Maple Syrup Urine Disease (MSUD) is a rare genetic disorder that affects how the body breaks down certain amino acids. Amino acids are the basic building blocks of proteins. This condition occurs because of a deficiency in an enzyme called branched-chain alpha-keto acid dehydrogenase (BCKAD). BCKAD is responsible for breaking down three specific amino acids: Leucine, Isoleucine, and Valine. When these amino acids can’t be processed correctly, harmful substances called Ketoacids build up in the body.
Accumulation of Ketoacids can cause severe neurological problems, potentially leading to coma and even death. In newborns with MSUD, you may notice symptoms like slow growth, delayed developmental milestones, and feeding difficulties. People with this condition also have urine that smells like maple syrup, which is a unique sign of MSUD.1 Blackburn PR, Gass JM, Vairo FPE, et al. Maple syrup urine disease: mechanisms and management. Appl Clin Genet. 2017;10:57-66. Published 2017 Sep 6. doi:10.2147/TACG.S125962
How common is MSUD?
MSUD is a rare genetic condition. It affects 1 in 185,000 infants. It is more common in communities with high rates of cousin marriages. Hence, among Ashkenazi Jews, it affects 1 in 26,000 infants.2Maple Syrup Urine Disease (MSUD) | Children’s Hospital Pittsburgh. Children’s Hospital of Pittsburgh. Published 2020. https://www.chp.edu/our-services/rare-disease-therapy/conditions-we-treat/maple-syrup-urine-disease
Cause of Maple Syrup Urine Disease
Mutations in one of three genes, namely BCKDHA, BCKDHB, or DBT, lead to Maple syrup urine disease. These genes play a role in producing enzymes known as BCKAD complex. MSUD follows an autosomal recessive inheritance pattern; hence, both parents must possess the mutated gene for their child to have MSUD. Everyone has two copies of each gene. A carrier of MSUD is healthy but carries a mutation in one of the two gene copies. When two carrier parents have a child, each pregnancy carries a 25% chance of the child having the disorder. This risk is the same for both males and females. Communities with high rates of consanguineous marriages are more likely to have cases of MSUD. Hence, it is extremely important to screen newborns for the condition. Early diagnosis has been linked with better health outcomes.
What is the BCKAD Enzyme Complex?
The branched-chain alpha-keto acid dehydrogenase is a complex multi-enzyme system consisting of three catalytic components: alpha-ketoacid dehydrogenase (referred to as the E1 component), dihydrolipoyl transacylase (the E2 component), and dihydrolipoamide dehydrogenase (the E3 component). It’s crucial to emphasize that deficiencies in the E3 component can result in a potentially life-threatening accumulation of lactic acid, leading to lactic acidosis.
Types of Maple Syrup Urine Disease
MSUD has five major types. These subtypes differ from each other by severity, age of onset, and level of enzyme activity.
Classic MSUD
People with classic MSUD have less than 2% BCKAD enzymatic activity. These newborns exhibit a maple syrup odor in cerumen shortly after birth and in urine within the first week. Untreated neonates experience irritability, lethargy, poor feeding, and apnea, leading to coma and early death due to brain edema.
In older individuals, increased leucine levels cause epigastric pain, anorexia, vomiting, muscle fatigue, altered consciousness, psychiatric symptoms, and movement issues (ataxia).
Intermediate MSUD
The intermediate form of MSUD has around 30% of BCKAD activity. In the neonatal period, individuals may seem healthy, but their earwax could have a maple syrup odor. In their early years, they might have feeding issues, growth problems, and intellectual disabilities and face neurological symptoms like those in the classic form.3Google Scholar. scholar.google.com. Accessed September 7, 2023. https://scholar.google.com/scholar_lookup?title=The+Metabolic+and+Molecular+Bases+of+Inherited+Disease&author=DT+Chuang&author=VE+Shih&publication_year=2001&
Intermittent MSUD
People with intermittent MSUD typically show no symptoms, maintaining normal growth and neurological development, even with an unrestricted diet. However, they may develop symptoms during increased energy demands on the body, such as during illness.
Thiamine-Responsive
Thiamine-responsive MSUD is an infrequent type linked to genetic mutations in the DBT gene. People affected by this condition display symptoms similar to the intermediate form and typically need a treatment regimen that involves both dietary restrictions on BCAAs and thiamine (Vit B1) supplementation.
E3 Deficient MSUD
E3-deficiency MSUD is accompanied by lactic acidosis. It is also referred to as MSUD type III and exhibits a combination of deficiencies in keto acid dehydrogenases. Lactic acidosis can lead to severe irregular breathing, muscle weakness (hypotonia), nausea, vomiting, and heart rate abnormalities. It is also characterized by poor growth (failure to thrive) and a combined form of metabolic acidosis, including increased levels of lactic and pyruvic acid in the bloodstream, as well as organic aciduria. Notably, this specific type of MSUD may potentially benefit from lipoic acid supplementation.4 Maple Syrup Urine Disease – an overview | ScienceDirect Topics. www.sciencedirect.com. Accessed September 11, 2023. https://www.sciencedirect.com/topics/medicine-and-dentistry/maple-syrup-urine-disease#:~:text=Finally%2C%20E3%2Ddeficiency%20MSUD%20with
Symptoms of Maple Syrup Urine Disease
Newborns typically first start showing symptoms of MSUD within the first 48 hours of birth. However, In older children, signs of intermediate, intermittent, and thiamine-responsive MSUD usually emerge before age seven. By the end of the first week of extrauterine life, the following clinical signs become evident:
- The infant fails to take feed and vomits.
- The infant has poor muscle tone.
- The patient may exhibit lethargy and experience convulsive seizures.
- This may lead to extensive brain damage leading to mental retardation.
- Death by the end of the first year of life without treatment.
- Increased levels of branched-chain amino acids and their corresponding alpha-keto acids in the blood and urine.
- A characteristic odor resembling that of maple syrup or burnt sugar in the urine.
What is a Metabolic Crises?
MSUD can also predispose patients to metabolic crises. Metabolic crises are caused by low blood sugar and the build-up of toxic substances in the blood. Symptoms of a metabolic crisis include poor appetite, nausea, vomiting, diarrhea, extreme sleepiness, irritable mood, and behavior changes. If left untreated, it can lead to breathing problems, seizures, coma, and sometimes even death. Treatment requires the removal of toxic substances and the management of blood glucose levels.
People with certain metabolic disorders (such as some fatty acid oxidation disorders, amino acid disorders, and organic acid disorders) experience metabolic crises more frequently. These crises often result from triggers such as illness or infection, prolonged periods without food, and, in some instances, strenuous exercise.5Metabolic crisis – newbornscreening.info. https://www.newbornscreening.info/glossary/metabolic-crisis/#:~:text=This%20is%20a%20serious%20health
How do you test for Maple Syrup Urine Disease?
MSUD can be tested by a variety of techniques.6 Philadelphia TCH of. Maple Syrup Urine Disease (MSUD). www.chop.edu. Published April 14, 2022. https://www.chop.edu/conditions-diseases/maple-syrup-urine-disease-msud#:~:text=Most%20infants%20with%20MSUD%20are For instance, newborns can undergo screening through a blood test, where a small blood sample is typically taken from the baby’s heel shortly after birth. This blood sample is then analyzed for elevated levels of specific amino acids, such as leucine, isoleucine, and valine, which can indicate the presence of the disease. Other tests include:
Urine Analysis:
Healthcare professionals typically collect a midstream urine sample to check for the presence of specific metabolites, including alloisoleucine, a particular amino acid that accumulates in the urine of individuals with MSUD. FeCl3 test with urine gives a blue color in MSUD.
Plasma Amino Acid Analysis:
A blood sample may be taken to measure the levels of amino acids in the bloodstream, particularly the branched-chain amino acids (leucine, isoleucine, and valine).
Genetic Testing:
Genetic testing can confirm the diagnosis of MSUD by identifying mutations in the genes responsible for the condition. There are several genes associated with MSUD, including the BCKDHA, BCKDHB, and DBT genes. Identifying specific mutations can help understand the condition’s severity and potential treatment options.
Role of Tandem Mass Spectrometry in MSUD
Tandem mass spectrometry (MS/MS) examines the Fisher ratio and concentrations of leucine-isoleucine. Elevated branched-chain amino acid detection in this test warrants additional laboratory studies. This test can detect classic MSUD; however, it may not detect milder forms of MSUD due to normal leucine levels.
MS/MS cannot distinguish amino acids with the same mass, such as hydroxyproline, leucine, isoleucine, and allo-isoleucine. To remedy this, second-tier testing is performed. This includes liquid chromatography to analyze allo-isoleucine on dried blood spots.
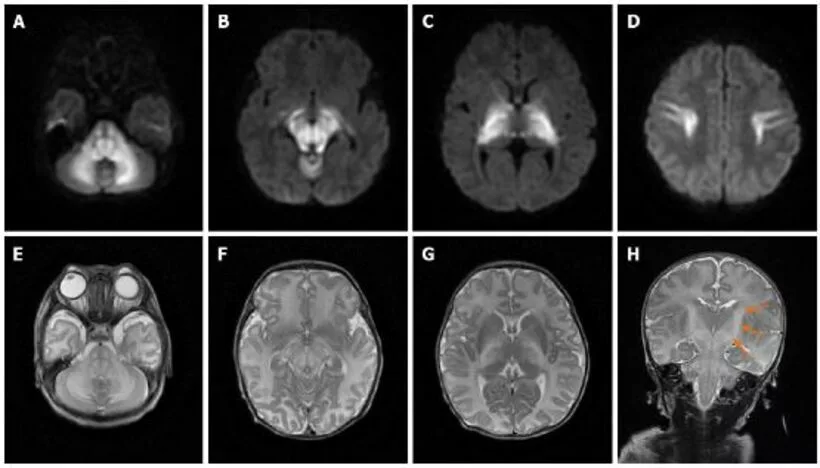
Additional laboratory studies include the Dinitrophenylhydrazine test(DNPH test) and Gas Chromatography testing. The DNPH test can detect alpha-keto acids in urine. Gas chromatography can also test for branched-chain amino acids. Imaging studies can be done to follow up on complications from the disease. For example, MRIs can show MSUD edema or lesions affecting the white matter.7Li Y, Liu X, Duan CF, Song XF, Zhuang XH. Brain magnetic resonance imaging findings and radiologic review of maple syrup urine disease: Report of three cases. World J Clin Cases. 2021;9(8):1844-1852. doi:10.12998/wjcc.v9.i8.1844
Treatment of Maple Syrup Urine Disease
MSUD management requires managing amino acid levels and preventing and treating metabolic crises.
Healthcare providers manage amino acid levels by constantly monitoring them. To ensure that levels do not exceed the patient’s tolerance, a specialized diet is initiated. This strict diet provides essential nutrients while restricting the intake of these three amino acids. Additionally, Thiamine-responsive MSUD will need B1 supplementation along with a strict diet.
Patients with the condition usually require a multi-disciplinary team to assist them in navigating the different complications that arise from the condition. These can involve physiotherapists, Speech-language therapists, and counselors. These experts can help with mobility issues, speech delays, and psychological conditions like depression and anxiety respectively.
Finally, patients with liver transplants can overcome MSUD, as the new liver can produce the enzymes that are lacking in the patient. These patients can then enjoy a normal diet and avoid other problems associated with MSUD progression. However, they can still pass on the gene for the disease.
How to Manage Metabolic Crises?
MSUD patients must be immediately hospitalized when they become ill or when their amino acid levels become dangerously high. These conditions can increase the chance of the patient experiencing a metabolic crisis. They need immediate stabilization of circulation, airway, and breathing. Management often involves IV glucose and insulin administration to reduce amino acid levels. In severe cases, dialysis may be required to remove toxic substances from the blood. Continuous monitoring is essential to prevent complications and ensure recovery.
Complications of Maple Syrup Urine Disease
Undiagnosed or untreated MSUD can be fatal and may lead to metabolic crises. Metabolic crises occur due to sudden increases in branched-chain amino acids. They can result in severe physical and neurological deficits. Metabolic crises can even occur in patients currently undergoing treatment. A metabolic crisis is signaled by the emergence of clinical manifestations, such as profound fatigue, heightened irritability, episodes of vomiting, and a diminished state of alertness. Other complications of untreated MSUD are8Hassan SA, Gupta V. Maple Syrup Urine Disease. PubMed. Published 2022. https://www.ncbi.nlm.nih.gov/books/NBK557773/#:~:text=Maple%20syrup%20urine%20disease%20is
- Seizures
- Metabolic acidosis
- Swelling of the brain
- Reduced blood flow to the brain
- Cognitive impairments
- Vision impairment
- Muscle stiffness
- Permanent neurological damage
- Weakened bones (Osteoporosis)
- Acute pancreatic inflammation
- High plasma leucine levels cause T-cell suppression, leading to repeated candidiasis in the esophagus.
- Inadequate essential amino acids result in anemia, hair loss, stunted growth, and skin inflammation.
Prognosis of Maple Syrup Urine Disease
A good prognosis for MSUD depends on prompt diagnosis and treatment. However, delayed onset of classic MSUD by 7 to 14 days can result in significant learning impairment and cerebral palsy.9Strauss KA, Puffenberger EG, Carson VJ. Maple Syrup Urine Disease. In: Adam MP, Mirzaa GM, Pagon RA, et al., eds. GeneReviews®. Seattle (WA): University of Washington, Seattle; January 30, 2006. Around 61% of adult MSUD patients live independently and integrate into society, but 56% still require psychological and psychiatric care.10Abi-Wardé MT, Roda C, Arnoux JB, et al. Long-term metabolic follow-up and clinical outcome of 35 patients with maple syrup urine disease. J Inherit Metab Dis. 2017;40(6):783-792. doi:10.1007/s10545-017-0083-x
Life Expectancy with Maple Syrup Disease
The life expectancy of patients suffering from MSUD depends on the age of diagnosis, the severity of the condition, and conformity to the specialized diet provided. Patients with well-managed MSUD can have a normal lifespan. Specialized dietary supplementation can benefit patients both in their nutrition and quality of life.11le Roux C, Murphy E, Lilburn M, Lee PJ. The longest-surviving patient with classical maple syrup urine disease. Journal of Inherited Metabolic Disease. 2006;29(1):190-194. doi:https://doi.org/10.1007/s10545-006-0204-4
Conclusion
In summary, Maple Syrup Urine Disease (MSUD) is a rare genetic disorder that affects amino acid metabolism, leading to severe neurological problems. There are five subtypes, and early diagnosis and management are crucial for a normal lifespan. Treatment involves dietary control and, in some cases, liver transplantation.
Refrences
- 1Blackburn PR, Gass JM, Vairo FPE, et al. Maple syrup urine disease: mechanisms and management. Appl Clin Genet. 2017;10:57-66. Published 2017 Sep 6. doi:10.2147/TACG.S125962
- 2Maple Syrup Urine Disease (MSUD) | Children’s Hospital Pittsburgh. Children’s Hospital of Pittsburgh. Published 2020. https://www.chp.edu/our-services/rare-disease-therapy/conditions-we-treat/maple-syrup-urine-disease
- 3Google Scholar. scholar.google.com. Accessed September 7, 2023. https://scholar.google.com/scholar_lookup?title=The+Metabolic+and+Molecular+Bases+of+Inherited+Disease&author=DT+Chuang&author=VE+Shih&publication_year=2001&
- 4Maple Syrup Urine Disease – an overview | ScienceDirect Topics. www.sciencedirect.com. Accessed September 11, 2023. https://www.sciencedirect.com/topics/medicine-and-dentistry/maple-syrup-urine-disease#:~:text=Finally%2C%20E3%2Ddeficiency%20MSUD%20with
- 5Metabolic crisis – newbornscreening.info. https://www.newbornscreening.info/glossary/metabolic-crisis/#:~:text=This%20is%20a%20serious%20health
- 6Philadelphia TCH of. Maple Syrup Urine Disease (MSUD). www.chop.edu. Published April 14, 2022. https://www.chop.edu/conditions-diseases/maple-syrup-urine-disease-msud#:~:text=Most%20infants%20with%20MSUD%20are
- 7Li Y, Liu X, Duan CF, Song XF, Zhuang XH. Brain magnetic resonance imaging findings and radiologic review of maple syrup urine disease: Report of three cases. World J Clin Cases. 2021;9(8):1844-1852. doi:10.12998/wjcc.v9.i8.1844
- 8Hassan SA, Gupta V. Maple Syrup Urine Disease. PubMed. Published 2022. https://www.ncbi.nlm.nih.gov/books/NBK557773/#:~:text=Maple%20syrup%20urine%20disease%20is
- 9Strauss KA, Puffenberger EG, Carson VJ. Maple Syrup Urine Disease. In: Adam MP, Mirzaa GM, Pagon RA, et al., eds. GeneReviews®. Seattle (WA): University of Washington, Seattle; January 30, 2006.
- 10Abi-Wardé MT, Roda C, Arnoux JB, et al. Long-term metabolic follow-up and clinical outcome of 35 patients with maple syrup urine disease. J Inherit Metab Dis. 2017;40(6):783-792. doi:10.1007/s10545-017-0083-x
- 11le Roux C, Murphy E, Lilburn M, Lee PJ. The longest-surviving patient with classical maple syrup urine disease. Journal of Inherited Metabolic Disease. 2006;29(1):190-194. doi:https://doi.org/10.1007/s10545-006-0204-4

