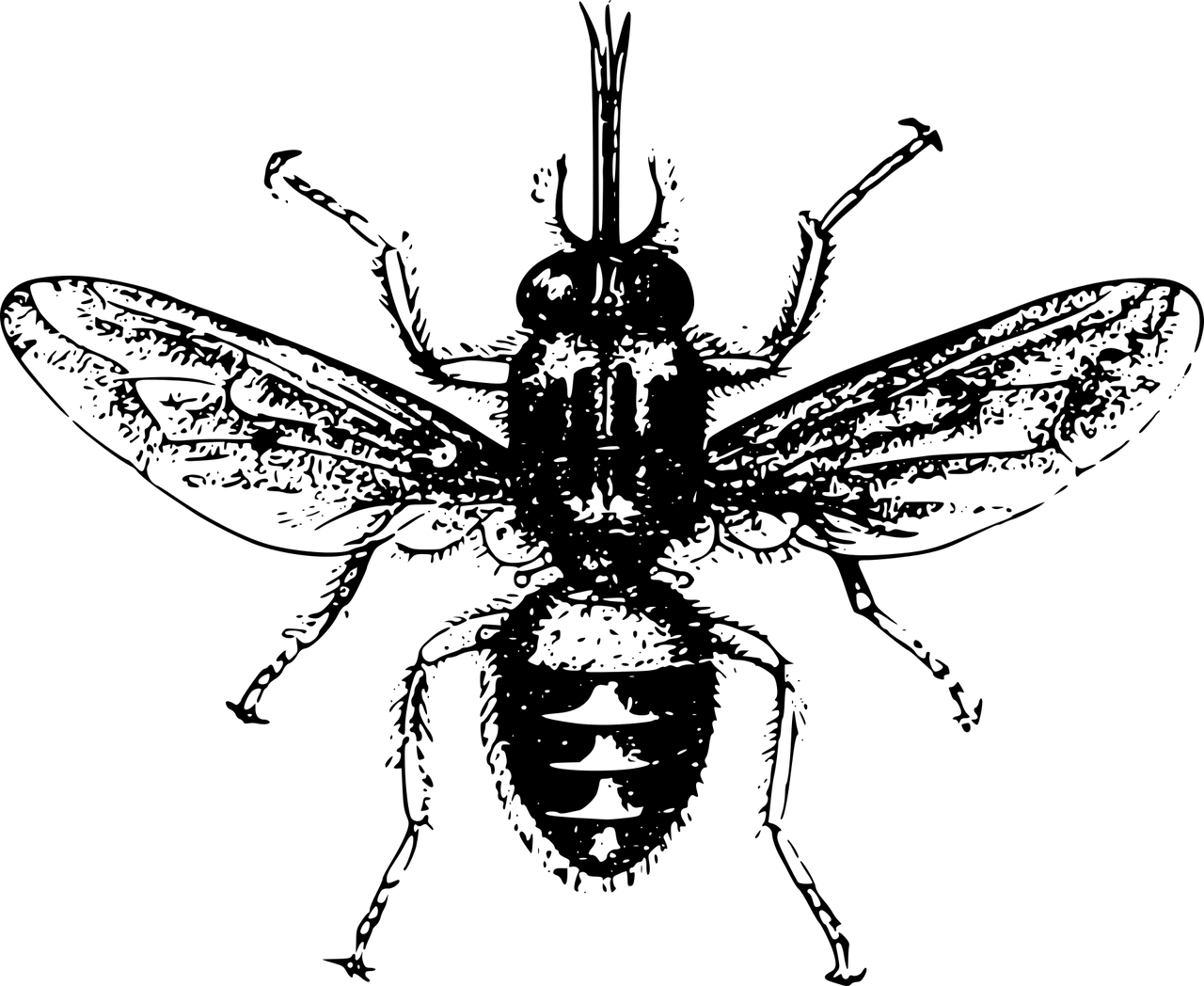
Trypanosomiasis, or Human African trypanosomiasis (HAT), commonly known as the African sleeping sickness /Sleeping sickness, is a parasitic, infectious disease caused by the protozoan Trypanosoma brucei (Gambian and Rhodesian). It is a vector-borne disease, and the parasite gets transmitted to humans via the bite of a tsetse fly (belonging to the Glossina genus). Tsetse flies are common in sub-Saharan regions of Africa (most prevalent in the sub-Saharan populations). The highest number of cases are reported in the Republic of Congo, but the numbers are declining, thanks to the extensive preventive measures. As per a 2022 report, the prevalence of HAT infection in Congo was 0.3%.1Elenga, V. A., Lissom, A., Elion, D. O. A., Vouvoungui, J. C., Djontu, J. C., Boumpoutou, R. K., … & Ntoumi, F. (2022). Risk factors and prevalence of human African trypanosomiasis in individuals living in remote areas of the Republic of Congo. BMC Public Health, 22(1), 2322.
The disease causes swollen bumps on the bite site, muscle/joint aches, fever, and altered mental status. Patients often have trouble walking and find it difficult to stay awake (thus the name sleeping sickness!). The disease tends to spread to different parts of the body and can also involve the brain and the spinal cord, leading to severe consequences. Untreated trypanosomiasis can lead to seizures, coma, and even death. Mostly, doctors prescribe different classes of drugs to manage trypanosomiasis (depending on the condition of the patient and the extent of organ involvement).
Stages Of Trypanosomiasis
There are two main stages of trypanosomiasis, i.e., hemolymphatic and meningo-encephalitic.2Malvy, D., & Chappuis, F. (2011). Sleeping sickness. Clinical Microbiology and Infection, 17(7), 986-995. However, experts also identify another initial stage where skin manifestations are seen.
The infection’s initial stage develops a few days (to a few weeks) after the tsetse fly bite. The initial presentations include skin lesions. The trypanosomal chancre is a typical sore that develops due to the protozoal infection. The sore is painful and appears red and indurated.
Hemolymphatic Stage
The first stage is characterized by the spread of the infection through body fluids. During this stage, the Trypanosoma parasite multiplies and disseminates into the blood vessels and lymphatic system (liver, spleen, heart, and endocrine organs). As the main carriers are blood (hemo-) and lymph, this stage is called the hemolymphatic stage. Patients experience swelling of lymph nodes (lymphadenopathy), headaches, fever, and muscle/joint aches during this period.
Central Nervous System (CNS) Stage
In the later stage, the infectious parasite crosses the blood-brain barrier and affects the CNS (brain and spinal cord). The Gambian type of parasite usually takes several months (to years) to reach the brain. However, with the Rhodesian type, CNS involvement can set in within a few weeks. Individuals report serious symptoms like personality changes, tremors, loss of muscle control, persistent headaches, etc. Patients in the CNS stage require aggressive and immediate treatment, as untreated patients can die in a coma.
Trypanosomiasis Symptoms
Skin Bumps & Rash
There are multiple dermatological presentations of protozoal infections. However, the first symptom to develop in human trypanosomiasis is a red bump on the bite site. Many individuals are capable of recalling exposure to tsetse flies. In patients, fever and adenopathies accompany skin lesions. Microscopic analyses confirm a diagnosis of trypanosomiasis based on trypanosomal chancres presence.3Hope-Rapp, E., Klement, E., Danis, M., Bricaire, F., & Caumes, E. (2009, February). Double trypanosomal chancre revealing West African trypanosomiasis in a Frenchman living in Gabon. In Annales de Dermatologie et de Venereologie (Vol. 136, No. 4, pp. 341-345).
In a clinical study, a French patient diagnosed with African sleeping sickness showed skin lesions. A 37-year-old worker had a macular skin rash (flat and red) on the arms and the trunk. In addition to the rash, the patient’s skin blanched (turned white on pressing). Sometimes later, pruritic (itchy) lesions developed on the trunk that interfered with daily activities.4Ezzedine, K., Darie, H., Le Bras, M., & Malvy, D. (2007). Skin features accompanying imported human African trypanosomiasis: hemolymphatic Trypanosoma gambiense infection among two French expatriates with dermatologic manifestations. Journal of Travel Medicine, 14(3), 192-196.
Fever & Chills
In the early stages of the disease, there is intermittent fever, which is indicative of infection. However, there is a high-grade fever as the parasite affects the CNS. Many patients report recurrent fever (which comes and goes) as a concerning symptom. High fever induces chills in some patients. Fever is an important feature of protozoal diseases such as leishmaniasis, trypanosomiasis, etc.5Johnston, V., Stockley, J. M., Dockrell, D., Warrell, D., Bailey, R., Pasvol, G., … & British Infection Society. (2009). Fever in returned travelers presenting in the United Kingdom: recommendations for investigation and initial management. Journal of Infection, 59(1), 1-18. Some clinicians have noted significantly higher fevers in younger patients (below 18 years of age).
Headaches
Persistent headaches in trypanosomiasis patients usually indicate CNS involvement by the parasite. In a study, it was revealed that headaches are present in around 24.5% of the patients.6Kennedy, P. G. (2008). The continuing problem of human African trypanosomiasis (sleeping sickness). Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society, 64(2), 116-126.
 However, another study found headache to be one of the most common symptoms (present in 78.7% cases) of Human African Trypanosomiasis. Sleep issues and neurological and psychiatric disturbances almost always accompany headaches.7Ortiz-Martínez, Y., Kouamé, M. G., Bongomin, F., Lakoh, S., & Henao-Martínez, A. F. (2023). Human African Trypanosomiasis (Sleeping Sickness)—Epidemiology, Clinical Manifestations, Diagnosis, Treatment, and Prevention. Current Tropical Medicine Reports, 10(4), 222-234.
However, another study found headache to be one of the most common symptoms (present in 78.7% cases) of Human African Trypanosomiasis. Sleep issues and neurological and psychiatric disturbances almost always accompany headaches.7Ortiz-Martínez, Y., Kouamé, M. G., Bongomin, F., Lakoh, S., & Henao-Martínez, A. F. (2023). Human African Trypanosomiasis (Sleeping Sickness)—Epidemiology, Clinical Manifestations, Diagnosis, Treatment, and Prevention. Current Tropical Medicine Reports, 10(4), 222-234.
Muscle & Joint Pains
A highlighting feature of trypanosomiasis is joint pain (arthralgia) and myalgia (muscle ache). Parasitic arthritis is seen in several parasitic infections, including trypanosomiasis, which leads to inflammation and joint aches.8Márquez-Hernández, J. D. (2019). Parasitic arthritis. Infections and the Rheumatic Diseases, 301-314. Myalgias and arthralgias further contribute to sleeping difficulties in patients and a generalized reduction in quality of life.9Willyard, C. (2011). Putting sleeping sickness to bed. Nature Medicine, 17(1), 14-18.
Sleeping Disorders
More than 74% of patients report sleep disturbances; therefore, the name. The major causes of excessive sleeping in patients are attributed to:
- Nocturnal (night-time) insomnia
- Daytime somnolence (drowsiness)
- Uncontrolled sleep episodes
- Reversal of the sleep/wake cycle

The exact mechanism of the sleeping sickness infection is not confirmed, but experts believe that brain infections (such as Trypanosoma infection) target the sleep-wake-regulatory neuronal cell groups. Thus, this impact leads to abruptions in sleep.10Tesoriero, C., Del Gallo, F., & Bentivoglio, M. (2019). Sleep and brain infections. Brain Research Bulletin, 145, 59-74.
As per a study, more than 45% of patients suffer from sleep disorders. Other symptoms accompanying sleeping problems include fever, headache, and general body pain.11Kagira, J. M., Maina, N., Njenga, J., Karanja, S. M., Karori, S. M., & Ngotho, J. M. (2011). Prevalence and types of coinfections in sleeping sickness patients in Kenya (2000/2009). Journal of Tropical Medicine, 2011(1), 248914.
Another study revealed that Trypanosoma brucei interferes with sleep timing as well as with sleep architecture. Animal studies highlight a reduced homeostatic sleep response to sleep deprivation in patients. Moreover, there was a reduced electrophysiological response in infected mice.12Rijo-Ferreira, F., Bjorness, T. E., Cox, K. H., Sonneborn, A., Greene, R. W., & Takahashi, J. S. (2020). Sleeping sickness disrupts the sleep-regulating adenosine system. Journal of Neuroscience, 40(48), 9306-9316.
Altered Mental Status
With this particular infection, the involvement of the brain and spinal cord is quite evident. The protozoal pathogen crosses the blood-brain barrier to affect the spinal cord. Most patients report significant alterations in memory, cognition, and muscle control during the CNS stage of the disease.
Confusion:
As per a study, 6.7% of patients reported mental confusion as an early symptom of HAT. Sleeping disorders and fevers usually accompany mental alterations.13Kato, C. D., Nanteza, A., Mugasa, C., Edyelu, A., Matovu, E., & Alibu, V. P. (2015). Clinical profiles, disease outcome and co-morbidities among T. b. rhodesiense sleeping sickness patients in Uganda. PloS one, 10(2), e0118370.
Memory & Cognitive Issues:
Once the parasite crosses the blood-brain barrier, it impacts the brain’s neuronal pathways. The abruptions in synaptic conduction lead to cognitive issues and sleep disorders.14Kristensson, K., Nygård, M., Bertini, G., & Bentivoglio, M. (2010). African trypanosome infections of the nervous system: parasite entry and effects on sleep and synaptic functions. Progress in neurobiology, 91(2), 152-171.
Ataxia & Walking Difficulties:
HAT induces poor muscle control and coordination. This leads to trouble in maintaining balance while walking. A 38-year-old man, diagnosed with the African sleeping sickness presented with drowsiness and a feeling of being off-balance while walking. He also reported having fevers, chills, and episodes of memory loss and his wife claimed he preferred to “sleep the day away”.15Domachowske, J., Suryadevara, M., Domachowske, J., & Suryadevara, M. (2020). African Sleeping Sickness: African Trypanosomiasis. Clinical Infectious Diseases Study Guide: A Problem-Based Approach, 307-311.
Anemia & Lymph Node Swelling
As already mentioned, the parasite affects the lymphatic structures, such as lymph nodes, and causes swelling. Lymphadenopathy in travelers who have been to tsetse fly-rich areas should be properly investigated. Swelling of lymph nodes, particularly along the back of the neck, is commonly associated with the early stage of African trypanosomiasis, also known as African sleeping sickness. It is called the Winterbottom’s sign and is most frequently seen in infections caused by Trypanosoma brucei gambiense. It also causes a breakdown of blood cells. So, patients may also experience symptoms of anemia.
Seizures & Coma
If left untreated, trypanosoma infection can lead to severe neurological symptoms such as seizures and coma. These effects can eventually lead to death. When left untreated, death ensues in weeks to months.
Causes Of Trypanosomiasis
There are two different types of Trypanosoma protozoa.
Trypanosoma Brucei Gambiense:
It is the prevalent form responsible for disease outbreaks in Western Africa. 92% of all the reported cases are victims of the Gambiense variant. According to the World Health Organization, this type is found in 24 countries of Africa (west and central Africa).16World Health Organization. (2023). Trypanosomiasis, human African (sleeping sickness). Retrieved from [https://www.who.int/news-room/fact-sheets/detail/trypanosomiasis-human-african-(sleeping-sickness)](https://www.who.int/news-room/fact-sheets/detail/trypanosomiasis-human-african-(sleeping-sickness)) It generally causes chronic illness that takes months or even years for the disease to advance to CNS involvement.
Trypanosoma Brucei Rhodesiense:
This is a rare form of protozoan (infecting around 8% of the patients). The Rhodesiense type inhabits 13 countries and rapidly progresses to multi-organ invasion (especially the brain).
The parasitic disease mainly induces an inflammatory response in the brain’s hypothalamic structures, potentially leading to circadian rhythm dysfunction.17Lundkvist, G. B., Kristensson, K., & Bentivoglio, M. (2004). Why trypanosomes cause sleeping sickness. Physiology, 19(4), 198-206.
Is Trypanosomiasis Contagious?
There are no reported cases of Trypanosoma from human-to-human contact (skin contact, blood transfusion, exchange of sexual and body fluids). However, pregnant mothers can transfer the parasite to the fetus (in the womb). Though rare, there are still chances of acquiring the disease via blood exchange as the parasite spreads through the blood.
Tsetse fly acquires the Trypanosoma protozoa from an infected human or animal (cattle, pigs, horses, etc.). Therefore, you can only get infected if the tsetse fly gets infected by biting the infected person, and then the fly bites you.
How To Diagnose Trypanosomiasis?
History & Physical Examination:
Your healthcare provider will take your medical history. An important question is recent traveling to tsetse fly areas (like Africa). After noting the history, your doctor will perform a physical examination.
Diagnostic Tests:
Microscopic Examination
An important test is to detect the presence of the pathogenic parasite in the body fluids. Pathologists observe the samples (of lymph and cerebrospinal fluid) under a microscope.
Blood test:
Your health provider will withdraw a small amount of blood from a vein and observe it under the microscope. In most cases, a blood smear under a microscope effectively shows the presence of the parasites.
Lymph Node Fluid Test:
In this test, the doctor withdraws a small amount of lymph fluid from your lymph nodes via a needle.
Spinal Tap Test:
In the spinal tap test, healthcare providers collect spinal fluid using a needle that is inserted in the lower back (lumbar vertebrae).
Chancre Fluid:
Your doctor may withdraw fluid from the trypanosomal chancre to observe it under the microscope. Rarely, doctors may opt for contents of the bone marrow to check for parasite presence.
American Trypanosomiasis Vs. Human African Trypanosomiasis
There are different types of disease-causing parasites. Another species of the protozoa Trypanosoma family, i.e., Trypanosoma cruzi, is responsible for the Chagas disease (aka American trypanosomiasis).18Suárez, C., Nolder, D., García-Mingo, A., Moore, D. A., & Chiodini, P. L. (2022). Diagnosis and clinical management of Chagas disease: An increasing challenge in non-endemic areas. Research and reports in tropical medicine, 13, 25. The symptoms of Chagas disease are different from those of African sleeping sickness. This disease is predominantly found in Central and South America and Mexico, where it is transmitted by triatomine bugs (“kissing bugs”). Common symptoms include swelling at the injection site, fever, and heart complications if untreated.
On the other hand, Human African Trypanosomiasis, or African sleeping sickness, is caused by Trypanosoma brucei, transmitted by the tsetse fly in sub-Saharan Africa. This illness leads to symptoms like fever, severe headaches, lymph node swelling (notably Winterbottom’s sign), and neurological disturbances as it progresses, potentially leading to a fatal outcome if left untreated. Therefore, both diseases should not be confused as one.
Trypanosomiasis Treatment
Trypanosomiasis is curable, but it requires timely diagnosis and treatment. Two factors determine the type and extent of treatment:
- Type of parasite variant (Gambeinse or Rhodesiense)
- Extent of organ involvement
Anti-Parasitic Medications
Doctors prescribe the following medications for African sleeping sickness:
Suramin & Melarsoprol:
These drug work well for the initial stage of East African sleeping sickness and is effective against the Rhodesiense variant. Suramin and melarsoprol were initially used as first-line therapy drugs for young individuals (below 6 years of age). Melarsoprol is also effective against the Rhodesiense type.
However, now doctors prefer drugs like fexinidazole because it is effective in both stages of rhodesiense human African trypanosomiasis.19Lindner, A. K., Lejon, V., Barrett, M. P., Blumberg, L., Bukachi, S. A., Chancey, R. J., … & Priotto, G. (2024). New WHO guidelines for treating rhodesiense human African trypanosomiasis: expanded indications for fexinidazole and pentamidine. The Lancet Infectious Diseases.
Pentamidine & Fexinidazole:
This is an effective diamidine drug, prescribed for Trypanosoma brucei gambiense infection. Pentamidine is injected intra-muscularly whereas fexinidazole is an oral drug that helps manage non-severe cases of African sleeping sickness.
Eflornithine & Nifurtimox:
Eflornithine is an intravenous drug that can be used as monotherapy to treat the condition. Nifurtimox is an oral drug used in patients suffering from 2nd stage of the disease. Both eflornithine and nifurtimox are effective against Trypanosoma brucei gambiense.
Nifurtimox & Eflornithine Combination Therapy (NECT)
Doctors now prefer using nifurtimox and eflornithine combined therapy to manage 2nd stage HAT cases. Clinical research suggests that the combination therapy is effective and shows promising results.20Kuemmerle, A., Schmid, C., Kande, V., Mutombo, W., Ilunga, M., Lumpungu, I., … & Valverde Mordt, O. (2020). Prescription of concomitant medications in patients treated with Nifurtimox Eflornithine Combination Therapy (NECT) for T. b. gambiense second-stage sleeping sickness in the Democratic Republic of the Congo. PLoS Neglected Tropical Diseases, 14(1), e0008028. Another study concluded NECT to be a safe and effective treatment modality for advanced cases.21Neau, P., Hänel, H., Lameyre, V., Strub-Wourgaft, N., & Kuykens, L. (2020). Innovative partnerships for the elimination of human African trypanosomiasis and the development of fexinidazole. Tropical Medicine and Infectious Disease, 5(1), 17.
Symptomatic Management
In addition to the anti-parasitic drugs, doctors can prescribe you medications for symptomatic management of the conditions. Your doctor may advise the following medicines:
- Corticosteroids (for reduction of inflammation/swelling)
- Pain-killers (analgesics)
- Anti-malarial drugs
Trypanosomiasis Prevention
Mass screening and vector control measures such as tiny target implementation (catching tsetse flies) have been shown to reduce the occurrence of Gambian human African trypanosomiasis.22Kaba, D., Djohan, V., Berté, D., Ta, B. T. D., Selby, R., Kouadio, K. A. D. M., … & Courtin, F. (2021). Use of vector control to protect people from sleeping sickness in the focus of Bonon (Côte d’Ivoire). PLoS Neglected Tropical Diseases, 15(6), e0009404.

There is no vaccine for the condition. Therefore, prevention is your best chance of saving yourself from a fatal encounter. You can adopt the following steps to stay safe:
- Do not travel to infected areas (East Africa, etc.).
- Stay indoors. If you are in an endemic area, avoid movement during the day and stay away from bushes and shrubs.
- Wear long, thick clothes (full sleeves and long pants) to prevent tsetse fly bites.
- Use sleeping nets (mesh nets) for protection during sleep.
- Please carefully look for flies in your car before sitting in it. Many people get infected from fly bites inside the car.
Final Word
Human African Trypanosomiasis, or sleeping sickness, is a parasitic infection (Trypanosoma brucei) transmitted to humans by the bite of a tsetse fly (Glossina genus). There exist two types of parasites, i.e., rhodesiense and gambiense. The disease progresses in 2 stages. In the initial stage, the parasite multiplies and spreads through blood and lymph, while in the 2nd stage, the parasite crosses the blood-brain barrier and affects the CNS. Common symptoms include headaches, recurrent fever, body aches, chancres, psychological disturbances, etc. More than 75% of patients report excessive daytime sleepiness and disturbed sleep-wake cycles. Treatment involves anti-parasitic drugs like fexinidazole, melarsoprol, nifurtimox, and eflornithine combined therapy, etc. If left untreated, the condition can lead to severe consequences like seizures, coma, and even death.
Refrences
- 1Elenga, V. A., Lissom, A., Elion, D. O. A., Vouvoungui, J. C., Djontu, J. C., Boumpoutou, R. K., … & Ntoumi, F. (2022). Risk factors and prevalence of human African trypanosomiasis in individuals living in remote areas of the Republic of Congo. BMC Public Health, 22(1), 2322.
- 2Malvy, D., & Chappuis, F. (2011). Sleeping sickness. Clinical Microbiology and Infection, 17(7), 986-995.
- 3Hope-Rapp, E., Klement, E., Danis, M., Bricaire, F., & Caumes, E. (2009, February). Double trypanosomal chancre revealing West African trypanosomiasis in a Frenchman living in Gabon. In Annales de Dermatologie et de Venereologie (Vol. 136, No. 4, pp. 341-345).
- 4Ezzedine, K., Darie, H., Le Bras, M., & Malvy, D. (2007). Skin features accompanying imported human African trypanosomiasis: hemolymphatic Trypanosoma gambiense infection among two French expatriates with dermatologic manifestations. Journal of Travel Medicine, 14(3), 192-196.
- 5Johnston, V., Stockley, J. M., Dockrell, D., Warrell, D., Bailey, R., Pasvol, G., … & British Infection Society. (2009). Fever in returned travelers presenting in the United Kingdom: recommendations for investigation and initial management. Journal of Infection, 59(1), 1-18.
- 6Kennedy, P. G. (2008). The continuing problem of human African trypanosomiasis (sleeping sickness). Annals of Neurology: Official Journal of the American Neurological Association and the Child Neurology Society, 64(2), 116-126.
- 7Ortiz-Martínez, Y., Kouamé, M. G., Bongomin, F., Lakoh, S., & Henao-Martínez, A. F. (2023). Human African Trypanosomiasis (Sleeping Sickness)—Epidemiology, Clinical Manifestations, Diagnosis, Treatment, and Prevention. Current Tropical Medicine Reports, 10(4), 222-234.
- 8Márquez-Hernández, J. D. (2019). Parasitic arthritis. Infections and the Rheumatic Diseases, 301-314.
- 9Willyard, C. (2011). Putting sleeping sickness to bed. Nature Medicine, 17(1), 14-18.
- 10Tesoriero, C., Del Gallo, F., & Bentivoglio, M. (2019). Sleep and brain infections. Brain Research Bulletin, 145, 59-74.
- 11Kagira, J. M., Maina, N., Njenga, J., Karanja, S. M., Karori, S. M., & Ngotho, J. M. (2011). Prevalence and types of coinfections in sleeping sickness patients in Kenya (2000/2009). Journal of Tropical Medicine, 2011(1), 248914.
- 12Rijo-Ferreira, F., Bjorness, T. E., Cox, K. H., Sonneborn, A., Greene, R. W., & Takahashi, J. S. (2020). Sleeping sickness disrupts the sleep-regulating adenosine system. Journal of Neuroscience, 40(48), 9306-9316.
- 13Kato, C. D., Nanteza, A., Mugasa, C., Edyelu, A., Matovu, E., & Alibu, V. P. (2015). Clinical profiles, disease outcome and co-morbidities among T. b. rhodesiense sleeping sickness patients in Uganda. PloS one, 10(2), e0118370.
- 14Kristensson, K., Nygård, M., Bertini, G., & Bentivoglio, M. (2010). African trypanosome infections of the nervous system: parasite entry and effects on sleep and synaptic functions. Progress in neurobiology, 91(2), 152-171.
- 15Domachowske, J., Suryadevara, M., Domachowske, J., & Suryadevara, M. (2020). African Sleeping Sickness: African Trypanosomiasis. Clinical Infectious Diseases Study Guide: A Problem-Based Approach, 307-311.
- 16World Health Organization. (2023). Trypanosomiasis, human African (sleeping sickness). Retrieved from [https://www.who.int/news-room/fact-sheets/detail/trypanosomiasis-human-african-(sleeping-sickness)](https://www.who.int/news-room/fact-sheets/detail/trypanosomiasis-human-african-(sleeping-sickness))
- 17Lundkvist, G. B., Kristensson, K., & Bentivoglio, M. (2004). Why trypanosomes cause sleeping sickness. Physiology, 19(4), 198-206.
- 18Suárez, C., Nolder, D., García-Mingo, A., Moore, D. A., & Chiodini, P. L. (2022). Diagnosis and clinical management of Chagas disease: An increasing challenge in non-endemic areas. Research and reports in tropical medicine, 13, 25.
- 19Lindner, A. K., Lejon, V., Barrett, M. P., Blumberg, L., Bukachi, S. A., Chancey, R. J., … & Priotto, G. (2024). New WHO guidelines for treating rhodesiense human African trypanosomiasis: expanded indications for fexinidazole and pentamidine. The Lancet Infectious Diseases.
- 20Kuemmerle, A., Schmid, C., Kande, V., Mutombo, W., Ilunga, M., Lumpungu, I., … & Valverde Mordt, O. (2020). Prescription of concomitant medications in patients treated with Nifurtimox Eflornithine Combination Therapy (NECT) for T. b. gambiense second-stage sleeping sickness in the Democratic Republic of the Congo. PLoS Neglected Tropical Diseases, 14(1), e0008028.
- 21Neau, P., Hänel, H., Lameyre, V., Strub-Wourgaft, N., & Kuykens, L. (2020). Innovative partnerships for the elimination of human African trypanosomiasis and the development of fexinidazole. Tropical Medicine and Infectious Disease, 5(1), 17.
- 22Kaba, D., Djohan, V., Berté, D., Ta, B. T. D., Selby, R., Kouadio, K. A. D. M., … & Courtin, F. (2021). Use of vector control to protect people from sleeping sickness in the focus of Bonon (Côte d’Ivoire). PLoS Neglected Tropical Diseases, 15(6), e0009404.

