Churg-Strauss Syndrome (Eosinophilic Granulomatosis with Polyangiitis) is a rare but serious multisystem vasculitis characterized by inflammation of small- and medium-sized arteries. It is most commonly associated with a history of adult-onset asthma, allergic rhinitis, nasal polyps, and prominent eosinophilia in blood and tissues. This autoimmune disorder can lead to significant organ damage if not diagnosed and treated promptly.
What is Churg-Strauss Syndrome?
The syndrome involves eosinophil-rich inflammation and granuloma formation, primarily affecting the lungs, skin, and peripheral nervous system, but it can involve nearly any organ system, including the cardiovascular, gastrointestinal, renal, and central nervous systems. The vasculitis may be difficult to detect histologically, especially if biopsies are performed after immunosuppressive therapy or from inaccessible locations.
Pathophysiologically, EGPA is classified as a vasculitis of small- and medium-sized arteries. It involves immune activation that leads to vessel wall inflammation, tissue destruction, and granuloma formation—clusters of macrophages (epithelioid cells) and inflammatory debris.1.Greco, A., Rizzo, M. I., De , A., Gallo, A., Fusconi, M., Ruoppolo, G., Altissimi, G., & De Vincentiis, M. (2015). Churg–Strauss syndrome. Autoimmunity Reviews, 14(4), 341–348.
Churg-Strauss syndrome mimics other types of blood vessel inflammation. However, adult-onset asthma, recurring sinus infections, and significantly elevated eosinophil levels set it apart from them.
Is it common?
Fortunately, it is rare and affects only 1-3 people out of every million.2Keogh, K. A., & Specks, U. (2006). Churg-Strauss syndrome. Seminars in Respiratory and Critical Care Medicine, 27(2), 148–157. https://doi.org/10.1055/s-2006-939518. As reported, it usually manifests in the age group of 35-55 years. That said, clinicians have observed cases at both extremes of age as well, from as young as 4 to as old as 74. Males and females exhibit similar gender prevalences.
Cause of Churg-Strauss Syndrome
The cause of the disease is yet unclear. However, research suggests that the reason for an exaggerated immune response might be an interplay of environmental factors (i.e., allergens) and some genes. Strong association of HLA-DQ and HLA-DRB4 3with the presence of the disease strengthens that theory.Vaglio, A., Martorana, D., Maggiore, U., Grasselli, C., Zanetti, A., Pesci, A., Garini, G., Manganelli, P., Bottero, P., Tumiati, B., Sinico, R. A., et al. (2007). HLA–DRB4 as a genetic risk factor for Churg-Strauss syndrome. Arthritis & Rheumatism, 56(9), 3159–3166.
Furthermore, in already prone patients, some medications like leukotriene-modifying agents (like Montelukast) seem to trigger and speed up the process.
Mechanism of the Disease
The basic mechanism is a malfunctioned immune system. It perceives the body’s own cells as aliens and destroys them. Although the exact mechanism is unknown, eosinophils, T-helper 2 (Th2) cells, and antineutrophil cytoplasmic antibodies (ANCA) are thought to be important participants.4Sablé-Fourtassou, R., Cohen, P., Mahr, A., Pagnoux, C., Mouthon, L., Jayne, D., Blockmans, D., et al. (2005). Antineutrophil cytoplasmic antibodies and the Churg–Strauss syndrome. Annals of Internal Medicine, 143(9), 632–638. ANCA targets monocytes and neutrophils, while eosinophils release toxins such as major basic protein that cause cell damage.
Symptoms of Churg-Strauss Syndrome
The hallmark symptoms of Churg-Strauss syndrome form a classic triad.
Triad of Churg-Strauss Syndrome:
In medicine, a triad means a group of three symptoms that frequently co-exist. Here, the triad consists of:
- Asthma: It is the hallmark of the disease. Nearly every patient has it.
- Eosinophilia: Increased number of eosinophils (an immune cell type) in the plasma.
- Vasculitis: Blood vessel inflammation and potential necrosis in severe cases.
Other than these, symptoms may include:
- Body aches and fatigue
- Loss of appetite leading to weight loss
- Abdominal pain and bleeding
- Muscular and joint pain
- Pain, numbness, and tingling sensations in hands and feet
- Ulcers and rashes on limbs
This disease occurs in 3 stages, with the first stage manifesting as a mild illness that gradually progresses to worse symptoms.
Stages of Disease
Stage 1: (Asthmatic Phase):
It starts as long-standing adult-onset asthma with or without nasal polyps, sinus infections, and flu-like symptoms. Asthma is persistent, and medicines do not seem to be effective. Since these symptoms are common, diagnosis is often delayed at this stage.
Stage 2: ( Eosinophilic Phase):
It is the stage of elevated eosinophils. Sometimes, their level can go as high as 10%. These eosinophils invade organs such as the lungs, digestive tract, and heart. Consequently, patients may develop pneumonia or gastroenteritis and present with fever, cough, shortness of breath, abdominal pain, or diarrhea.
Stage 3: (Vascular Damage Phase):
Finally, widespread vascular damage initiates. At the start, it manifests as a few swollen, leaky blood vessels. With time, it may even lead to full-fledged damage to the vessel lumen. Vascular inflammation is often accompanied by granuloma formation. Common signs of this stage include:
- Nerve damage – causing pain, tingling, and numbness. Foot drop may also occur.
- Palpable skin spots
- Kidney injury or nephropathy
- Serious heart complications
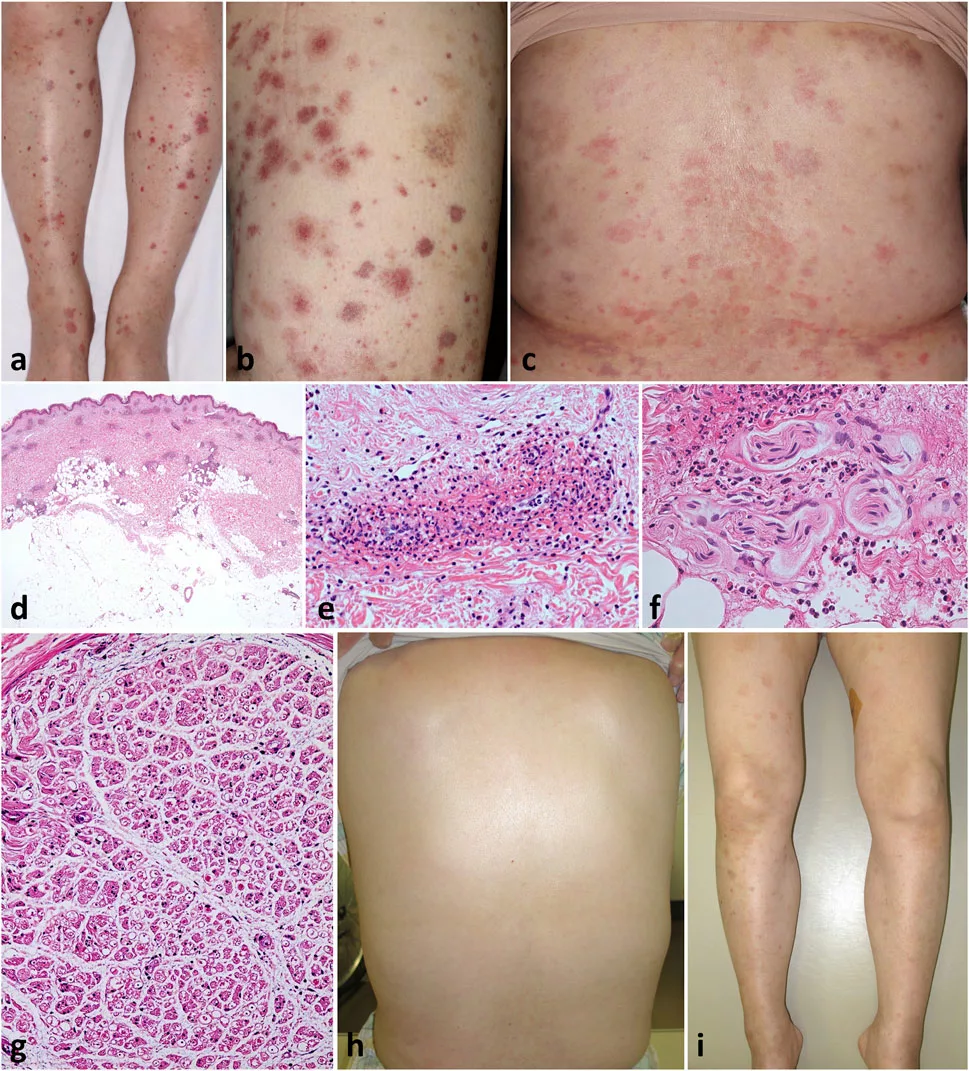
Image reproduced from Kawate K, et al. J Cutan Immunol Allergy. 2024;7. available via Frontiers under license CC BY.
Differential Diagnosis of Churg-Strauss Syndrome
This disorder can look like other ANCA-mediated vascular disorders, such as:
- Granulomatosis with Polyangitis
- Microscopic Polyangitis
- Wegener Granulomatosis
Or hyperesosniophlic conditions like:
- Allergic Bronchopulmonary Aspergillosis
- Hypereosinophilic Syndrome
Churg-Strauss Syndrome vs Wegener’s Granulomatosis
Amongst all disorders mentioned above, distinguishing Churg-Strauss syndrome from Wegener’s Granulomatosis is most challenging. Both of them target the blood vessels and the lungs mainly. However, certain features help to distinguish it from Wegener’s granulomatosis.
| Churg-Strauss syndrome | Wegener’s granulomatosis |
| Marked eosinophilia | Slightly raised eosinophils |
| History of asthma | No history of asthma |
| Lung involvement is predominant | Kidney involvement is predominant |
| p-ANCA positivity | c-ANCA positivity |
Diagnosis of Churg-Strauss Syndrome
The workup for disease aims to exclude other conditions and then evaluate the extent of organ involvement.
In 2022, the American College of Rheumatology (ACR) established the criteria to diagnose the disease. According to that, the presence of at least 4 out of the following 6 clinical and laboratory features is mandatory to label the disease as Churg-Strauss syndrome.5Baldini, C., Talarico, R., Della Rossa, A., & Bombardieri, S. (2010). Clinical manifestations and treatment of Churg–Strauss syndrome. Rheumatic Disease Clinics of North America, 36(3), 527–543. These include:
- Asthma
- Migratory pulmonary infiltrates
- Paranasal sinus abnormalities
- Single or multiple nerve involvement
- Peripheral blood eosinophilia (>10% of total leukocyte count)
- Eosinophilic infiltration in tissue biopsy
These criteria demonstrated a high diagnostic accuracy, with a specificity of 99.7% and a sensitivity of 85%.
Blood Tests:
These include:
Complete Blood Count
This test tells the number of all cells present in the blood. Normal eosinophil level is 1-4%. If it exceeds 10%, it is a key clue for the diagnosis. However, it doesn’t confirm the presence of disease. This is because raised eosinophils can also be present in asthma, parasitic infection, cancer or as a result of the reaction to some drugs.
ANCA Testing
30-40% of patients show the presence of p-ANCA antibodies in plasma.
ESR & CRP
Inflammatory markers like ESR and CRP tend to be significantly raised in disease.
IgE
This antibody is seen in most cases of allergic conditions..
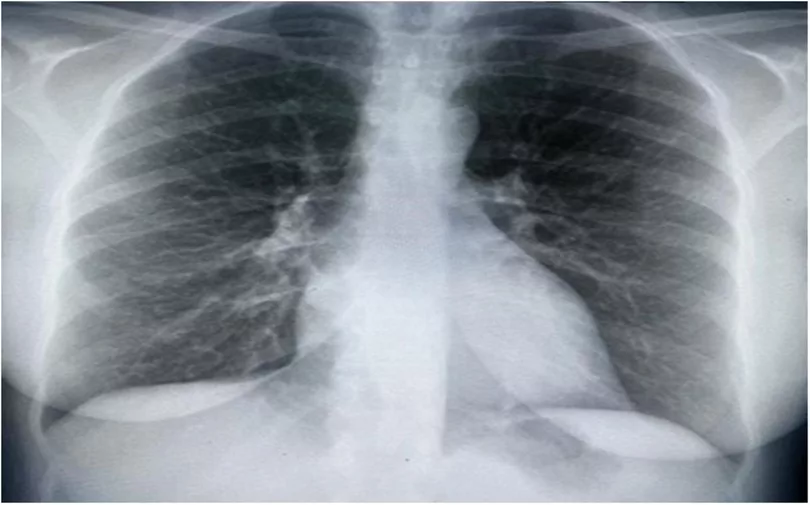
Imaging Tests:
These include:
Chest X-rays or high-resolution CT scans show lung infiltrates or pleural effusions. Nodular opacities suggestive of granuloma are also visible in severe cases. In addition, A CT scan of the paranasal sinuses (CT-PNS) may reveal sinusitis or nasal polyps.
Biopsy:
An excised part of the affected tissue (skin, lung, nerve, or gut), when visualised under the microscope, can confirm the diagnosis by showing vascular injury, eosinophils or granulomatous inflammation.6Katzenstein, A.-L. A. (2000). Diagnostic features and differential diagnosis of Churg–Strauss syndrome in the lung: A review. American Journal of Clinical Pathology, 114(5), 767–772
Nerve & Organ-Specific Tests:
- Electromyography (EMG) and nerve conduction studies help detect nerve damage like mononeuritis multiplex in patients who report neuropathy.
- Echocardiograms and cardiac MRI to check heart involvement
- Renal function tests and Urine Examination help spot kidney injury, especially in ANCA-positive cases.
Treatment of Churg-Strauss Syndrome
Unfortunately, we don’t have a cure for Churg-Strauss syndrome. But some medicines may help to reduce symptoms. The main goal is to control symptoms and organ damage and improve the quality of life. Treatment is not the same for everyone. It depends on how bad the disease is and on the patient’s general health profile.
Corticosteroids:
Systemic corticosteroids remain first-line.7Churg, A., Brallas, M., Cronin, S. R., & Churg, J. (1995). Formes frustes of Churg–Strauss syndrome. Chest, 108(2), 320–323. Prednisolone, Fludrocortisone, and high-potency steroids are of great help to suppress the inflammation. At first, doctors usually prescribe a higher dose. Then, after a few weeks, they slowly taper off the dose. It is because the long-term use of steroids can lead to low bone mass, obesity, and high blood sugar levels.
Immuno-Suppressive Therapy:
In severe cases, steroids alone are not sufficient. Hence, physicians prescribe immunosuppressive agents. They include Azathioprine, Cyclophosphamide,Methotrexate or Infliximab.8Hellmich, B., & Gross, W. L. (2005). Recent progress in the pharmacotherapy of Churg–Strauss syndrome. Expert Opinion on Pharmacotherapy, 5(1), 25–35. In some cases where the patient showed intolerance to them, Mycophenolate mofetil showed good results as an alternate option. These drugs disturb the immune system. Therefore, close monitoring with routine blood chemistry is essential to prevent their side effects.
Biological Treatments:
For relapsing cases, biological agents may help. According to studies, Mepolizumab, an anti-IL-5 monoclonal antibody, showed a significant reduction in cases that showed predominant eosinophilic inflammation. Similarly, in ANCA-positive patients who had systemic vasculitis, an anti-CD20 monoclonal antibody, Rituximab, was proven to be quite beneficial.
Monitoring & Long-term Care:
Relapse rates in Churg-Strauss syndrome are substantial. Nearly 25-50% of patients may experience it, especially during the tapering of the dose. Hence, regular monitoring of eosinophils, ANCA, and evaluations of organs is mandatory.
Prognosis of Churg-Strauss Syndrome
Thanks to new diagnostic modalities and better immunosuppressive therapies, the outlook for Churg-Strauss syndrome has improved significantly. Before corticosteroids, EGPA was often fatal. Now, according to research, the 5-year survival rate has reached over 85–90%. The outcomes are even better in patients without major organ damage.
The Five-Factor Score (FFS) is a validated prognostic tool that helps predict outcomes and guide treatment. These include:
- Age over 65 years
- Gastrointestinal involvement (bleeding or ischemia)
- Renal insufficiency (creatinine >1.58 mg/dL)
- Cardiac involvement
- Absence of ENT involvement (suggesting more systemic disease)
Each of them indicates a worse prognosis. Even an FFS ≥ 1 signals higher risk and supports the use of more aggressive immunosuppressive therapy.
Complications of Churg-Strauss Syndrome
While treatment outcomes are generally favourable, the syndrome can lead to irreversible organ damage when diagnosis or management is delayed. These include:
Cardiac Complication:
High eosinophilic infiltration leads to inflammation of the heart walls (myocarditis) and lining (pericarditis) or damage to coronary vessels. In addition, arrhythmia and heart failure can also occur. This is observed mostly in ANCA-negative patients.
Renal Complications:
The disease damages the filtration process of the kidney. Damage to the glomerulus causes the leaking of protein in the urine. Subsequently, renal insufficiency occurs after some time. ANCA-positive patients are mainly at risk for it.
Lung Complications:
Chronic inflammation results in pulmonary infiltrates, mass formation, difficult-to-control asthma, and pleural effusion. In rare cases, pulmonary fibrosis and bronchiectasis may also be seen. A drastic lung complication is alveolar haemorrhage. In this case, the patient presents with hemoptysis, anaemia, dyspnea, and hypoxemia. It is fatal and needs prompt care.
Neurological Complication:
About 60-70% of patients experience peripheral neuropathy. Mononeuritis multiplex is the hallmark presentation. The patient may present with sensory and motor deficits like numbness, low or absent sensations, and wrist/foot drop. Rarely, damage to brain vessels can cause seizures, encephalopathy, or brain haemorrhage.
When to see a doctor?
If you are experiencing facial pain with chronic asthma and/or multiple recurring episodes of sinus infections that don’t go away with medications, go to your doctor right away.
Conclusion:
Churg-Strauss syndrome or Eosinophilic granulomatosis with polyantitis(EGPA) is a feared complication of asthma. The main culprits of the disease are eosinophils and antibodies, mainly ANCA. The disease causes widespread inflammation in the body, with the main targets being blood vessels and lungs. Doctors diagnose the disease by clinical findings, blood, and imaging tests. Pulse doses of intravenous corticosteroids and cytotoxic drugs are beneficial to suppress the symptoms and prolong life.
Refrences
- 1.Greco, A., Rizzo, M. I., De , A., Gallo, A., Fusconi, M., Ruoppolo, G., Altissimi, G., & De Vincentiis, M. (2015). Churg–Strauss syndrome. Autoimmunity Reviews, 14(4), 341–348.
- 2Keogh, K. A., & Specks, U. (2006). Churg-Strauss syndrome. Seminars in Respiratory and Critical Care Medicine, 27(2), 148–157. https://doi.org/10.1055/s-2006-939518
- 3with the presence of the disease strengthens that theory.Vaglio, A., Martorana, D., Maggiore, U., Grasselli, C., Zanetti, A., Pesci, A., Garini, G., Manganelli, P., Bottero, P., Tumiati, B., Sinico, R. A., et al. (2007). HLA–DRB4 as a genetic risk factor for Churg-Strauss syndrome. Arthritis & Rheumatism, 56(9), 3159–3166.
- 4Sablé-Fourtassou, R., Cohen, P., Mahr, A., Pagnoux, C., Mouthon, L., Jayne, D., Blockmans, D., et al. (2005). Antineutrophil cytoplasmic antibodies and the Churg–Strauss syndrome. Annals of Internal Medicine, 143(9), 632–638.
- 5Baldini, C., Talarico, R., Della Rossa, A., & Bombardieri, S. (2010). Clinical manifestations and treatment of Churg–Strauss syndrome. Rheumatic Disease Clinics of North America, 36(3), 527–543.
- 6Katzenstein, A.-L. A. (2000). Diagnostic features and differential diagnosis of Churg–Strauss syndrome in the lung: A review. American Journal of Clinical Pathology, 114(5), 767–772
- 7Churg, A., Brallas, M., Cronin, S. R., & Churg, J. (1995). Formes frustes of Churg–Strauss syndrome. Chest, 108(2), 320–323.
- 8Hellmich, B., & Gross, W. L. (2005). Recent progress in the pharmacotherapy of Churg–Strauss syndrome. Expert Opinion on Pharmacotherapy, 5(1), 25–35.

