Dacryocystitis refers to inflammation of the tear sac. It can be classified as acute or chronic and acquired or congenital. Dacryocystitis is not a contagious condition. Treatment may involve warm compresses, but sometimes antibiotics are necessary.
What Is Dacryocystitis?
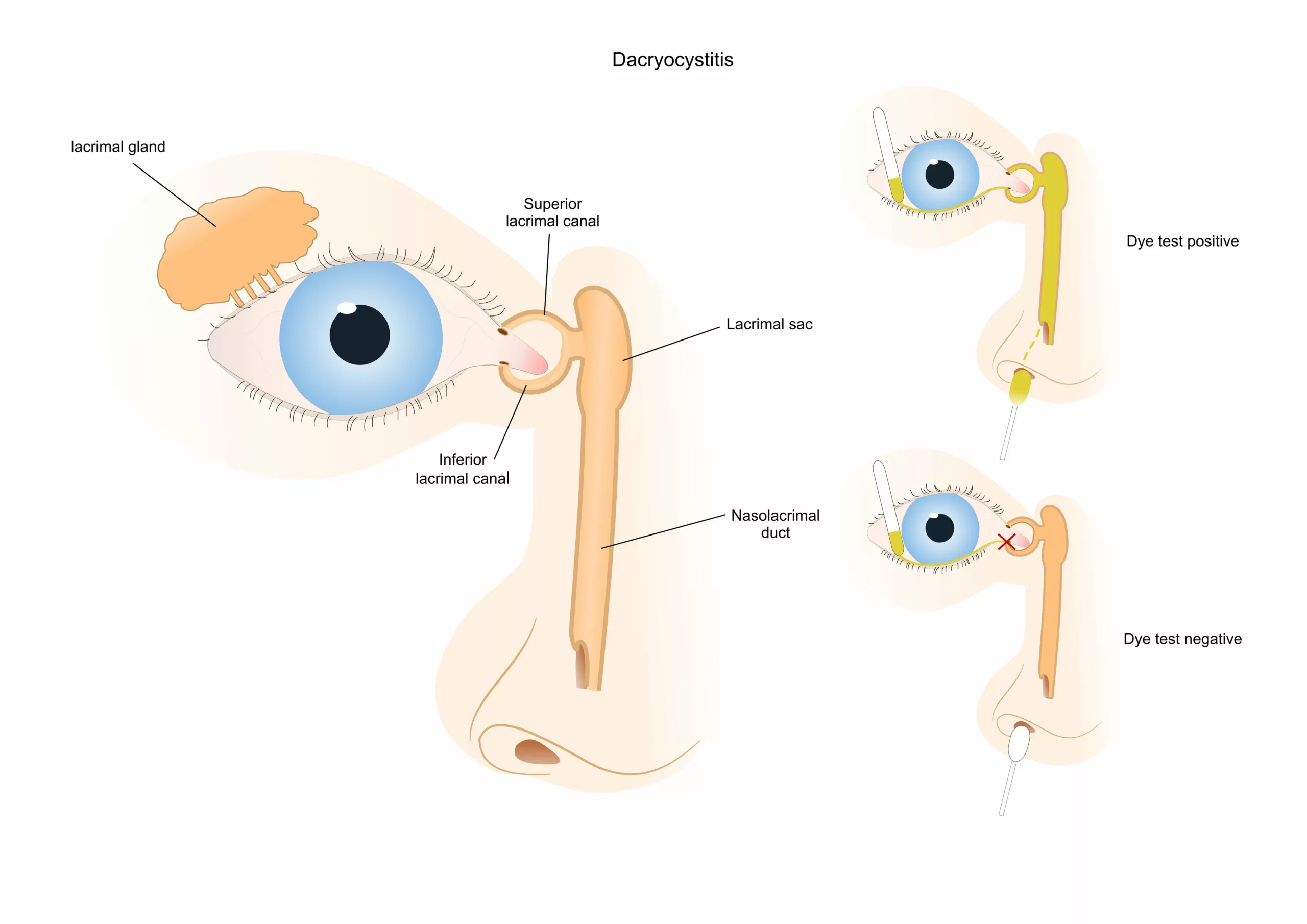
Dacryocystitis is defined by inflammation of the lacrimal sac, often caused by an obstruction in the nasolacrimal duct. This blockage results in the buildup of tears within the lacrimal sac, leading to stagnation and debris accumulation. The stagnant environment also creates an ideal breeding ground for microorganisms, potentially leading to infection and the development of the acute form of the condition.
Types Of Dacryocystitis
Dacryocystitis can be subdivided into acute and chronic dacryocystitis based on the onset of symptoms. It can also be classified according to the cause, such as congenital or acquired dacryocystitis.
Acute & Chronic Dacryocystitis
An acute infection usually causes acute dacryocystitis. It is sudden in onset and tends to resolve quickly within three months. In children, this infection is usually caused by Staph or Streptococcus species. In adults, Haemophilus or Pseudomonas may also cause Acute Dacryocystitis.
Chronic dacryocystitis develops due to persistent obstruction. Systemic disease, recurrent infections, or dacryoliths (concretions formed in the lacrimal sac) within the nasolacrimal system may cause chronic dacryocystitis. These patients may also present with chronic conjunctivitis. Common systemic diseases associated with chronic dacryocystitis include Wegener granulomatosis, sarcoidosis, and systemic lupus erythematosus.1Taylor RS, Ashurst JV. Dacryocystitis. [Updated 2023 Sep 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470565/
Congenital Dacryocysitis & Acquired Dacryocystitis
Congenital dacryocystitis occurs in approximately 1 out of 4000 births. This happens because of a blockage in the valve of Hasner. This valve is located in the distal nasolacrimal duct. Before birth, the nasolacrimal system is filled with amniotic fluid. If this fluid doesn’t come out properly after birth, it can become infected. This will happen within a few days after birth.2 Dacryocystitis – EyeWiki. Aao.org. Published February 6, 2020. https://eyewiki.aao.org/Dacryocystitis
Acquired Dacryocystitis may result from blockage caused by nose and ethmoid bone fractures. Other causes include surgeries of the nose and sinuses, especially procedures involving endoscopic and endonasal methods. Tumors of the lacrimal sac and certain medications like pilocarpine and fluorouracil may also cause the condition.
Difference Between Dacryocystitis & Dacryoadenitis
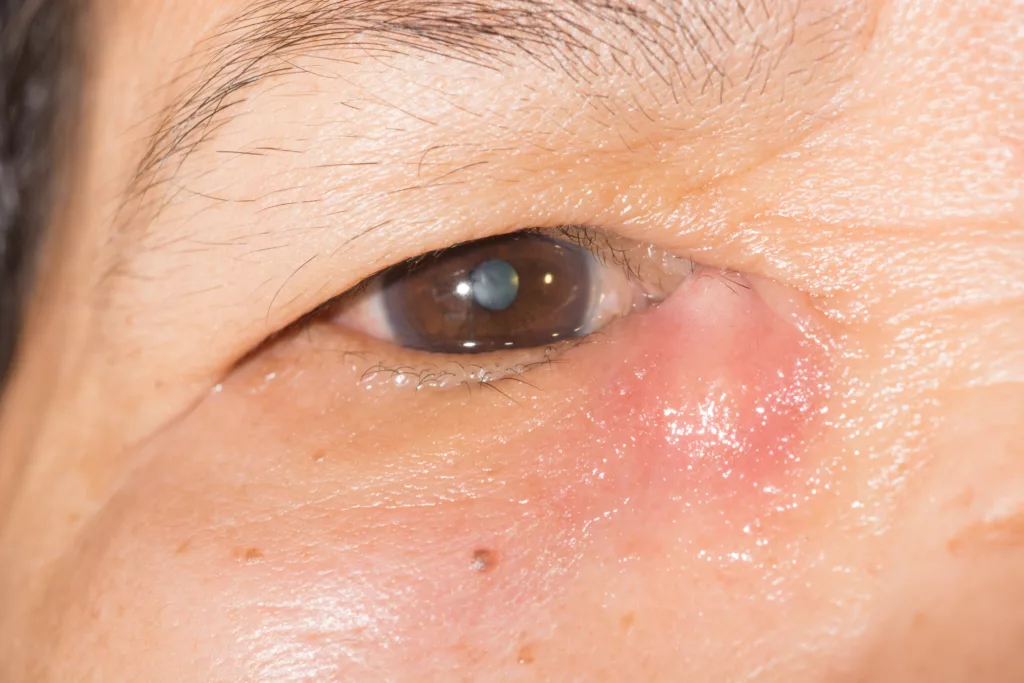
Dacryocystitis refers to inflammation of the nasolacrimal sac. It presents with symptoms like eye pain, swelling around the eye, redness or darkening of the skin, and abscesses with possible discharge (pus) in the inner corner of the eyelids.
Dacryoadenitis refers to inflammation of the lacrimal gland (tear gland). Patients with dacryoadenitis present with swelling around the upper outside corner of the eye (the lateral canthus). They often have ptosis (drooping eyelid) in the affected eye. Patients may also experience pain, watery eyes (epiphora), swollen lymph nodes near the ear, and sometimes discoloration, along with a sensation of warmth in the affected area.
How Common is Dacryocystitis?
Dacryocystitis has a bimodal distribution. It is most common just after birth or in adults after 40 years of age. Adult women are more likely to suffer from the condition.3Chen L, Fu T, Gu H, et al. Trends in dacryocystitis in China: A STROBE-compliant article. Medicine (Baltimore). 2018;97(26):e11318. doi:10.1097/MD.0000000000011318 Females are at greater risk due to a narrower duct diameter.
Causes of Dacryocystitis
Generally, dacryocystitis results from tear duct blockage, which leads to inflammation. These blockages can arise from membranes in newborns. In children and adults, dacryocystitis can have multiple causes:
- Trauma – such as broken bones and surgical procedures.
- Tumors
- Certain medications used for the treatment of Glaucoma, like pilocarpine and dorzolamide, antivirals like trifluridine, and cancer therapies like fluorouracil, docetaxel, or radioactive iodine can also lead to Dacryocystitis.
- Autoimmune conditions
- Infections, which may lead to inflammation of the nasolacrimal system.
Signs & Symptoms Of Dacryocystitis
Signs and symptoms of dacryocystitis will depend on the type. Generally, for acute dacryocystitis, symptoms include:
- Fever
- Pain, redness, and swelling around the tear sac near the inner corner of the eye
- Watery pus and discharge from the eye
- There may also be oozing pus from the puncta.
These symptoms usually last for a few hours to days. However, chronic dacryocystitis has a longer history of symptoms. The symptoms are milder, with minimal swelling and watery discharge. There may be discomfort in the eye; patients may present with conjunctivitis, and like acute dacryocystitis, pus may ooze out of the punta on the application of pressure.
How Do You Diagnose Dacryocystitis?
Physicians will take a thorough history and physical examination before diagnosing dacryocystitis. A physician may inquire about eye pain, symptoms’ onset, and discharges while taking history. They will then perform additional tests, such as
Physical Examinations
The physical examination will focus on the affected eye and surrounding areas. It may also involve measuring the size of the tear meniscus. The lacrimal sac may be palpated to reveal any tenderness or swelling. Both of these signs indicated inflammation or infection.
Fluorescein Dye Test
Healthcare providers can perform a fluorescein dye disappearance test to assess the function of the lacrimal drainage system. The test involves placing sterile dye and observing whether it drains or stagnates in the eye. If the dye hasn’t drained or remained stagnant after five minutes, then there may be a lacrimal system obstruction.4Guzek JP, Ching AS, Hoang TA, et al. Clinical and radiologic lacrimal testing in patients with epiphora. Ophthalmology. 1997;104(11):1875-1881. doi:10.1016/s0161-6420(97)30013-x
Imaging Studies & Other Tests
If an obstruction is present, healthcare providers may order imaging studies to determine the extent of the blockage. This also helps screen for underlying diseases and obstructions. For suspected structural abnormalities, the doctor may order a dacryocystography. Nasal endoscopies can help rule out nasal septal deviations. When patients exhibit symptoms such as visual alterations, fever, or signs suggestive of orbital cellulitis, healthcare providers may opt to conduct blood tests. These tests serve to delve deeper into the patient’s condition, providing valuable insights into potential systemic issues that may be contributing to their symptoms.
For chronic dacryocystitis, they may perform anti-neutrophilic and antinuclear antibody testing. These specialized tests aid in diagnosing and managing chronic inflammatory conditions, providing crucial information for effective treatment planning and monitoring.
Culture & Microbial Assay
Healthcare providers may perform tear duct massages (Crigler massages) to collect samples. The massage may release pus or liquid discharge from the lacrimal sac. The second method to obtain a sample is to disinfect the area and obtain a sample through the puncture and aspiration of the lacrimal sac.5Heichel J, Struck HG, Glien A. Diagnostik und Therapie von Tränenwegserkrankungen : Ein strukturiertes patientenzentriertes Versorgungskonzept [Diagnostics and treatment of lacrimal duct diseases : A structured patient-centred care concept]. HNO. 2018;66(10):751-759. doi:10.1007/s00106-018-0535-0 The sample can then be sent to the lab for testing to be inoculated on different culture media and processed. This can help find the causative organism and guide antibiotic therapy.
How Do You Treat Dacryocystitis?
Management of the condition generally requires treating the underlying cause. Patients can use warm compresses and perform Criggler massages to relieve inflammation. Treatments for dacryocystitis will depend on the patient’s age and include the following:
For Adults
In adults with acute dacryocystitis, treatment may include a combination of heat application with massages and systemic antibiotics (either oral or intravenous). In cases with abscesses, drainage by puncture and aspiration of the lacrimal sac is often preferred. However, this can be uncomfortable and painful for the patient. It also may not always remove enough material, leading to recurrent inflammation and complications such as fistula formation.
In acute cases, surgical interventions have traditionally been avoided due to concerns about worsening the infection.6Cahill KV, Burns JA. Management of acute dacryocystitis in adults. Ophthalmic Plast Reconstr Surg. 1993;9(1):38-42. doi:10.1097/00002341-199303000-00005 When necessary, the preferred approach usually involves a procedure known as dacryocystorhinostomy. Dacryocystorhinostomy creates a new functional pathway from the canaliculi to the nose. To create this new pathway, surgeons perform a procedure called Osteotomy, which involves cutting or reshaping the bone. Then, the nasolacrimal sac is opened up into the nose.7Ullrich K, Malhotra R, Patel BC. Dacryocystorhinostomy. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 7, 2023. Surgeons can perform the procedure using an external or endonasal approach.
Chronic dacryocystitis, on the other hand, is almost always managed surgically. Probing is accepted as first-line management in chronic cases and can be done in the outpatient setting. However, further surgical options may be necessary if symptoms persist or recur despite probing. These may include procedures such as balloon dacryoplasty, nasolacrimal intubation, and nasolacrimal stenting, each with variable first-time success rates. If these therapies fail, evaluation for more invasive procedures like percutaneous dacryocystorhinostomy (DCR) is recommended.8Taylor RS, Ashurst JV. Dacryocystitis. [Updated 2023 Sep 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470565/
For Children
In children, a more conservative approach is adopted. This is because 90% of the congenital obstructions of the nasolacrimal ducts resolve by one year of age. Conservative treatment primarily involves hydrostatic massages and twice-daily administration of bacitracin eyedrops.
The doctor may recommend early nasolacrimal intubation for patients with recurrent episodes of acute dacryocystitis or dacryocele. This procedure involves inserting a small, flexible tube called a lacrimal intubation set into the nasolacrimal duct to widen it and improve tear drainage.
Lacrimal probing and irrigation are done for patients between 12 and 18 months old with persistent blockage. Administering antibiotics before probing and irrigation has been associated with a higher success rate for the procedure. Healthcare providers reserve nasolacrimal intubation for patients aged 18 to 36 months. Finally, dacryocystorhinostomy is indicated for pediatric patients over three years old.
Complications Of Dacryocystitis
Dacrocystitis can lead to severe complications if left untreated. It can lead to preorbital and septal cellulitis. Orbital cellulitis can even damage the optic nerve, leading to visual loss.9Alsalamah AK, Alkatan HM, Al-Faky YH. Acute dacryocystitis complicated by orbital cellulitis and loss of vision: A case report and review of the literature. Int J Surg Case Rep. 2018;50:130-134. doi:10.1016/j.ijscr.2018.07.045 Moreover, congenital dacryocystitis can spread to the eye socket. This may lead to brain abscesses, meningitis, and sepsis. However, the complications are rare; dacryocystitis usually has a favorable prognosis.
Conclusion
In conclusion, dacryocystitis presents complex challenges, from acute infections to chronic inflammations, particularly affecting the lacrimal sac. Early recognition and prompt treatment, whether through conservative measures or surgical interventions tailored to the individual’s needs, are crucial in managing this condition effectively. With advances in diagnostic techniques and therapeutic options, coupled with interdisciplinary collaboration among healthcare providers, patients with dacryocystitis can receive timely and comprehensive care, ultimately improving their outcomes and quality of life.
Refrences
- 1Taylor RS, Ashurst JV. Dacryocystitis. [Updated 2023 Sep 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2023 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470565/
- 2Dacryocystitis – EyeWiki. Aao.org. Published February 6, 2020. https://eyewiki.aao.org/Dacryocystitis
- 3Chen L, Fu T, Gu H, et al. Trends in dacryocystitis in China: A STROBE-compliant article. Medicine (Baltimore). 2018;97(26):e11318. doi:10.1097/MD.0000000000011318
- 4Guzek JP, Ching AS, Hoang TA, et al. Clinical and radiologic lacrimal testing in patients with epiphora. Ophthalmology. 1997;104(11):1875-1881. doi:10.1016/s0161-6420(97)30013-x
- 5Heichel J, Struck HG, Glien A. Diagnostik und Therapie von Tränenwegserkrankungen : Ein strukturiertes patientenzentriertes Versorgungskonzept [Diagnostics and treatment of lacrimal duct diseases : A structured patient-centred care concept]. HNO. 2018;66(10):751-759. doi:10.1007/s00106-018-0535-0
- 6Cahill KV, Burns JA. Management of acute dacryocystitis in adults. Ophthalmic Plast Reconstr Surg. 1993;9(1):38-42. doi:10.1097/00002341-199303000-00005
- 7Ullrich K, Malhotra R, Patel BC. Dacryocystorhinostomy. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 7, 2023.
- 8Taylor RS, Ashurst JV. Dacryocystitis. [Updated 2023 Sep 11]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK470565/
- 9Alsalamah AK, Alkatan HM, Al-Faky YH. Acute dacryocystitis complicated by orbital cellulitis and loss of vision: A case report and review of the literature. Int J Surg Case Rep. 2018;50:130-134. doi:10.1016/j.ijscr.2018.07.045

