What is Morbid Obesity?
Morbid Obesity, also known as Class III obesity, is a severe chronic condition characterized by:
- A body mass index (BMI) higher than 40.
- A body mass index greater than 35, accompanied by at least one severe obesity-related health issue.
- A body weight that exceeds 100 pounds above the recommended ideal body weight.
According to the Centers for Disease Control and Prevention (CDC), Morbid obesity affects more than 9% of adults in the U.S.1Centers for Disease Control and Prevention. (n.d.). Adult obesity facts. https://www.cdc.gov/obesity/data/adult.html It typically results from an increased caloric intake, leading to the excessive accumulation of fats in the body.
This excess fat contributes to obesity, affecting nearly every system in the body, including the cardiovascular, gastrointestinal, endocrine, respiratory, genitourinary, and musculoskeletal systems. Additionally, morbid obesity can lead to Obesity Hypoventilation Syndrome, a condition characterized by impaired breathing due to excessive weight.
You can prevent obesity by adopting a healthy lifestyle, maintaining a balanced diet, avoiding prolonged periods of inactivity, and engaging in physical activities such as walking, swimming, jogging, and regular exercise. In cases of severe morbid obesity, surgical options are also available as a potential choice.

What causes Morbid Obesity?
Morbid obesity is primarily attributed to an imbalance in calorie management within the body. This condition arises from two main factors: an increased caloric intake and insufficient calorie expenditure. Here’s a breakdown of how these factors contribute to morbid obesity:
Excessive Caloric Intake
Morbid obesity often occurs when an individual consumes more calories than their body requires. This surplus of calories is obtained through dietary intake.
Reduced Calorie Utilization
Equally significant is the inadequate utilization of calories. The body expends calories during daily activities, exercise, work, or even while at rest or asleep. When the rate at which calories are burned is lower than at which they are consumed, the body accumulates excess calories.
As a consequence of this calorie imbalance, the body stores these excess calories as fat. Over time, the accumulation of excessive fat leads to morbid obesity. Genetic factors also exert considerable influence on the development of morbid obesity. Additionally, metabolic issues and certain medications, like antidepressants, can contribute to this condition. Some other factors are:
- Hypothyroidism
- Eating Disorders
- Cushing syndrome
- Polycystic ovaries
- Sedentary lifestyle
- Stress, anxiety
- Smoking
Diagnostic Criteria for Morbid Obesity
Several criteria and assessments are used to diagnose morbid obesity. These criteria are based on body mass index (BMI), medical history, and clinical evaluations. The following assessment helps in diagnosing Obesity:
Clinical Evaluation
During a clinical examination, the following parameters are considered:
- General weight assessment, including weight trends.
- Blood pressure and heart rate measurements.
Medical History
Inquiries about a patient’s history often include:
- Weight changes (gain or loss).
- Dietary habits.
- Family history of obesity or related conditions.
Systemic Examination
A comprehensive examination of various body systems, such as the cardiovascular, pulmonary, gastrointestinal, and neurovascular systems, helps identify any disorders associated with morbid obesity.
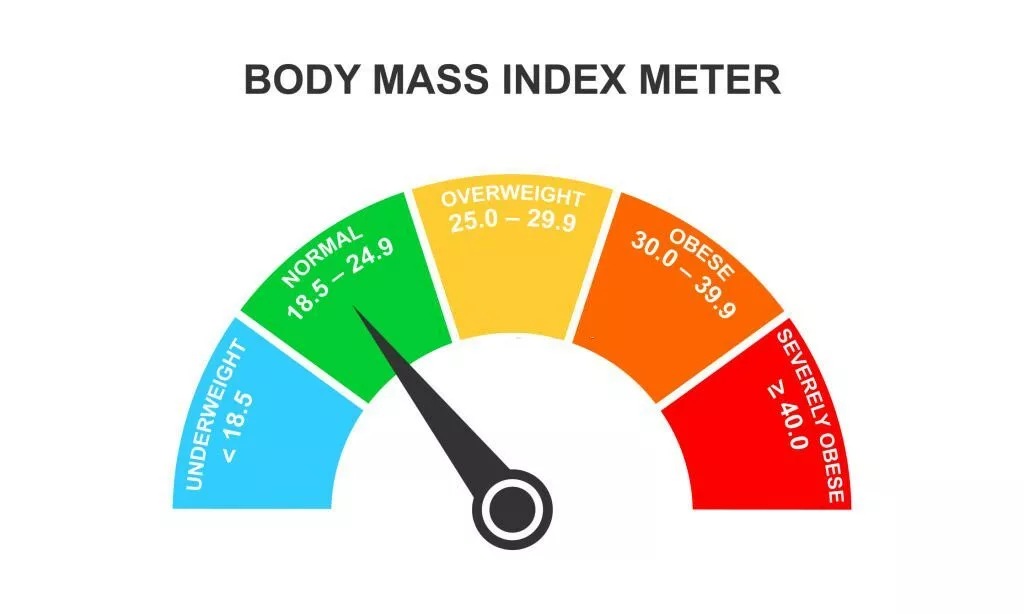
Body Mass Index (BMI) Criteria For Obesity
The Body Mass Index (BMI) is a screening tool that assesses the relationship between your body weight and height to estimate body fat levels in both males and females.
You can calculate your BMI by dividing your body weight in kilograms by the square of your height in meters.
According to the World Health Organization, people are classified into the following categories according to Body mass index (BMI) criteria:2Purnell, J. Q. (2023, May 4). Definitions, Classification, and Epidemiology of Obesity. Endotext – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK279167/#
- Severely underweight – BMI less than 16.5kg/m^2
- Underweight – BMI below 18.5 kg/m^2
- Normal body weight – BMI greater than or equal to 18.5 to 24.9 kg/m^2
- Overweight – BMI greater than or equal to 25 to 29.9 kg/m^2
- Obesity class I – BMI 30 to 34.9 kg/m^2
- Obesity class II – BMI 35 to 39.9 kg/m^2
- Obesity class III – BMI greater than or equal to 40 kg/m^2 (it’s also called severe, morbid, extreme, or massive obesity)
Waist Circumference
Measuring waist circumference provides insight into visceral and abdominal fat accumulation. Abdominal obesity is often associated with morbid obesity, and criteria may vary, but in general, a waist circumference greater than 88 cm in females and 102 cm in males is indicative of abdominal obesity.3Lean, M. E., Han, T. S., & Morrison, C. E. (1995). Waist circumference as a measure for indicating the need for weight management. BMJ (Clinical research ed.), 311(6998), 158–161. https://doi.org/10.1136/bmj.311.6998.158.

Advanced Imaging
In some cases, dual-energy X-ray absorptiometry (DEXA) scans are used to assess regional fat distribution, especially when traditional methods like anthropometry or BMI may not provide sufficient information. DEXA scans help identify fat distribution patterns, which can offer insights into the risk of cardiovascular diseases.
Complications Of Morbid Obesity
Morbid obesity leads to many complications because obesity affects almost every system of your body. Its complications include:
Pulmonary Complications
Morbid obesity causes pulmonary Complications like:
- Obstructive sleep apnea
- Asthma
- Obesity hypoventilation syndrome
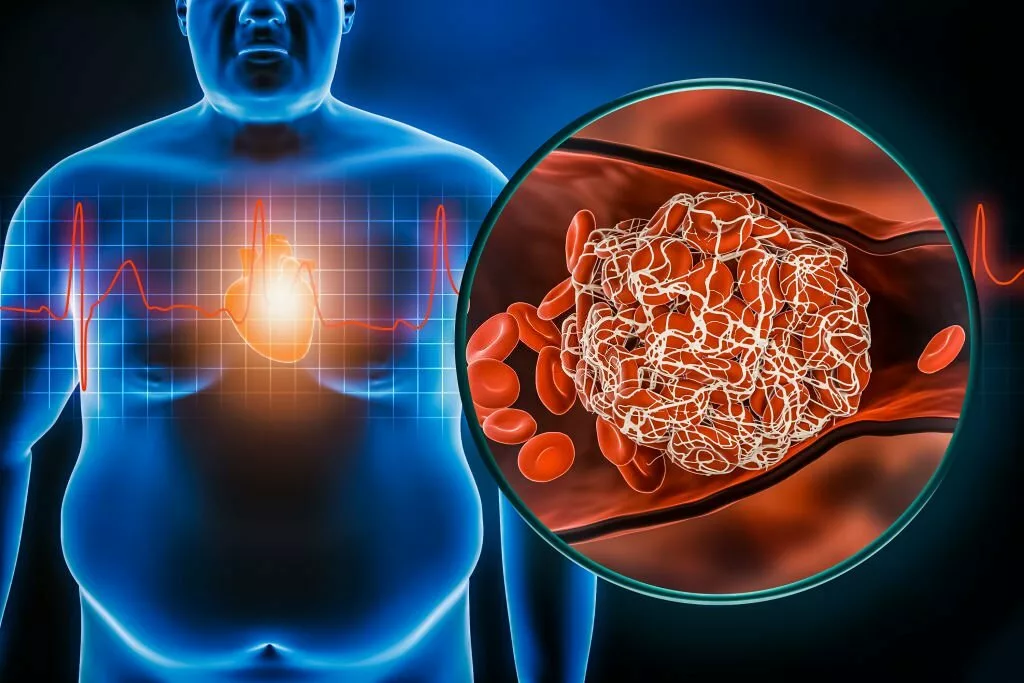
Cardiac Complications
Cardiac complications of morbid obesity are:
- Atherosclerosis
- High blood pressure
- Myocardial infarction
- Heart failure
- Coronary artery disease
Musculoskeletal Problems
Morbid obesity causes musculoskeletal abnormalities like:
- Chronic back pain
- Joint dislocation
- Disc herniation
Moreover, it can also cause degeneration of the knee and hip joint.
Endocrine Abnormalities
Endocrine disorders also commonly occur in morbidly obese individuals. Some of these disorders include:
- Diabetes
- Hyperlipidemia
- Hypercholesterolemia
- Hirsutism
Moreover, diabetes causes many complications, like diabetic foot, neuropathy, nephropathy, and retinopathy.
Gastrointestinal Tract Disorders
Morbid obesity causes gastrointestinal tract disorders like:
- Gastro-esophagal reflux disease (GERD)
- Fatty liver
- Hernias
Obesity also increases the risk of cancers.4Centers for Disease Control and Prevention. (n.d.). Obesity and Cancer. Retrieved from https://www.cdc.gov/cancer/obesity/index.htm
Life Expectancy
Morbid obesity reduces life expectancy. As a result, obese people have a life span that is 10-15 years less than healthy individuals. The reason behind this is various life-threatening complications of obesity, like cardiovascular, respiratory, gastrointestinal, endocrine, genitourinary, and musculoskeletal system diseases. Moreover, cancer also increases the mortality rate.5Haslam, D. W., & James, W. P. (2005). Obesity. Lancet (London, England), 366(9492), 1197–1209. https://doi.org/10.1016/S0140-6736(05)67483-1
Is Obesity Genetic?
Genetic factors also have an impact on obesity. According to Human Genome-Wide Association studies, more than 250 genes are associated with obesity. However, the FTO gene on chromosome number 16 has the highest risk of causing obesity.6Fall, T., & Ingelsson, E. (2014). Genome-wide association studies of obesity and metabolic syndrome. Molecular and cellular endocrinology, 382(1), 740–757. https://doi.org/10.1016/j.mce.2012.08.018
Obesity can be monogenic as well as polygenic. Monogenic obesity occurs due to a mutation in the leptin signaling pathway in your body. However, Sixty percent of obesity is polygenic, and it occurs due to the mutation in CYP27A1, TFAP2B, PARK2, IFNGR1, as well as UCP2 & UCP3- genes that are involved in uncoupling proteins in the adipose tissue.7Tirthani E, Said MS, Rehman A. Genetics and Obesity. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK573068/ As a result, the mutation causes the accumulation of fats in the adipose tissues. Therefore, it is safe to say that obesity has a genetic predisposition.
What Is The Association Between COVID And Obesity?
Obesity is a chronic condition that increases the risk of many diseases, including COVID-19. Additionally, morbidly obese individuals have a significantly higher rate of complications and risk of hospitalization from COVID-19.8People with Certain Medical Conditions. (2023, May 11). Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html
This increased morbidity is due to obesity affecting the immune system, making the body more prone to infections. Moreover, obesity decreases lung capacity and makes ventilation more difficult. Obesity also causes metabolic syndrome, which increases the risk of developing COVID-19.

How to manage Morbid Obesity?
Managing morbid obesity requires a comprehensive approach to improve overall health and effectively reduce excess weight. Here are several key strategies and interventions for managing morbid obesity:
Dietary Modifications:
Adopting a healthy and balanced diet is fundamental in managing morbid obesity. It involves reducing the consumption of carbohydrates and fats while focusing on nutrient-rich foods. A diet rich in fruits, vegetables, lean proteins, and whole grains can support weight loss and improve overall health.
Regular Physical Activity:
Regular exercise is crucial for burning excess calories and shedding extra weight. Activities such as swimming, jogging, and brisk walking are effective for increasing energy expenditure. These exercises also enhance cardiovascular fitness and muscle strength.
Avoiding Sedentary Behavior:
Reducing sedentary behavior is essential for managing morbid obesity. This includes minimizing extended periods of sitting and incorporating movement into daily routines. Simple changes like taking short walks, using standing desks, or participating in recreational activities can be beneficial.
Lifestyle Choices:
Avoiding smoking and limiting alcohol consumption is advisable for those with morbid obesity. Smoking cessation and moderating alcohol intake are not only beneficial for weight management but also for overall health and well-being.
Medical Interventions:
In some cases, medical interventions may be necessary. These options include:
Weight Loss Medication
Healthcare professionals may prescribe medications like orlistat to assist in weight management.9Ozkan Y, Aydin S, Donder E, Koca SS, Aydin S, Ozkan B, Sahin I. Effect of orlistat on the total ghrelin and leptin levels in obese patients. J Physiol Biochem. 2009 Sep;65(3):215-23. doi: 10.1007/BF03180574. PMID: 20119816. Orlistat helps with weight loss by inhibiting the absorption of dietary fats in the intestines, reducing overall calorie intake. These medications are typically considered when lifestyle modifications alone are insufficient.
Semaglutide (OZEMPIC)
Ozempic (semaglutide) is a new weight loss drug that has rapidly gained popularity for its effectiveness in treating morbid obesity. Initially approved for managing type 2 diabetes, Ozempic has demonstrated significant weight loss benefits. It functions by increasing insulin secretion, reducing glucagon release, slowing gastric emptying, and suppressing appetite, which collectively leads to substantial weight reduction. Administered as a once-weekly subcutaneous injection, Ozempic is most effective with lifestyle modifications such as a calorie-restricted diet and regular physical activity. This drug not only aids in weight loss but also offers improved glycemic control and potential cardiovascular benefits, making it a promising option for those struggling with obesity and PCOS.10Carmina, E., & Longo, R. A. (2023). Semaglutide Treatment of Excessive Body Weight in Obese PCOS Patients Unresponsive to Lifestyle Programs. Journal of Clinical Medicine, 12(18), 5921. https://doi.org/10.3390/jcm12185921
Hormonal Treatment
Hormonal treatments may be recommended for individuals with specific hormonal imbalances contributing to morbid obesity. These treatments aim to address the underlying causes.
Surgical Procedures:
For severely obese individuals who have not achieved significant weight loss through other methods, bariatric surgery may be considered.11Albaugh VL, Abumrad NN. Surgical treatment of obesity. F1000Res. 2018 May 21;7:F1000 Faculty Rev-617. doi: 10.12688/f1000research.13515.1. PMID: 29904577; PMCID: PMC5964632. The most commonly performed bariatric surgeries include:
Gastric Sleeve
This procedure involves reducing the stomach size to create a smaller, sleeve-shaped pouch.
Gastric Bypass
In gastric bypass surgery, the digestive system is rerouted to create a smaller stomach pouch and alter nutrient absorption.
Adjustable Gastric Band
An adjustable band is placed around the upper part of the stomach to restrict food intake.
Less frequently utilized is a fourth operation known as biliopancreatic diversion with a duodenal switch.
Liposuction and abdominoplasty (tummy tuck) are surgical procedures that can be used as part of the treatment plan for individuals with morbid obesity, particularly for those who have lost a significant amount of weight and are dealing with excess skin and residual fat deposits. However, it’s important to note that these procedures are not primary treatments for morbid obesity but rather adjunctive options.
Effective management of morbid obesity necessitates a personalized approach with input from healthcare providers. Lifestyle changes and non-surgical interventions should be attempted first, and surgical options are typically considered for individuals with severe obesity who have not responded adequately to other treatments. These approaches collectively work toward achieving sustainable weight loss and improved health.
Conclusion
In summary, Morbid Obesity is a chronic, life-threatening condition that occurs due to genetic as well as environmental factors. It affects almost every system of your body; therefore, it causes severe life-threatening complications, including diseases of the cardiovascular system, gastrointestinal system, musculoskeletal system, and genitourinary system. You can prevent obesity through diet, lifestyle changes, activities like exercise, swimming, jogging and cycling, etc. In addition, surgical options like gastric bypass and gastric sleeve surgery are also available for morbid obesity.
Refrences
- 1Centers for Disease Control and Prevention. (n.d.). Adult obesity facts. https://www.cdc.gov/obesity/data/adult.html
- 2Purnell, J. Q. (2023, May 4). Definitions, Classification, and Epidemiology of Obesity. Endotext – NCBI Bookshelf. https://www.ncbi.nlm.nih.gov/books/NBK279167/#
- 3Lean, M. E., Han, T. S., & Morrison, C. E. (1995). Waist circumference as a measure for indicating the need for weight management. BMJ (Clinical research ed.), 311(6998), 158–161. https://doi.org/10.1136/bmj.311.6998.158.
- 4Centers for Disease Control and Prevention. (n.d.). Obesity and Cancer. Retrieved from https://www.cdc.gov/cancer/obesity/index.htm
- 5Haslam, D. W., & James, W. P. (2005). Obesity. Lancet (London, England), 366(9492), 1197–1209. https://doi.org/10.1016/S0140-6736(05)67483-1
- 6Fall, T., & Ingelsson, E. (2014). Genome-wide association studies of obesity and metabolic syndrome. Molecular and cellular endocrinology, 382(1), 740–757. https://doi.org/10.1016/j.mce.2012.08.018
- 7Tirthani E, Said MS, Rehman A. Genetics and Obesity. [Updated 2023 Jul 31]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK573068/
- 8People with Certain Medical Conditions. (2023, May 11). Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/need-extra-precautions/people-with-medical-conditions.html
- 9Ozkan Y, Aydin S, Donder E, Koca SS, Aydin S, Ozkan B, Sahin I. Effect of orlistat on the total ghrelin and leptin levels in obese patients. J Physiol Biochem. 2009 Sep;65(3):215-23. doi: 10.1007/BF03180574. PMID: 20119816.
- 10Carmina, E., & Longo, R. A. (2023). Semaglutide Treatment of Excessive Body Weight in Obese PCOS Patients Unresponsive to Lifestyle Programs. Journal of Clinical Medicine, 12(18), 5921. https://doi.org/10.3390/jcm12185921
- 11Albaugh VL, Abumrad NN. Surgical treatment of obesity. F1000Res. 2018 May 21;7:F1000 Faculty Rev-617. doi: 10.12688/f1000research.13515.1. PMID: 29904577; PMCID: PMC5964632.

