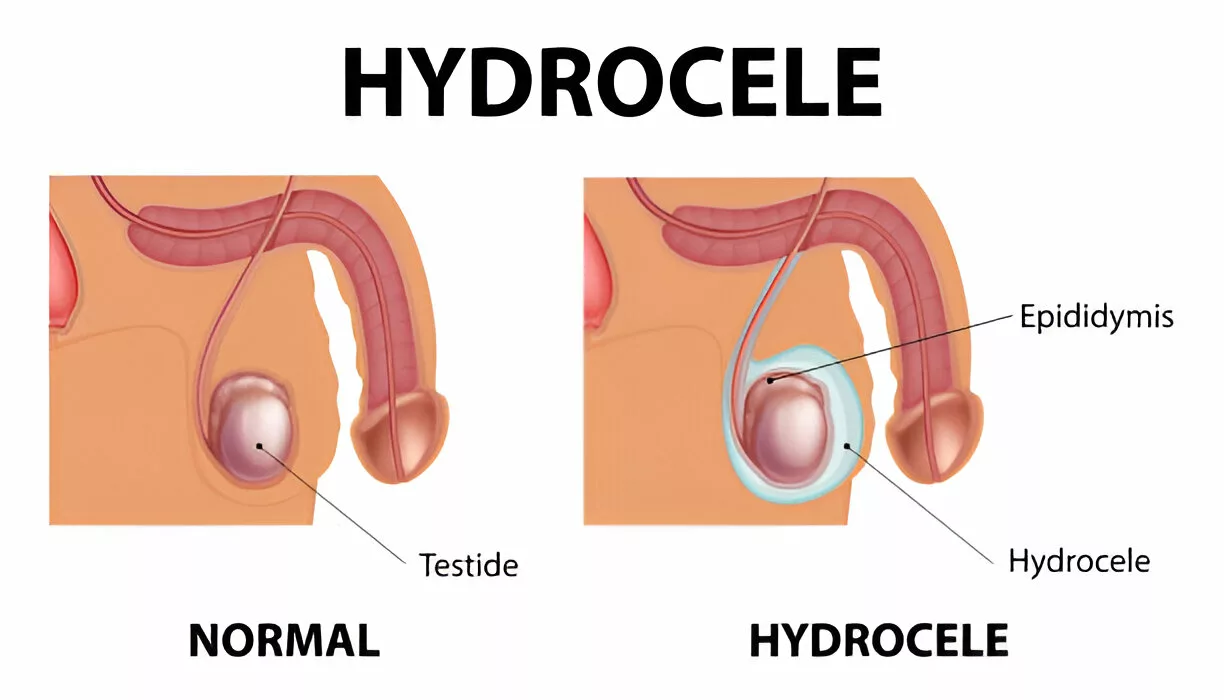
A hydrocele is a fluid-filled sac within the scrotum (skin pouch that houses the testicles). The disorder most commonly affects male infants but may also be present in adults. Hydroceles occur in approximately 10% of male infants at birth and often resolve spontaneously within the first year of life. Survey reports reveal that pediatric hydrocele has a prevalence of 1/1000 infants and 3.4/1000 children.1Xie, X., Pei, J., Zhang, L., & Wu, Y. (2025). Global birth prevalence of major congenital anomalies: a systematic review and meta-analysis. BMC Public Health, 25, 449. Hydrocele in both testes is called bilateral hydrocele. It arises during normal development and resolves without intervention. In most cases, the sac is painless. However, swelling in the scrotum can cause discomfort and interfere with the day-to-day activities of adults. Surgical intervention is only required when the sac doesn’t go away on its own.
Embryological Development & the Structure of the Testes
In normal fetal development, tunica vaginalis is the peritoneal serous membrane that surrounds the testis within the scrotum. Normally, it contains a small amount of viscous fluid to lubricate the testes. It is composed of two layers, i.e., parietal and visceral layers. Fluid accumulation between the tunica layers leads to the development of a hydrocele.
The testes develop in the abdomen (retroperitoneally) and descend out of the abdominal cavity via the inguinal canal. During development, there is communication between the abdomen and the testes through the open tunica vaginalis. But when the testes descend, the tunica vaginalis forms a projection, i.e., processus vaginalis, which obliterates and disconnects the testes from the abdomen. This shuts the surroundings of the testes from the abdomen. Improper closure or insufficient removal of fluid leads to hydrocele formation.
Types Of Hydrocele
The development of hydrocele is categorized into two major types, i.e., primary and secondary causes.
Primary Hydrocele:
There are four types of hydroceles in the primary category:
Congenital
This type of hydrocele arises when the processus vaginalis is fully patent, allowing communication between the abdomen and testes. Peritoneal fluid flows into the scrotum, leading to the formation of a hydrocele.
Infantile
In the infantile type, there is partial obliteration (proximal portion) of the processus vaginalis. However, the distal portion remains patent, allowing fluid accumulation. It accounts for 2.6% of all hydroceles. The sacs can grow to large sizes and are linked to a higher rate of testicular dysmorphisms.2Cozzi, D. A., Mele, E., Ceccanti, S., Pepino, D., d’Ambrosio, G., & Cozzi, F. (2008). Infantile abdominoscrotal hydrocele: a not so benign condition. Journal of Urology, 180(6), 2611-2615.
Encysted Hydrocele of the Cord
Both the distal and proximal portions of the processus vaginalis get blocked, but the central portion remains patent in the encysted hydrocele of the cord.
Vaginal
In vaginal hydrocele is the most common type of hydrocele in adults. It occurs when fluid accumulates between the parietal and visceral layers of the tunica vaginalis (the serous membrane that normally surrounds the testis). In this type, the processus vaginalis has properly closed, and there is no communication with the peritoneal cavity, making it a non-communicating hydrocele. The fluid buildup surrounds the testis, which can make it difficult or impossible to palpate the testis on examination.
Secondary Hydrocele:
As the name indicates, this type arises secondary to some other condition. Underlying pathologies that contribute to the rise of a hydrocele include:
- Infection (Filariasis, TB of the epididymis)
- Injury
- Cancers
Filariasis is a neglected tropical disease (like trypanosomiasis) that can induce scrotal pathologies. Studies show that fliarial hydrocele is a common manifestation of lymphatic filariasis, which poses a significant health burden in endemic regions.3Otabil, K. B., & Tenkorang, S. B. (2015). Filarial hydrocele: a neglected condition of a neglected tropical disease. The Journal of Infection in Developing Countries, 9(05), 456-462.
Another commonly used classification of hydroceles in the medical field is based on the communication status of the testes with the abdomen. So, we have non-communicating hydroceles (tunica vaginalis closes, but the remaining fluid isn’t absorbed by the body) and communicating hydroceles (tunica vaginalis remains patent). Non-communicating hydroceles can be present at birth (or may develop later on).
Another rare type is Nuck’s hydrocele, which occurs in people without testicles. Unlike the prevalent types, the sac develops in the lining of the pelvic wall and may be associated with painful swelling of the inguinal lymph nodes.4Keeratibharat N, Chansangrat J. Hydrocele of the Canal of Nuck: A Review. Cureus. 2022 Apr 2;14(4):e23757. doi: 10.7759/cureus.23757. PMID: 35402114; PMCID: PMC8980195.
Hydrocele Symptoms
Generally, present on both sides, bilateral hydrocele has the following symptoms:
Fluctuating Testicular Swelling:
Patients notice evident, soft swelling in their testicles. The interesting thing about hydroceles is that the size of the swelling changes throughout the day. Painless lump and changing scrotum size are common symptoms of hydroceles.5Dhadwal, A., Kumari, P., & Thakur, C. (2024). A Comprehensive Review on Hydrocele. Research Journal of Pharmacology and Pharmacodynamics, 16(2), 107-113. The undulations in scrotum size are seen in communicating hydroceles due to drainage and movement of abdominal fluids. Generally, no changes in size are seen in non-communicating hydroceles.
Pain And Heaviness
A hydrocele rarely causes discomfort. However, several patients have reported testicular pain due to an underlying hydrocele.6Khalid, D. M. (2024). Testicular pain. InnovAiT, 17(2), 88-94. Patients also report a feeling of heaviness in the testes.
Hydrocele Causes
Hydroceles are part of the normal embryonic and fetal development. Initially, there is communication between the tunica vaginalis and the abdomen, so there is the presence of abdominal fluid in the scrotum naturally. Once the processus vaginalis closes, the fluid gets absorbed, and there is no further entrance of abdominal fluid. However, when the processus vaginalis doesn’t close, there is drainage of fluid in the scrotum from the abdomen. In non-communicating types, there is no new accumulation of fluids, but there is an inability of your body to clear the trapped fluid.
In adults and older children, infections like filariasis cause hydrocele by initiating damage and inflammation of the inguinal lymph nodes. This leads to the accumulation of fluid in the tunica vaginalis.
Do Hydroceles Affect Your Fertility?
No, hydroceles have no impact on your fertility and do not cause infertility.
Hydrocele Diagnosis
The primary step in hydrocele diagnosis is physical examination. Your doctor will take a look at the swelling in the scrotum and may palpate it (to check the fluid accumulation). Doctors often apply pressure to the groin region and ask you to cough. This is done to detect any changes in the size of the sac (due to communication). This test also helps differentiate a hydrocele from a herniation through the abdominal wall, i.e., inguinal hernia.
Specific diagnostic tests for hydrocele include:
Transilumination: Your healthcare provider might shine a light through your scrotum and check for tenderness. The process is called transillumination and helps the professional see fluid within the scrotum. The presence of fluid lights up the testes on passing of the light.
Imaging studies: When significant swelling is present, your doctor might also order multiple imaging studies to rule out other serious conditions like cancer. A pelvic ultrasound is the most commonly adopted test that creates good images of the soft tissues (including testes). A CT scan provides detailed cross-sectional images of the testicles and aids in the diagnosis of the condition.
Differential Diagnosis:
Hydrocele Vs Varicocele
Patients feel testicular swelling in both conditions. However, in the case of a hydrocele, there is the presence of fluid around the testicles, whereas in a varicocele, there is dilation or enlargement of the testicular veins.
Hydrocele Vs Inguinal Hernia
Hydroceles are often mistaken for inguinal hernia and vice versa. Inguinal hernias arise when your intestine pushes out through the skin (weak abdominal wall). This can be due to protrusion of an organ or when the testicular sac (mostly communicable) becomes large enough to push the intestines out to form a bulge.
Other conditions that fall under the differential diagnosis include:
- Epididymitis
- Epididymal cyst
- Hematocele
Hydrocele Treatment
In the vast majority of infant cases, the hydrocele goes away within 2 years after birth and doesn’t need treatment. So, you need not worry about your child’s swelling. However, you might need to consult a urologist (urinary tract specialist) if the swelling becomes large.
In adults, hydroceles secondary to infection or trauma resorb after the underlying cause is properly treated. Most doctors keep small swellings under observation by regularly performing ultrasounds and exams.
Hydrocelectomy:
Surgery is reserved for cases that do not heal themselves. During a hydrocelectomy, a surgeon removes the hydrocele under anesthesia. After removal, a dressing is placed on the incision site. Sometimes, the doctor also passes a drainage tube (and keeps it there for a couple of days) to drain out the accumulated fluid. The process usually takes a few hours, and you can go home on the same day. Research shows that hydrocelectomy is the most effective treatment modality and, therefore, the gold standard in the management of hydroceles.7Rashid, S., Kishore, A., Ahmad, B., Liang, L. M. S., Mironov, O., & Mahmood, S. U. (2024). Sclerotherapy in the Treatment of Hydroceles: A Comprehensive Review of the Efficacy, Types of Sclerosants, and Comparative Outcomes Against Hydrocelectomy. Canadian Association of Radiologists Journal, 75(4), 921-930.
Sclerotherapy:
This is a procedure to treat varicose veins, but has been shown to be effective in hydrocele as well. In this, the doctor injects a solution into the hydrocele that causes scarring. This eventually leads to the stoppage of fluid accumulation and consequent alleviation of symptoms. The most commonly used solutions (agents) include phenol, tetracycline antibiotics, plidocanol, and sodium tetradecyl sulfate. Sclerotherapy and aspiration are great alternatives to surgery.8Shakiba, B., Heidari, K., Afshar, K., Faegh, A., & Salehi-Pourmehr, H. (2023). Aspiration and sclerotherapy versus hydrocelectomy for treating hydroceles: a systematic review and meta-analyses. Surgical Endoscopy, 37(7), 5045-5051.
Aspiration:
Sometimes, doctors opt for needle aspiration, in which they drain the fluid from your scrotum using long needles. It is the preferred mode of treatment for patients who have a high risk of post-surgical complications. Monotherapy with aspiration has limited success. Thus, most of the time, aspiration is paired with sclerotherapy to get the job done.9Stapleton, P., Sathianathen, N. J., & Johns-Putra, L. (2024). Aspiration and Sclerotherapy for the Management of Hydrocele in an Ambulatory and Regional Setting. Société Internationale d’Urologie Journal, 5(6), 835-842.
Recurrence of a hydrocele, though rare, can happen if there is insufficient removal of the tunica vaginalis or the underlying cause is not completely eliminated.
Final Word
A hydrocele is a fluid-filled sac that develops in the scrotum of infants and adults. In infants, it is a normal process of development, and the sac goes away on its own. It may be caused by communication between the scrotum and the abdominal cavity due to a patent processus vaginalis. However, the sacs may arise even after closure of the processus vaginalis (non-communicating hydroceles). Most hydroceles are painless and only cause swelling, heaviness of the testes. Infection and trauma can contribute to its occurrence. Doctors diagnose it with transillumination and imaging studies. The majority of cases don’t need treatment. Non-resolving sacs can be treated non-surgically with sclerotherapy and needle aspiration. However, surgical removal (hydrocelectomy) remains the gold standard of treatment.
Refrences
- 1Xie, X., Pei, J., Zhang, L., & Wu, Y. (2025). Global birth prevalence of major congenital anomalies: a systematic review and meta-analysis. BMC Public Health, 25, 449.
- 2Cozzi, D. A., Mele, E., Ceccanti, S., Pepino, D., d’Ambrosio, G., & Cozzi, F. (2008). Infantile abdominoscrotal hydrocele: a not so benign condition. Journal of Urology, 180(6), 2611-2615.
- 3Otabil, K. B., & Tenkorang, S. B. (2015). Filarial hydrocele: a neglected condition of a neglected tropical disease. The Journal of Infection in Developing Countries, 9(05), 456-462.
- 4Keeratibharat N, Chansangrat J. Hydrocele of the Canal of Nuck: A Review. Cureus. 2022 Apr 2;14(4):e23757. doi: 10.7759/cureus.23757. PMID: 35402114; PMCID: PMC8980195.
- 5Dhadwal, A., Kumari, P., & Thakur, C. (2024). A Comprehensive Review on Hydrocele. Research Journal of Pharmacology and Pharmacodynamics, 16(2), 107-113.
- 6Khalid, D. M. (2024). Testicular pain. InnovAiT, 17(2), 88-94.
- 7Rashid, S., Kishore, A., Ahmad, B., Liang, L. M. S., Mironov, O., & Mahmood, S. U. (2024). Sclerotherapy in the Treatment of Hydroceles: A Comprehensive Review of the Efficacy, Types of Sclerosants, and Comparative Outcomes Against Hydrocelectomy. Canadian Association of Radiologists Journal, 75(4), 921-930.
- 8Shakiba, B., Heidari, K., Afshar, K., Faegh, A., & Salehi-Pourmehr, H. (2023). Aspiration and sclerotherapy versus hydrocelectomy for treating hydroceles: a systematic review and meta-analyses. Surgical Endoscopy, 37(7), 5045-5051.
- 9Stapleton, P., Sathianathen, N. J., & Johns-Putra, L. (2024). Aspiration and Sclerotherapy for the Management of Hydrocele in an Ambulatory and Regional Setting. Société Internationale d’Urologie Journal, 5(6), 835-842.

