduce swelling and pain.
- Use a Supportive Girdle: Wearing an athletic supporter (also called an athletic girdle or a jockstrap, or tight briefs) can stabilize the testicles firmly in place to reduce their movement and pain.
- Take a rest and elevate it: Lie down and have the scrotum raised upon a rolled towel or a small cushion. Don’t do rigorous exercise or sex until healed.
- Drinking lots of fluids and getting rest: Staying well-hydrated and prioritizing rest supports your immune system’s response to infection. These simple actions can aid overall recovery when used alongside appropriate medical treatment.
Recovery Time & Monitoring:
The recovery depends on the cause and the development of complications. In bacterial orchitis, the symptoms tend to improve within 48 to 72 hours of the start of antibiotics, though it might require 2 to 4 weeks before complete recovery. In the case of viral cases, it can take up to 12 weeks to recover, if there are no complications.14Crook & Aldred; Medscape (2022). Provides symptomatic timelines Follow-up visits may be needed to:
- Make sure the symptoms are cured
- Examine testicular atrophy or continued inflammation
- Take action if symptoms worsen or persist
Surgery might be required in some rare cases, especially when an abscess develops or there is damage to the testicles.
Acute vs Chronic Orchitis:
With adequate care, acute orchitis improves within a couple of weeks. However, chronic orchitis may take more time than 6 weeks, and in most cases, it is more difficult to cure. The chronic cases can be due to remaining infections, injuries to the testicles, or systemic inflammation.15Frontiers in Immunology — Zhao et al. (2021). States up to 30–50% testicular atrophy and ~13% subfertility
And when correctly diagnosed, it would define what type it is and be cured accordingly.
Epididymitis vs. Orchitis
The biggest misunderstanding is where epididymitis and orchitis are combined. They are not the same, despite the fact that both of them affect the male reproductive system and are likely to appear at the same time.16Crook & Aldred — American Family Physician (2009). Differentiates based on location, onset, treatment, noting combined form epididymo‑orchitis is common
- Epididymitis is an inflammation of the epididymis, which is a twisted tube situated behind each testicle that stores and transports sperm.
- When the testicle itself becomes inflamed, we say it is orchitis.
| Feature | Orchitis | Epididymitis |
| Location | Testicle(s) | Epididymis (tube behind the testicle) |
| Common Cause | Viral (mumps) | Bacterial (STIs/UTIs) |
| Age Group Affected | Teenagers, adults | Young adult men, older men |
| Treatment | Antivirals (supportive), Antibiotics (bacterial cases) | Antibiotics |
| Onset | Sudden | Gradual |
| Pain Location | Whole testicle | The posterior part of the testicle |
What is Epididymo-Orchitis?
In some cases, these conditions are not isolated. When the epididymitis infects the testicle, it is known as epididymal orchitis. Such a combination is more prevalent than pure orchitis and refers to a situation where both organs are inflamed concurrently.17Street et al. — “2016 European Guideline on the Management of Epididymo‑orchitis.” IUSTI (2017). Reports 2.45 per 1,000 men/year incidence, recommends antibiotics
Symptoms last longer and are more intense, and the treatment routine is normally the same with bacterial orchitis, excessive antibiotics, bed rest, and support. Untreated epididym0-orchitis can lead to an abscess or even infertility in the long term.
Complications & Prevention of Orchitis
Orchitis is usually treatable, but if left untreated, it can lead to a cascade of complications. Here are some potential outcomes:
- Testicular Atrophy: The testicles might shrink due to long-term inflammation and loss of blood supply.
- Infertility: The orchitis caused by the mumps may cause infertility, especially when the sperm-producing tissue is infected.
- Chronic Pain: The patient experiences some discomfort or pain which is likely to last after the disease until several months later.
- Testicular Abscess: In some cases, pus may accumulate within the testicle, forming an abscess that may require surgical drainage.
- Hydrocele: An accumulation of fluid around the testicle (hydrocele) can occur following infection, leading to visible swelling and discomfort.
How to Prevent Orchitis?
Prevention of the onset of orchitis can take the following measures:18Frontiers in Immunology — Zhao et al. (2021); Medscape (2022). Emphasize vaccination, condom use, treating UTIs, protective gear, hygiene
- Vaccination: You should be vaccinated against mumps, which is the first prevention measure against viral orchitis.
- Safe Sex Behavior: Wear condoms and have STI screening to reduce the risks of having STDs.
- Treat UTIs: In cases when it is indicated that there is a UTI due to a burning sensation or frequent urination, it is always recommended that one treat it as fast as possible.
- Avoid Trauma: At the time of a sport or other physical activity, wear protective clothes to avoid damaging your groin.
- Proper Hygiene: Older men should exercise caution to avoid infection of the testicle by ensuring good hygiene.
Most instances of orchitis can be avoided by making some intelligent lifestyle choices and being conscious.
Is Orchitis contagious?
It will depend on the cause. Orchitis is an indirectly contagious disease, whereas the infections that produce it are contagious. For example:
- The mumps virus is very infectious, and it is transmitted via respiratory droplets.19 General clinical consensus; Crook & Aldred (2023). Reinfection is possible without resolving risk factors
- During unprotected sexual intercourse, STIs such as chlamydia or gonorrhea may be contracted.20General clinical consensus; Crook & Aldred (2023). Reinfection possible without resolving risk factors
And, therefore, you can not “catch” orchitis from others; you can catch the infection that causes orchitis.
Can Orchitis go away on its own?
Spontaneous recovery without any special medicine is possible in the viral orchitis, where it is connected with mumps or with some other viruses that have a self-limiting essence. Here, pain relievers, hydration, and rest are normally sufficient.
Nevertheless, the bacterial orchitis cannot be eliminated without treatment. It requires antibiotics to kill the infection. Ignoring treatment may result in chronic pain, sterility, and even the permanent loss of testicles.
Can you get Orchitis twice?
Yes, orchitis can recur, especially when risk factors are not resolved, leading to the development of orchitis a second time. The more times orchitis strikes, the greater the risk of long-term complications. Prevention is key here.
How can Orchitis affect fertility?
One of the most severe long-term side effects of orchitis is fertility problems, particularly in cases caused by the mumps virus or in cases where both testes are affected.21Zhao et al. (2021); Park & Jin (2012). Provide exact figures and study outcomes Complications may include:
- Decreased sperm production
- Testicular atrophy
- Hormonal imbalances
- Scar tissue that blocks sperm flow22Frontiers in Immunology — Zhao et al. (2021). Details on decreased sperm production, atrophy, and hormonal disruption .
If you’ve had orchitis and are trying to conceive, it is better to consult a urologist. Semen analysis may assist in determining the possibility that fertility is affected.
Conclusion
Orchitis is an aching and worrying pathology that needs attention. This is an ailment that could start with sudden pain in the scrotum, to chronic conditions such as infertility.
Do not forget that this disease is not only a personal inconvenience but also may cause serious reproductive consequences. However, you can overcome it with initial medical support, friendly treatment, and proper preventative measures.
Refrences
- 1Harvey T. Crook and A. Wayne Aldred — “Orchitis.” StatPearls [NCBI Bookshelf], 2023. This source describes orchitis as inflammation of one or both testicles often due to viral or bacterial infections
- 2Mun‐Ho Jin and Seung‐Jae Park — “Clinical Features of Mumps Orchitis in Vaccinated Postpubertal Males.” Korean Journal of Urology, 2012. Reports orchitis in 15–40% (approx. 1 in 3) post‑pubertal mumps cases
- 3Harvey T. Crook et al. — “Epididymitis and Orchitis: An Overview.” American Family Physician, 2009. Offers detailed symptom descriptions including scrotal swelling, fever, and pain on palpation
- 4Orchitis entry — Wikipedia (April 2025). Lists blood in semen/urine, and scrotal erythema/warmth
- 5Zhao et al. — “Mumps Orchitis: Clinical Aspects and Mechanisms.” Frontiers in Immunology, 2021. Highlights mumps, coxsackievirus, echovirus, and CMV as viral agents
- 6.StatPearls: Orchitis — Crook & Aldred (2023). Notes orchitis typically begins 4–8 days after parotitis
- 7Medscape – Practice Essentials, Etiology of Orchitis (2022). Details bacterial pathogens including Chlamydia, Gonorrhea, and E. coli ascending via urinary tract
- 8Crook & Aldred — StatPearls (2023). Discusses non‑infectious etiologies such as trauma, autoimmune orchitis, and reflux
- 9Crook & Aldred — StatPearls (2023); American Family Physician, 2009. Emphasizes history, physical findings, and distinction from torsion
- 10Medscape (2022); StatPearls (2023). Lists diagnostic modalities including urine analysis, STI panels, Doppler ultrasound, and blood tests for leukocytosis and mumps antibodies
- 11Crook & Aldred — StatPearls (2023). Indicates use of doxycycline, azithromycin, ciprofloxacin, levofloxacin for bacterial causes
- 12Frontiers in Immunology — Zhao et al. (2021); StatPearls (2023). Advise NSAIDs like ibuprofen and rest/supportive care
- 13Medscape (2022). Supports hospitalization for abscess drainage or severe pain .
- 14Crook & Aldred; Medscape (2022). Provides symptomatic timelines
- 15Frontiers in Immunology — Zhao et al. (2021). States up to 30–50% testicular atrophy and ~13% subfertility
- 16Crook & Aldred — American Family Physician (2009). Differentiates based on location, onset, treatment, noting combined form epididymo‑orchitis is common
- 17Street et al. — “2016 European Guideline on the Management of Epididymo‑orchitis.” IUSTI (2017). Reports 2.45 per 1,000 men/year incidence, recommends antibiotics
- 18Frontiers in Immunology — Zhao et al. (2021); Medscape (2022). Emphasize vaccination, condom use, treating UTIs, protective gear, hygiene
- 19General clinical consensus; Crook & Aldred (2023). Reinfection is possible without resolving risk factors
- 20General clinical consensus; Crook & Aldred (2023). Reinfection possible without resolving risk factors
- 21Zhao et al. (2021); Park & Jin (2012). Provide exact figures and study outcomes
- 22Frontiers in Immunology — Zhao et al. (2021). Details on decreased sperm production, atrophy, and hormonal disruption .

