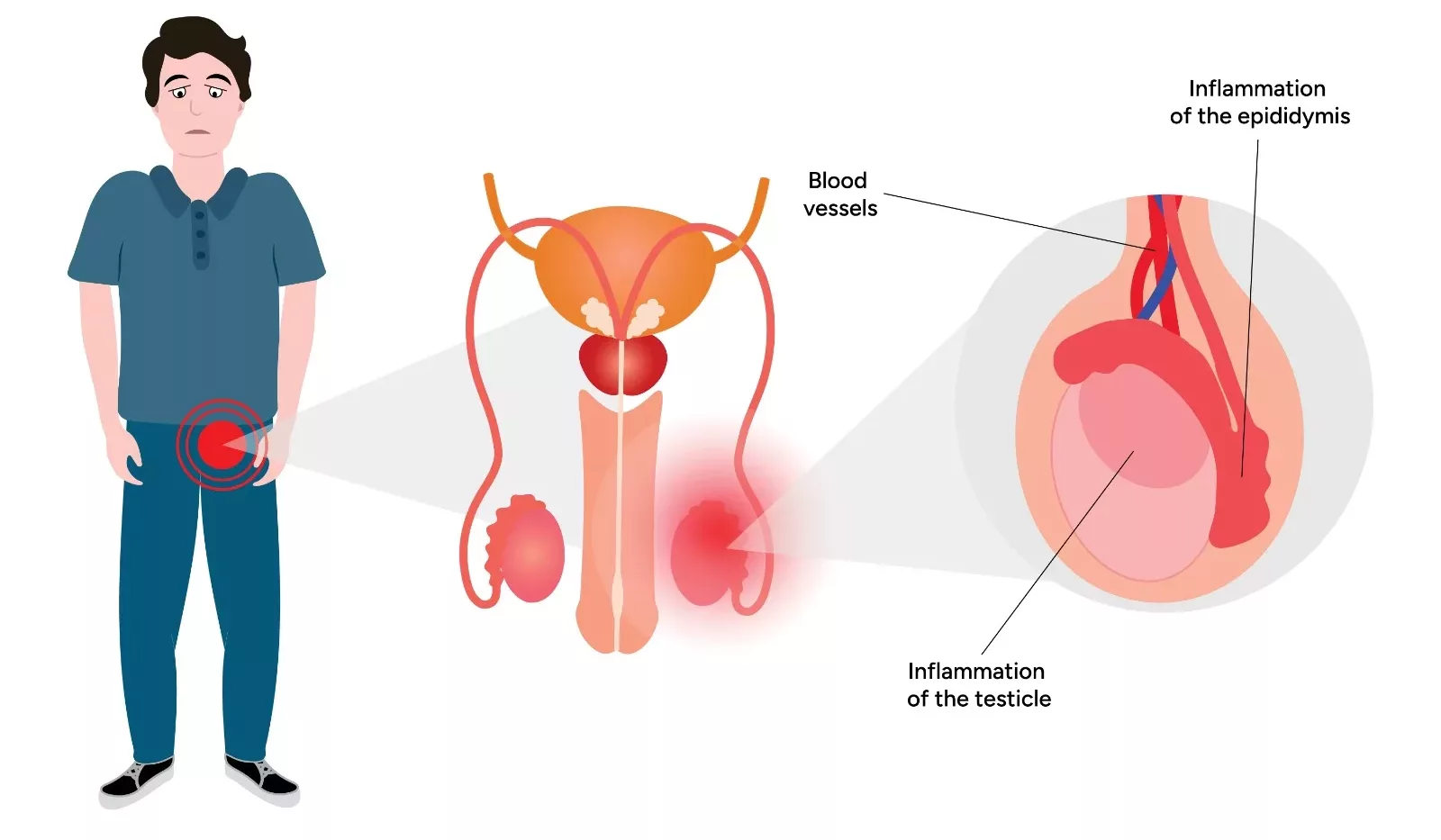
Epididymitis refers to the inflammation of the epididymis. The epididymis is a coiled tube located at the back of the testicle. This tube is responsible for storing and carrying sperm. It commonly presents with gradual-onset scrotal pain, swelling, and tenderness, sometimes radiating to the groin. Urinary symptoms such as dysuria or frequency may also occur. Because its presentation can resemble testicular torsion—a surgical emergency—prompt evaluation is essential. This condition affects males of all ages, though it is most prevalent in men aged 20 to 40. Around 600,000 cases are reported annually in the United States.1Rupp, T.J. and S.W. Leslie, Epididymitis. 2017.
Bacterial infection is the primary cause. In younger men, sexually transmitted organisms like Chlamydia trachomatis and Neisseria gonorrhoeae are common culprits, while older men are more often affected by gram-negative bacteria such as E. coli. Epididymitis can be acute or chronic. When it involves inflammation of the testicle itself, the condition is termed epididymo-orchitis. Treatment usually involves supportive care and antibiotics that target the infection and pain.
Causes of Epididymitis
Epididymitis most often results from a bacterial infection. In older men, this is commonly due to urinary pathogens such as Escherichia coli, often related to bladder outlet obstruction or urinary catheter use. In younger, sexually active men, sexually transmitted infections—particularly Chlamydia trachomatis and Neisseria gonorrhoeae—are the primary causes, accounting for approximately 50% of cases.2Rakhimov, F., EPIDIDYMITIS: MODERN ASPECTS OF ETIOLOGY, DIAGNOSIS AND TREATMENT. International journal of medical sciences, 2025. 1(2): p. 210-213.
In prepubescent boys, epididymitis is less common but can occasionally result from urinary tract infections or, in rare and concerning cases, sexually transmitted pathogens due to possible sexual abuse.
The other possible causes of epididymitis include:
- Chemical epididymitis, caused by the backflow of sterile urine into the vas deferens, usually after heavy straining or procedures.
- Viral infections, such as the mumps virus.
- Drug-induced infections, occasionally associated with certain medications like amiodarone.3Rupp, T.J. and S.W. Leslie, Epididymitis. 2017.
- Non-infectious irritation, from prolonged sitting, excessive cycling, or trauma, which may lead to mechanical inflammation of the epididymis.4Rakhimov, F., EPIDIDYMITIS: MODERN ASPECTS OF ETIOLOGY, DIAGNOSIS AND TREATMENT. International journal of medical sciences, 2025. 1(2): p. 210-213.
Risk Factors
The risk factors include:
- Prior history of urinary tract infection
- A previous history of sexually transmitted disease
- Anatomic abnormalities, such as bladder outlet obstruction
- Prostate or urinary tract surgeries
- Excessive cycling
- Prolonged sitting
- Trauma5McConaghy, J.R. and B. Panchal, Epididymitis: an overview. American family physician, 2016. 94(9): p. 723-726.
Symptoms of Epididymitis
The symptoms of the condition include:
- Gradual-onset scrotal pain and tenderness
- Scrotal swelling or redness
- Pain radiating to the lower abdomen or groin
The urinary symptoms might include:
- Urinary urgency
- Dysuria
- Increased urinary frequency
- Incontinence of urine
- Urethral discharge
Other symptoms include:
- Low-grade fever
- Chills
- Pain in the pelvic area
- Enlarged lymph nodes in the groin (inguinal lymph nodes)
- Blood in semen (hematospermia)
Diagnosis of Epididymitis
The diagnosis of epididymitis is based on a combination of clinical evaluation, laboratory tests, and imaging studies.
History & Physical Examination:
The healthcare provider will ask if you have had a traumatic injury previously. Have you been involved in repetitive activities such as sports? They may inquire about your history of prior sexually transmitted disease exposures and any past medical history involving the genitourinary tract. These problems can include prostatitis, urinary tract infections, and previous surgical procedures. A digital rectal examination may demonstrate tenderness upon palpation of the prostate gland, especially in older males with suspected concurrent prostatitis.6Hongo, H., et al., Novel algorithm for management of acute epididymitis. International Journal of Urology, 2017. 24(1): p. 82-87.
A physical examination of the patient can include:
- Swelling of the scrotum
- Tenderness upon palpation, which is typically unilateral (a hallmark feature of epididymitis)
- Warm, inflamed, and erythematous skin of the scrotum.
- Tender inguinal adenopathy
- Urethral discharge upon examination7Lampejo, T., M. Abdulcadir, and S. Day, Retrospective review of the management of epididymo-orchitis in a London-based level 3 sexual health clinic: an audit of clinical practice. International Journal of STD & AIDS, 2017. 28(10): p. 1038-1040.
Other hallmark signs that may aid diagnosis include:
- Prehn’s sign – Elevation of the scrotum may relieve pain in cases of epididymitis, whereas pain typically persists or worsens in testicular torsion.
- Cremasteric reflex – This is tested by gently stroking the inner thigh, which normally causes the testicle on the same side to elevate due to contraction of the cremaster muscle. This reflex is usually preserved in epididymitis but is often absent in testicular torsion, making it a helpful clinical sign when differentiating the two conditions
Laboratory Tests:
These tests include:
Urinalysis
This test is usually performed for older adults with urinary tract infections. The urine culture test will detect bacteriuria and urinary pathogens if present. The presence of white and red blood cells in the urine is indicative of an acute inflammatory or infectious condition.8Rupp, T.J. and S.W. Leslie, Epididymitis. 2017.
Gram Stains of Urethral Secretions
It is performed to detect the gonococcal infection.
Nucleic Acid Amplification Tests (NAAT)
This test is usually performed for sexually active men at risk for sexually transmitted diseases. The first-void urine or urethral swabs are collected for pathogen detection.
Imaging:
The imaging tests are done to rule out other conditions. These tests offer detailed images that allow your doctors to see the structures of your body very clearly. The imaging modalities used for diagnosing epididymitis include:
Ultrasonography
Scrotal ultrasonography with Doppler is the imaging method of choice. It demonstrates inflammation of the testis and epididymis. Findings may include epididymal enlargement, increased blood flow, and sometimes a reactive hydrocele.
Computed Tomography (CT)
CT scans are not routinely used for diagnosing epididymitis, but can be helpful in patients presenting with flank pain or urinary symptoms associated with acute genitourinary problems such as ureterolithiasis.9Rakhimov, F., EPIDIDYMITIS: MODERN ASPECTS OF ETIOLOGY, DIAGNOSIS AND TREATMENT. International journal of medical sciences, 2025. 1(2): p. 210-213.
Management & Treatment
The treatment of the condition is based on the identification of the cause.
- Pain and swelling can be reduced in many cases by applying ice packs and elevating the scrotum.
- Epididymitis caused by repetitive physical activity or trauma is managed with rest, scrotal support, nonsteroidal anti-inflammatory drugs (NSAIDs), and close follow-up with a primary care provider.
- Empiric (presumptive) antibiotic therapy is initiated based on patient age, risk factors, and the most likely infectious agent.
Treatment for Sexually Transmitted Epididymitis
In men under 35 or those at risk for sexually transmitted infections (STIs), the recommended first-line treatment is:
- Ceftriaxone (250–500 mg IM once) plus
- Doxycycline (100 mg orally twice daily for 10 days)
- Azithromycin (1 g orally once) can be considered as an alternative to doxycycline in some cases.10Yamamichi, F., et al., What are the differences between older and younger patients with epididymitis? Investigative and Clinical Urology, 2017. 58(3): p. 205-209.
Treatment for Non-Sexually Transmitted Epididymitis
In men over 35, or those with a low risk for STIs but a history of urinary tract infections (UTIs) or urinary instrumentation, fluoroquinolones are preferred. Options include:
- Levofloxacin (500 mg orally once daily for 10 days)
- Ofloxacin (300 mg orally twice daily for 10 days)
- These are effective against typical urinary pathogens like E. coli and also active against Chlamydia trachomatis, though doxycycline is preferred for the latter.11Medina-Polo, J., Treatment of Epididymitis and Orchitis, in Guide to Antibiotics in Urology. 2024, Springer. p. 229-238.
Patients with epididymitis caused by urinary tract infection are advised to drink plenty of water and fluids to flush the genitourinary tract. They are advised to take the entire antibiotic therapy and follow up with their providers for further required management.
On the other hand, patients with epididymitis caused by sexually transmitted diseases are advised to refrain from sexual intercourse until they completely recover. The recovery time is from days to weeks for moderate to severe cases.
Preventive Measures
You can reduce the risk of infection and ultimately prevent epididymitis by following these measures:
- Use condoms during sexual activity to prevent STIs.
- Limit the number of sexual partners.
- Get tested and treated for STIs if exposed.
- Practice good genital hygiene.
Differential Diagnosis
The differential diagnosis of epididymitis is not limited to these, but might include:
- Spermatocele
- Testicular torsion
- Scrotal trauma
- Hydrocele
- Orchitis12Rupp, T.J. and S.W. Leslie, Epididymitis. 2017.
Prognosis
The independently associated prognostic factors with the severity of the epididymitis include:
- Previous history of diabetes mellitus
- Older age
- Higher white blood cell count
- Higher blood urea nitrogen levels
- Higher C-reactive protein13Hongo, H., et al., Novel algorithm for management of acute epididymitis. International Journal of Urology, 2017. 24(1): p. 82-87.
Additionally, patients with epididymitis due to a sexually transmitted infection have a greater risk of acquiring and transmitting HIV.14Nusbaum, M.R., et al., Sexually transmitted infections and increased risk of co-infection with human immunodeficiency virus. Journal of Osteopathic Medicine, 2004. 104(12): p. 527-535.
Complications of Epididymitis
If not treated properly, the condition can lead to the following complications:
- Sepsis (rare, but possible in severe or untreated infections)
- Infertility (especially with bilateral involvement or repeated episodes)
- Chronic pain
- Scrotal fibrosis
- Testicular abscess
- Epididymal abscess
Epididymitis Versus Orchitis
The key differences between the two conditions are summarized in the table:
| Feature | Epididymitis | Orchitis |
| Location | Epididymis | Testicle |
| Causes | Bacterial infections and trauma | Viral (e.g., mumps), sometimes bacterial |
| Onset of the disease | Gradual | It might be rapid or gradual |
| Physical findings | Swollen or tender epididymis | Testicular swelling and tenderness |
| Treatment | Supportive care and antibiotic therapy | Symptomatic |
Final Remarks
Epididymitis is a common and often distressing condition. Prompt recognition through careful clinical evaluation, targeted laboratory testing, and confirmatory imaging is mandatory to differentiate it from similar conditions, such as testicular torsion. Early and appropriate antibiotic therapy combined with supportive measures typically leads to rapid symptom improvement and full recovery, but delayed or inadequate treatment can result in complications. Awareness of risk factors, preventive strategies, and timely medical intervention is crucial in managing epididymitis effectively.
Refrences
- 1Rupp, T.J. and S.W. Leslie, Epididymitis. 2017.
- 2Rakhimov, F., EPIDIDYMITIS: MODERN ASPECTS OF ETIOLOGY, DIAGNOSIS AND TREATMENT. International journal of medical sciences, 2025. 1(2): p. 210-213.
- 3Rupp, T.J. and S.W. Leslie, Epididymitis. 2017.
- 4Rakhimov, F., EPIDIDYMITIS: MODERN ASPECTS OF ETIOLOGY, DIAGNOSIS AND TREATMENT. International journal of medical sciences, 2025. 1(2): p. 210-213.
- 5McConaghy, J.R. and B. Panchal, Epididymitis: an overview. American family physician, 2016. 94(9): p. 723-726.
- 6Hongo, H., et al., Novel algorithm for management of acute epididymitis. International Journal of Urology, 2017. 24(1): p. 82-87.
- 7Lampejo, T., M. Abdulcadir, and S. Day, Retrospective review of the management of epididymo-orchitis in a London-based level 3 sexual health clinic: an audit of clinical practice. International Journal of STD & AIDS, 2017. 28(10): p. 1038-1040.
- 8Rupp, T.J. and S.W. Leslie, Epididymitis. 2017.
- 9Rakhimov, F., EPIDIDYMITIS: MODERN ASPECTS OF ETIOLOGY, DIAGNOSIS AND TREATMENT. International journal of medical sciences, 2025. 1(2): p. 210-213.
- 10Yamamichi, F., et al., What are the differences between older and younger patients with epididymitis? Investigative and Clinical Urology, 2017. 58(3): p. 205-209.
- 11Medina-Polo, J., Treatment of Epididymitis and Orchitis, in Guide to Antibiotics in Urology. 2024, Springer. p. 229-238.
- 12Rupp, T.J. and S.W. Leslie, Epididymitis. 2017.
- 13Hongo, H., et al., Novel algorithm for management of acute epididymitis. International Journal of Urology, 2017. 24(1): p. 82-87.
- 14Nusbaum, M.R., et al., Sexually transmitted infections and increased risk of co-infection with human immunodeficiency virus. Journal of Osteopathic Medicine, 2004. 104(12): p. 527-535.

